Learning from the Epidemiological Response to the 2014/15 Ebola Virus Disease Outbreak
- DOI
- 10.2991/jegh.k.190808.002How to use a DOI?
- Keywords
- Ebola virus; epidemiologist; outbreak response; international deployment; West Africa; FETP
- Abstract
A large international response was needed to bring the 2014/15 West African Ebola virus disease outbreak under control. This study sought to learn lessons from this epidemic to strengthen the response to future outbreaks of international significance by identifying priorities for future epidemiology training and response. Epidemiologists who were deployed to West Africa were recruited through a snowball sampling method and surveyed using an online anonymous questionnaire. Associations between demographics, training, qualifications, and role while in-country were explored alongside respondents’ experience during deployment. Of 128 responses, 105 met the inclusion criteria. Respondents originated from 25 countries worldwide, for many (62%), this was their first deployment abroad. The most common tasks carried out while deployed were surveillance, training, contact tracing, and cluster investigation. Epidemiologists would value more detailed predeployment briefings including organizational aspects of the response. Gaps in technical skills reported were mostly about geographical information systems; however, epidemiologists identified the need for those deployed in future to have greater knowledge about roles and responsibilities of organizations involved in the response, better cultural awareness, and leadership and management skills. Respondents felt that the public health community must improve the timeliness of the response in future outbreaks and strengthen collaboration and coordination between organizations.
- Copyright
- © 2019 Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
The scale and complexity of the 2014/15 West African outbreak of Ebola Virus Disease (EVD) resulted in more cases and deaths than all other previously reported cases combined [1]. The World Health Organization (WHO) deemed a coordinated international response essential to control the outbreak, declaring it a Public Health Emergency of International Concern on 8 August 2014 [2]. In September 2014, WHO warned that a lack of healthcare workers was holding back the outbreak control efforts [2,3]. Subsequently, an unprecedented response evolved, involving many organizations worldwide deploying staff to support the outbreak response [4].
It has been argued that the 2014/15 EVD epidemic was an avoidable crisis and that a timely response would have limited its scale [5]. The insufficient capacity for rapid outbreak response highlighted during this outbreak has driven agencies across the world to improve their capacity for rapid deployment and response. This enhanced ability to respond has been achieved through developing current capacity and the formation of specific rapid response teams [6]. The rapid deployment of epidemiologists to support future outbreaks should contribute to earlier control, therefore it is vital that we support the development of mechanisms to identify, and mobilize personnel with the appropriate skills and expertise when needed.
It has been recognized that field epidemiologists with international experience may be more likely to apply for deployment during outbreak situations [7]. In addition, moral and personal development reasons have been highlighted as motivators for laboratory and medical staff to volunteer for deployment [8].
Over the past 20 years, there has been a rapid growth of Field Epidemiology Training Programs (FETP) around the world and over 2550 field epidemiologists have graduated from such programs [9,10]. Factors that may affect the experience of deployment include previous experience in working in a humanitarian crisis, predeployment training, and organization deployed. Information on training that would be provided was seen as an important factor in deciding whether to apply, since predeployment training is valued [8,11].
Between 15 April and 20 May 2015, we surveyed epidemiologists who had been deployed to West Africa in support of the response to the EVD outbreak. The aim was to capture learning from the epidemiological response to the outbreak, in particular to identify common themes, to inform the planning and response to future outbreaks, also to advise future epidemiological training.
2. MATERIALS AND METHODS
We implemented a cross-sectional study. Information was collected through a tailored web-based anonymous questionnaire using Select Survey®, which was piloted with a group of epidemiologists who had been deployed to West Africa. The questionnaire sought information on demographics, qualifications and training, deployment, and included seven open-ended questions (OQ) Figure 1.
Open-ended questions included in the questionnaire.
The Faculty of Medicine and Dentistry Research Ethics Committee at the University of Bristol granted ethical approval for this work. Participants were recruited through a snowball sampling method. The survey link was first sent to key organizations and individuals known to have contributed to the response. These organizations and individuals were invited to forward the invitation to participate to any epidemiologists deployed to West Africa as part of the response to this outbreak.
Inclusion criterion was deployed to a West African country, outside of their country of residence, to work as an epidemiologist at any point during the 2014/15 EVD outbreak.
Characteristics of the respondents were described using frequencies and percentages. Responses to the open answer questions were categorized into themes, through thematic analysis carried out by two individuals. Each open answer question asked for a single issue, however, a few responses included more than one theme. In this situation, all themes were included in the analysis as it was not possible to prioritize the responses. Additionally, fourteen comments were reassigned to a more appropriate question. Country of residence was grouped to form categories to explore potential variation in the distribution of variables. Percentages, prevalence ratios, and p-values (Fisher’s exact) were calculated in Stata 13.1 (p ≤ 0.05 was considered statistically significant).
3. RESULTS
We received 128 responses, of which 105 met the inclusion criterion. Respondents were resident in 25 different countries worldwide. The number of responses by country of permanent residence ranged from 1 to 24 Figure 2.
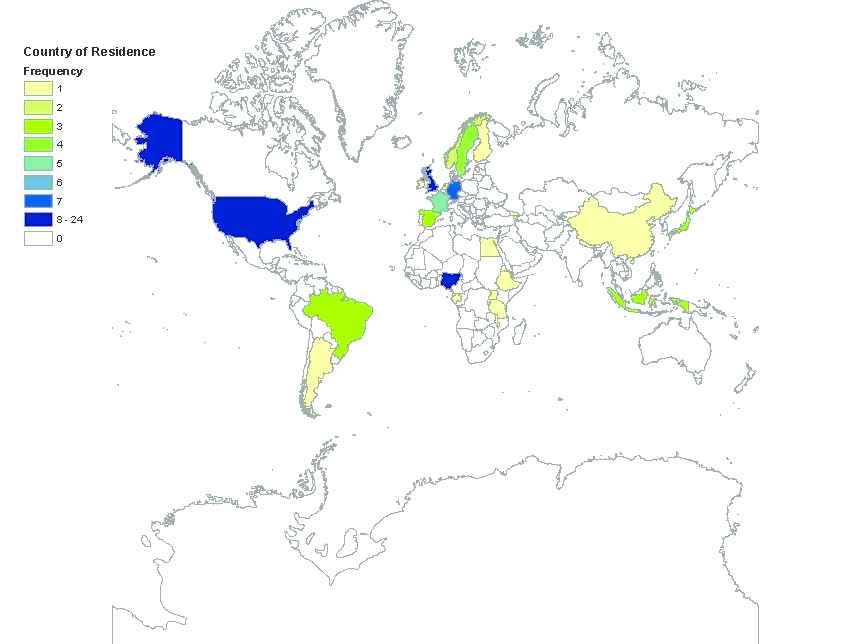
Distribution of respondents by country of residence.
Fifty (48%) respondents were male and 55 (52%) female. The gender ratio differed between grouped countries of residence; the greatest variation was between respondents from Nigeria with 89% male and 11% female. Fifty-five respondents (52%) were aged between 30 and 39 years, 25–29 years was the lowest age bracket of those deployed with 12 individuals, while 65 years and over was the highest age bracket, with just one individual.
Respondents were predominantly deployed by an international organization such as WHO or European Centre for Disease Prevention and Control (ECDC) (53%), followed by a national public or government organization, for example Public Health England or Centre for Disease Control (34%). About 10% were deployed by a nongovernmental organization such as the Red Cross or Médecins Sans Frontières and 2% were deployed by a university. The majority of respondents were routinely employed prior to deployment as epidemiologists (90%). The most common primary qualification was in medicine (48%), followed jointly by biology and veterinary science (11%), laboratory-based disciplines (6%), statistics (4%), nursing (3%), and geography (2%). Sixteen (15%) respondents reported other qualifications.
Sixty-five (62%) respondents had completed a Master’s degree in Public Health or Epidemiology. Sixty-seven (64%) respondents were completing or had completed an FETP, but there was variation by country of origin (see Table 1). The lowest percentage of respondents completing or having completed an FETP was in the UK (4/18, 22%), conversely, the UK had the highest percentage (6/18, 33%) of respondents who had completed a public health postgraduate specialist training program.
| Grouped country of residence | N | Masters in Epidemiology or Public Health n (%) | Completing or completed FETP n (%) | Postgraduate specialist training programme n (%) | PhD n (%) |
|---|---|---|---|---|---|
| UK | 18 | 12 (66.7) | 4 (22.2) | 6 (33.3) | 3 (16.7) |
| Rest of Europe | 25 | 13 (52.0) | 16 (64.0) | 7 (28.0) | 4 (16.0) |
| USA | 24 | 16 (66.7) | 19 (79.2) | 4 (16.7) | 3 (12.0) |
| Rest of America | 4 | 2 (50.0) | 3 (75.0) | 1 (25.0) | 0 |
| Nigeria | 18 | 10 (55.6) | 16 (88.9) | 2 (11.1) | 1 (5.6) |
| Rest of Africa | 6 | 4 (66.7) | 3 (50.0) | 0 | 1 (16.7) |
| Asia | 9 | 7 (77.8) | 6 (66.7) | 0 | 2 (22.2) |
| Not known | 1 | 1 (100.0) | 0 | 0 | 0 |
| Total | 105 | 65 (61.9) | 67 (63.8) | 20 (19.1) | 14 (13.2) |
Frequency of postgraduate qualifications, by grouped country of residence
The majority (65/105, 62%) of individuals reported this was their first deployment; however, there was major variation in previous experience of deployment by country of residence. The respondents from the UK were the only country group in which a majority of respondents (10/18, 56%) had been deployed to support an epidemiological mission abroad previously.
Respondents had most commonly been deployed to Sierra Leone. There was variation in the country deployed by grouped country of residence (see Table 2).
| Grouped country of residence | Sierra Leone only n (%) | Liberia only n (%) | Guinea only n (%) | Other African country n (%) | Deployed to two countries n (%) | Total N |
|---|---|---|---|---|---|---|
| UK | 13 (72.2) | 2 (11.1) | 2 (11.1) | 1 (5.6) | 0 | 18 |
| Rest of Europe | 11 (44.0) | 2 (8.0) | 10 (40.0) | 0 | 2 (8.0) | 25 |
| USA | 10 (41.7) | 4 (16.7) | 0 | 6 (25.0) | 4 (16.7) | 24 |
| Rest of America | 0 | 0 | 0 | 4 (100.0) | 0 | 4 |
| Nigeria | 6 (33.3) | 6 (33.3) | 1 (5.6) | 0 | 5 (27.8) | 18 |
| Rest of Africa | 1 (16.7) | 4 (66.7) | 0 | 0 | 1 (16.7) | 6 |
| Asia | 7 (77.8) | 1 (11.1) | 0 | 1 (11.1) | 0 | 9 |
| Not known | 1 (100.0) | 0 | 0 | 0 | 0 | 1 |
| Total | 49 (46.7) | 19 (18.1) | 13 (12.4) | 12 (11.4) | 12 (11.4) | 105 |
Country to which deployed, by grouped country of residence
There was also variation by country of residence in the length of the period of deployment. About 1–3 months was the most common period of deployment for respondents from the UK, the rest of Europe, and the USA at 67% (12/18), 80% (20/25), and 50% (12/24), respectively. However, 44% (4/9) of respondents from Asia and 42% (10/24) of respondents from the USA were deployed for 1 week to a month; conversely, 73% (13/18) of respondents from Nigeria were deployed for >3 months.
Surveillance was the most common task carried out while deployed in Sierra Leone, Liberia, and Guinea. Whereas training was the most common task carried out by those deployed to support other West African country (see Table 3).
| Tasks while deployed | Sierra Leone only n (%) | Liberia only n (%) | Guinea only n (%) | Other African country only n (%) | Deployed to two countries n (%) | Total N (%) |
|---|---|---|---|---|---|---|
| Surveillance | 36 (17.3) | 17 (21.3) | 12 (23.1) | 7 (19.4) | 12 (18.8) | 84 (19.1) |
| Contact tracing | 28 (13.5) | 11 (13.8) | 7 (13.5) | 6 (16.7) | 11 (17.2) | 63 (14.3) |
| Cluster investigation | 29 (13.9) | 13 (16.3) | 8 (15.4) | 2 (5.6) | 10 (15.6) | 62 (14.1) |
| Cluster control | 21 (10.1) | 9 (11.3) | 4 (7.7) | 1 (2.8) | 8 (12.5) | 43 (9.8) |
| Vaccine or treatment related research | 5 (2.4) | 1 (1.3) | 0 | 0 | 1 (1.6) | 7 (1.6) |
| Other research | 13 (6.3) | 2 (2.5) | 1 (1.9) | 1 (2.8) | 2 (3.1) | 19 (4.3) |
| Training | 35 (16.8) | 11 (13.8) | 9 (17.3) | 10 (27.8) | 8 (12.5) | 73 (16.6) |
| Mentoring | 22 (10.6) | 6 (7.5) | 4 (7.7) | 3 (8.3) | 8 (12.5) | 43 (9.8) |
| Evaluation | 10 (4.8) | 8 (10.0) | 5 (9.6) | 5 (13.9) | 3 (4.7) | 31 (7.1) |
| Other tasks not listed | 9 (4.3) | 2 (2.5) | 2 (3.8) | 1 (2.8) | 1 (1.6) | 15 (3.4) |
Tasks carried out while deployed, by country of deployment
4. KNOWLEDGE GAPS
The one thing that respondents most wished that they had known before their deployment (OQ1) was categorized into additional information as part of their predeployment briefing (n = 40) and organizational information (n = 26) (see Figure 3). The gaps in organizational information included (in descending order of frequency): knowledge of roles and responsibilities of organizations involved in the response, knowledge of organizational structures and an understanding of the political context, and knowledge about the arrangements for the coordination of the response. Examples of statements relating to this question are “I wish I had clearer picture (based on reality, not on declarative agreements) on who is responsible for what in the response”; “clear view of work organization (organogram and associated responsibilities and tasks)”, “The strong need to implement effective managigerial and coordination” and “Role of the political influences locally and internationally”.
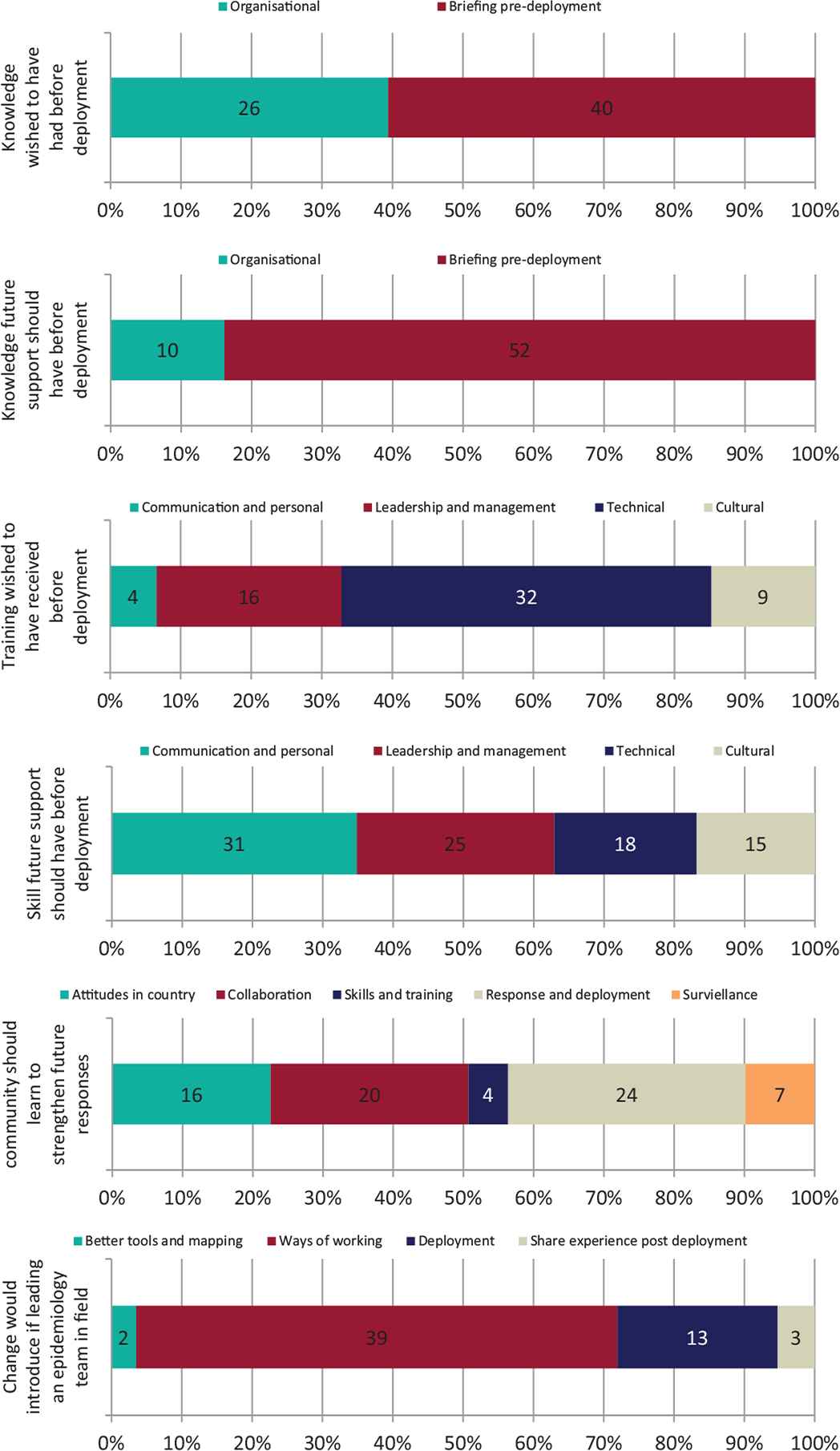
Open answer question responses overview categories.
There were knowledge gaps identified (OQ1) in the area of deployment-related information, such as information on accommodation and transport, job role-specific information, outbreak-specific information, cultural information, and better knowledge to help manage expectations. For example: “More information on specifics of the response in the country, e.g. What were people doing for case investigation, quarantine, etc.? What were protocols? Knowing this ahead of time would have saved time while in-country trying to figure it out.”
The gaps identified in response to OQ1 varied between grouped countries of residence with respondents from the USA being more likely to highlight organizational issues than respondents outside of the USA (p = 0.006).
Open-ended question 3 related to knowledge that respondents thought that future epidemiologists being deployed to support future outbreaks overseas should have. The needs identified fell into the same two main categories: additional briefing information prior to deployment (n = 52) and information on organizations taking part in the response such as roles and responsibilities (n = 10). Predeployment briefing needs identified included cultural information, information to allow better management of expectations, job role-specific information, clarity about personal skills required, and learning from the experience of those who have been previously deployed.
5. SKILLS GAPS
When asked what skills they most wished they had possessed prior to deployment (OQ2), responses were grouped into technical skills (n = 32), leadership and management skills (n = 16), cultural awareness (n = 9), and communication skills or other personal attributes (n = 4) (see Figure 3). The key technical skills identified were mapping software, data analysis/analytical software, for example, “Skills in managing complex data sets - merging, de-duplication techniques etc”, and infection control (n = 7). Cultural awareness needs identified included greater understanding of the cultural context (n = 4) and training in the native language (n = 3), for example, “More specific anthropological, sociological background information and local culture/mannerisms”. Leadership and management skill gaps reported included management training and teamwork skills, for example, “I wish I had been trained personal management in order to lead more effectively the team of local public health workers”.
Responses to this question varied by grouped countries of residence; this was particularly the case for Nigeria, which had higher numbers of individuals reporting gaps in technical skills (8/18, 44.44%). There was no difference in the needs identified in those who had completed an FETP compared to those who had not; 27% who had completed FETP reporting a requirement for improved technical skills compared to 29% for those who had not 7% of respondents who had completed FETP reported requirement for information related to cultural awareness compared with 11% of those with no FETP and 15% with FETP reported desire for improved leadership and management skills compared with 15% who had not.
Respondents highlighted the following skill attributes that epidemiologists deployed in future should (OQ4) possess: communication and other interpersonal skills (n = 31), followed by leadership and management skills (n = 25), technical skills (n = 18), and cultural awareness (n = 15). Interpersonal skills highlighted were, flexibility, resilience, and empathy, for example, “Flexibility to take up other functions should there be need”. Leadership and management skills identified as important for future deployments were: diplomacy, networking, management training, and teamwork skills, for example, “Effective communication skills - the importance of negotiation skills and working with people from different cultures and background and with governments”. Priorities in relation to technical skills included data analysis and mapping, for example, “Data base management for data entry, data management and data analysis, including GIS tools and training capacities”. Finally, cultural knowledge and skills highlighted were cultural awareness, intercultural relations, and community engagement: “Epidemiologists must have the ability to communicate with people from a very different culture of our countries. This is fundamental to exchange experiences and information”.
6. STRENGTHENING RESPONSE TO FUTURE OUTBREAKS
Respondents thought the public health community should strengthen the response to future outbreaks (OQ5) in a number of ways. First, in timeliness of response and human resources aspects, to allow us to mount response of this scale and duration (n = 24). Second, there should be greater collaboration and coordination between countries and organizations (n = 20). Additionally, there should be changes to attitudes and ways of working while in country to enable greater strengthening of local systems (n = 16) and improvements in surveillance (n = 7). A minority of people identified epidemiological skills and training as a priority to strengthen the response to future outbreaks (n = 4). Recommendations to improve response and deployment included the need for a more rapid response and development of a rapid response network:
“I think better mechanisms need to be in place to identify emerging problems quickly to ensure that resources are deployed at an earlier stage and in large quantities to stop the escalation of outbreaks.”
“There is a need to build a transnational response network that can be rapidly activated and can rise above partner politics to harmonize data collection, response strategies, etc. WHO GOARN was originally intended to do this but it has faced challenges of bureaucratic procedures, lack of funding, continued politics, etc.”
Key points highlighted in relation to working together were the need for interorganizational collaboration and sharing experiences in order to learn from them:
“Response to support future outbreaks of international importance should involve proper coordination of health organizations involved in the response. Parallel activities and duplication of efforts should be avoided as much as possible” and “Disseminate mission reports to the teams coming after/ proper handovers.”
Changes required to attitudes and ways of working while in country centered on the need for in-country involvement and development, and cultural respect:
“Strengthen health care systems in a sustainable way to have a system in place that can detect, mitigate and respond to outbreaks.”
“I think the importance of understanding the local culture and traditions is really essential. When hearing the stories from the field, I think the role of socio-anthropologists is important!”
7. CHANGES THAT SHOULD BE INTRODUCED
Improvements to ways of working (n = 39) were commonly cited as the key change that epidemiologists would introduce if leading an epidemiological team onsite (OQ6). These mainly related to the importance of communication, coordination and collaboration, and clarity of roles and responsibilities:
“Listen to the problems your team is facing on the ground and cooperate with as many other actors doing the same tasks on the ground to avoid duplications!”
“I would institute a clear delegation of roles from the beginning and ensure there is a regular time/space to get all partners on the same page.”
Changes to deployments were also highlighted, specifically the need for longer deployments and more adequate handover periods:
“Provide an archive of work done in the past months, some sort of induction pack including an overview of work/organizations/flows and take the time to explain all so new epi’s can start as quickly as possible.”
8. DISCUSSION
This study is the first to consolidate the experience from epidemiologists deployed as part of the response to the major EVD outbreak in West Africa. The need to learn from this outbreak has been highlighted by Heymann et al. [12]. As there is no central register of epidemiologists deployed as part of the response to outbreaks, we relied on professional networks and connections to identify participants for this study. Our survey demonstrates the large number of countries that were involved, with responses from epidemiologists from 24 countries. Interestingly, the consistency in the feedback we received was remarkable despite some variation by country groups. The key themes also ran throughout the various questions and were frequently repeated suggesting that these are real issues that should be improved.
Respondents were generally well trained, reporting few gaps in basic epidemiological skills but identifying a need for leadership training and greater cultural awareness. Predeployment training is generally valued [8]. None of the respondents mentioned a need for greater knowledge about EVD, but we identified a need for better information surrounding deployment and on organizational aspects of the response including roles and responsibilities. This is consistent with a study of staff deployed through Médecins Sans Frontières (MSF) that also identified the need for training to improve risk perception among healthcare workers [13].
Good technical epidemiological skills are necessary but not sufficient to perform effectively in an environment as complex as a large multiagency response to a public health emergency. Training of epidemiologists should also include leadership and communication skills. This needs to be met through formal training programs (technical skills in each area of practice are necessary but not sufficient to effectively influence population health). Being able to manage the context is key to a successful response and requires active engagement with communities in order to understand their values and perceptions [14].
The need for skills in working with communities and greater cultural awareness were also identified through this study. Respondents highlighted the importance of briefing to increase understanding the sociological and anthropological background specifically of the country of deployment. Social mobilization and local capacity building are vital for a successful outbreak response, this is also key in developing community trust and engagement.
Global health leaders have reflected on lessons to strengthen the response to future public health emergencies [5,12]. Deployed epidemiologists concurred in the need to develop rapid response networks and consider deployments over a longer period of time. The need to improve communication, coordination, and collaboration between organizations, government officials, regions, and countries was seen as key to strengthen the response to future outbreaks.
Rexroth et al. [7] found that clear job descriptions and improved preparation and training efforts would enhance willingness to apply for EVD response missions. Our study supports these findings, which suggest that these factors are also important to those who have been deployed.
We demonstrated the important contribution of FETPs to the global public health capacity. Rexroth et al. [7] found that those with FETP training and more international experience were more likely to apply for deployment. We found that nearly two-thirds of those deployed had completed or were completing an FETP. Most respondents were from countries with access to an FETP, however, we did not find any statistical differences in needs identified in those who had previous deployment experience, or had FETP, compared with those who had not. FETPs are making an important contribution to global health security and the graduates are often taking leadership positions [15] but the importance of ensuring that the curricula of these programs include leadership and management skills was highlighted by this study.
There were several limitations. There was no international log of staff deployed to support the response, and owing to the scale and number of organizations involved in the outbreak it was not possible to identify all the deployed epidemiologists, to invite them to participate in the study, or to assess the response rate. Some of the comments were ambiguous and it is possible that some may have been misinterpreted. This study focused on the experience of epidemiologists. A larger number of clinical and laboratory staff were also deployed and their experiences may well have been different.
The need for rapid deployment of staff to support the response to outbreaks of international significance, reported by the participants in this study, has been identified by governments and international institutions [16,17]. This research examined in detail the experiences of epidemiologists who were deployed in the 2014/15 EVD outbreak. We conclude three key actions should be taken to strengthen future outbreak responses. First, a central register of epidemiologists deployed during an outbreak would aid a coordinated response and allow rapid dissemination of information.
Second, predeployment training should ensure that epidemiologists have full information surrounding their deployment including outbreak-specific, cultural, and practical deployment information. In addition to technical skills, deploying organizations, FETPs, and specialist training courses should ensure that epidemiologists are trained in both leadership and personal skills. This training may take place in the format of a combination of organization-provided formal training and online massive open online courses.
Finally, the epidemiological response would benefit from being led by an in-country epidemiologist who would be vital in aiding the understanding of and tailoring the response to the local anthropological and sociological context. This would also build community trust and support social mobilization.
CONFLICTS OF INTEREST
Maya Holding, Chikwe Ihekweazu, James MacNaughton Stuart and Isabel Oliver have no financial, professional, or personal interests with other people or organizations that could inappropriately influence or bias the work described in this article.
AUTHOR CONTRIBUTIONS
I.O., C.I. and J.M.S. study conceptualization, methodology and supervision. I.O. and M.H. project administration, investigation, data curation, formal analysis and writing (original draft). All authors writing (review & editing).
FUNDING
The study is funded by the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Evaluation of Interventions, University of Bristol, in partnership with Public Health England. The views expressed are those of the authors and not necessarily those of the National Health Service, the NIHR, the Department of Health or Public Health England. We extend our gratitude to all of the participants who took part in this study.
ACKNOWLEDGMENTS
We would like to thank all the epidemiologists who participated in the study and helped share invitation to participate with their colleagues. We also thank colleagues from deploying organizations who also helped disseminate the invitation including: Dionisio Herrera and Jonas Brant from TEPHINET, Ute Rexroth – RKI, Sam Bracebridge from the UK FETP, Kostas Danis from ECDC’s EPIET Programme, Andreas Gilsdorf from RKI, Katharina Alpers from the German FETP, and Iro Evlampidou from MSF. We would also like to thank Professor David Heyman for his advice and support.
REFERENCES
Cite this article
TY - JOUR AU - Maya Holding AU - Chikwe Ihekweazu AU - James MacNaughton Stuart AU - Isabel Oliver PY - 2019 DA - 2019/08/22 TI - Learning from the Epidemiological Response to the 2014/15 Ebola Virus Disease Outbreak JO - Journal of Epidemiology and Global Health SP - 169 EP - 175 VL - 9 IS - 3 SN - 2210-6014 UR - https://doi.org/10.2991/jegh.k.190808.002 DO - 10.2991/jegh.k.190808.002 ID - Holding2019 ER -
