Incidence and Causes of Perinatal Mortality in Georgia
- DOI
- 10.2991/jegh.k.190818.001How to use a DOI?
- Keywords
- Birth registry; perinatal mortality; stillbirth; early neonatal death; cause of death
- Abstract
Georgia has one of the highest perinatal mortality rates (i.e., stillbirths and early neonatal deaths combined) in Europe. The Georgian Birth Registry was started in 2016 to provide data for preventive measures of maternal and child health. In this study, we aim to determine the incidence of perinatal mortality, assess the distribution of stillbirths and early neonatal deaths, and to determine the major causes of perinatal mortality in Georgia. Data sources were the Georgian Birth Registry and the vital registration system for the year 2017. Causes of early neonatal deaths were assigned into five categories, using the Wigglesworth classification with the Neonatal and Intrauterine deaths Classification according to Etiology modification. The study used descriptive statistics only, specifically counts, means, proportions, and rates, using the statistical software STATA version 15.0. (StataCorp, College Station, TX, USA). In 2017, 489 stillbirths and 238 early neonatal deaths were recorded, resulting in a perinatal mortality rate of 13.6 per 1000 births. About 80% of stillbirths had an unknown cause of death. The majority of stillbirths occurred before the start of labor (85%), and almost one-third were delivered by caesarean section (28%). Prematurity (58%) and congenital malformations (23%) were the main causes of early neonatal deaths, and 70% of early neonatal deaths occurred after the first day of life. The perinatal mortality rate in Georgia remained high in 2017. The major causes of early neonatal deaths were comparable to those of many high-income countries. Contrary to global data, most early neonatal deaths occurred after the first day of life.
- Copyright
- © 2019 Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Significant improvement in child survival has been achieved worldwide over the past 25 years. The mortality rate for children under the age of 5 years decreased from 91 deaths per 1000 livebirths in 1990 to 43 per 1000 in 2015 [1,2]. Death during the first month of life (the neonatal period) accounts for around 45% of mortality among children under the age of 5 years. Of those deaths, the majority (≈75%) occurs during the first 7 days of life (the early neonatal period) [3–5], and >50% occur during the first 24 hours [3,6,7]. Thus, the early neonatal period is the most critical time for an infant [2]. Since 2000, stillbirth rates have decreased by 25% globally [8], but there are still large disparities between countries [9].
The combined measure of stillbirths and early neonatal deaths (ENDs) comprises perinatal mortality (PM) [10]. Stillbirth is defined as the delivery of a fetus born with no signs of life. However, the definition varies across countries by gestational age and birthweight, which complicates international comparisons [11]. Georgian national guidelines define stillbirth as a fetus born with no sign of life at 22 completed gestational weeks or more, or a birthweight of >500 g, if the gestational age is unknown.
The causes of PM are numerous and vary according to the health status of the mother and access to antenatal care. About 99% of PM occurs in low- and middle-income countries [12]. In areas where pregnant women have access to quality healthcare services, congenital malformations, preterm birth, and intrauterine growth restriction are the leading causes of PM. In areas with low healthcare service coverage, the main causes of PM are asphyxia, neonatal tetanus, and infections [13]. Comparing specific causes of stillbirth is a challenge as a universal worldwide classification of causes of stillbirth is missing [11,14,15].
Georgia is a lower middle-income country with 3,729,600 inhabitants and has one of the highest PM rates in Europe [16–18]. In 2016, the fertility rate was 2.24, and the total birth rate was 15.2 per 1000 total population. Since 2001, the rate of stillbirths has decreased by 36%, but then stagnated, reaching 9.8 per 1000 total births in 2016 [17]. In 2016, the neonatal mortality rate was 6.3 and the END rate was 4.1 per 1000 livebirths, a slight increase from 3.8 in 2015. By the end of 2030, Georgia aims to reduce neonatal mortality to 5 per 1000 livebirths and the stillborn rate to 6.8 per 1000 total births [19]. To reach these goals, it is crucial to investigate the causes and characteristics of stillbirths and ENDs.
Until 2017, all births and deaths in Georgia were registered in a vital registration system (VRS) administered by the Ministry of Justice. In 2017, this responsibility was transferred to the National Centre for Disease Control and Public Health (NCDC). In 2016, the Georgian Birth Registry (GBR) was established, a digital medical birth registry with national coverage. Maternity homes are obliged to notify the Ministry of Health, the NCDC, and the GBR of all stillbirths and neonatal deaths within 24 h. Details on the implementation of the GBR are described elsewhere [20]. This study aims to determine the incidence of PM, assess the distribution of stillbirths and ENDs, and determine the major causes of PM in Georgia in 2017.
2. MATERIALS AND METHODS
2.1. Study Population
We extracted all cases of PM reported in the GBR and VRS in 2017. Information from the two databases was merged by the unique personal identification numbers of newborns and mothers. Any additional information identified in the VRS was used as supplemental data. In total, 52,228 mothers and 52,961 newborns were registered in the GBR in 2017. This corresponds to 98.5% of the newborns registered in the VRS. We excluded mothers with parity >15 (n = 14) and aged <13 or >53 years (n = 2), as well as newborns with a gestational age >43 weeks (n = 2) and a birthweight <100 g (n = 30), (gestational age was known for all newborns, but we excluded those with biologically implausible values). Twin births were included in the study for description of all PM cases in Georgia. Thus, the final study population included 52,180 mothers and 52,913 newborns, of which 489 were registered as stillbirths (gestational age ≥22 weeks) and 148 as ENDs. Sixty-six additional ENDs were identified in the VRS as newborns who die at home or after transfer to another hospital were not be registered as PM in the GBR. Thus, the total number of cases of PM was 729 in 2017. When considering causes of death for stillbirths and ENDs, we excluded ENDs with missing personal identification number (n = 24), as they could not be merged with GBR data. As the VRS registers all births and deaths in the country, we validated the PM cases through the VRS using maternal and personal identification number. The gestational age variable at delivery was validated using self-reported last menstrual period and gestational age at different antenatal care visits throughout pregnancy.
2.2. Study Setting
In Georgia, the majority of pregnant women use antenatal care services and 81% attend at least four visits [16]. Almost all (99.8%) give birth at government-approved medical centers assisted by gynecologists (of which there are 50 per 100,000 population) [16]. Pregnant women may attend four antenatal care visits free of charge under the national universal health coverage program. In 2016, >270 antenatal care centers and maternity hospitals provided services and reported to the GBR [16]. The doctors or other trained medical personnel in the maternity wards and antenatal care centers feed information on each pregnancy, delivery and newborn in the GBR.
2.3. Assigning Causes of Death
The GBR and VRS register causes of death according to the International Statistical Classification of Death and Related Health Problems 10th revision (ICD-10). However, whereas in the GBR, there is no limit either on the number of causes of death that can be registered or on any of order of events; the VRS defines primary cause and up to three underlying causes of death. Moreover, only the GBR provides cause of death for stillbirths as these causes are not registered in the VRS. Therefore, GBR was the primary source for all stillbirth causes of death. For ENDs, we compared the ICD-10 codes for causes of death in the GBR with those in the VRS and found 90% complete agreement. However, in 10% of cases, the VRS was either more comprehensive, or included the ICD-10 code for congenital malformation. Therefore, if newborns had a lethal congenital malformation in the VRS or in the GBR, they were assigned to the congenital malformation group.
When assigning a primary cause of death to ENDs, we used the Wigglesworth classification with the Neonatal and Intrauterine deaths Classification according to Etiology modification [21,22], which is based on birthweight, gestational age, Apgar score after 5 min, presence of lethal congenital malformation, causes of death (extracted from the GBR and VRS), and the underlying causes of death (extracted from the VRS). All recorded causes of death for each END case were listed together with the other aforementioned variables in order to assign one of the following causes of death: preterm delivery, congenital malformations, birth asphyxia, infection, and others. Appendix 1 summarizes criteria for assigning case-specific cause of death.
2.4. Statistical Analysis
Descriptive statistics were used for continuous variables as means and for categorical and dichotomous variables as percentages. The data were analyzed using the statistical software STATA version 15.0 (StataCorp, College Station, TX, USA).
2.5. Ethical Consideration
The NCDC Institutional Review Board revised and approved the study protocol (IRB # 2017-010 31.03.2017). Moreover, the Regional Committee for Medical and Health Research Ethics, North Norway, approved the use of the data from the GBR for research purposes (2017/404/REK Nord) [20].
3. RESULTS
In 2017, the PM rate was 13.6 per 1000 total births, and stillborn and END rates were 9.1 per 1000 total births and 4.5 per 1000 livebirths, respectively. The ratio of stillborn to ENDs was 2.1, and the proportion of ENDs to total number of neonatal deaths was 0.66. The majority of stillbirths (415, ≈85%) died antepartum, whereas only 45 (9%) were reported as intrapartum stillbirths. The remaining stillbirths (6%) had an unknown time of death. Of 214 ENDs, 64 (≈30%) died within the first 24 h, 65 (30%) between 24 and 72 h, and 85 (≈40%) between 73 and 168 h. The majority of stillbirths and ENDs occurred among extremely preterm newborns (gestational age 22–27 weeks), whereas 23% of stillbirths and 17% of ENDs were born at term (Table 1).
| GA, weeks | Stillbirths, n (%) | ENDs, n (%) | PM, n (%) | Total births, n (%) |
|---|---|---|---|---|
| 22–27 | 189 (38.6) | 82 (38.3) | 271 (38.6) | 545 (1) |
| 28–31 | 87 (17.8) | 67 (31.3) | 154 (21.9) | 559 (1.1) |
| 32–36 | 99 (20.3) | 29 (13.6) | 128 (18.2) | 3511 (6.6) |
| ≥37 | 114 (23.3) | 36 (16.8) | 150 (21.3) | 48,298 (91.3) |
| All | 489 | 214 | 703 | 52,913 |
Number of stillbirths, early neonatal deaths (ENDs), perinatal mortality (PM) cases, and total births in Georgia in 2017 by gestational age (GA)
Mean gestational age and birthweight were 30.6 weeks and 1569 g in stillbirths, and 29.9 weeks and 1490 g among ENDs, which was significantly lower than the values in livebirths (38.6 weeks; 3264 g). In all, 28% of stillbirths and 58% of ENDs were delivered by caesarean section. Furthermore, 2.3% of stillbirths and 23.0% ENDs were diagnosed with congenital malformations, which was significantly higher than that in livebirths (0.4%).
The majority of stillbirths were registered with an unknown cause of death (80%). The most commonly reported causes of death for stillbirths were maternal conditions (7.8%) and complications of the placenta and the umbilical cord (5.2%). Congenital malformations were registered in 2.6% of stillbirths. There was no missing information on the cause of death for ENDs. The leading cause of death in this group was preterm delivery (58%), followed by congenital malformations (23%), birth asphyxia (7%), and infections (7%). However, the cause of death for ENDs changes by gestational age, with preterm delivery being most common (89%) cause at a gestational age of 22–27 weeks, whereas congenital malformation was the leading cause of death after 32 weeks of gestational age (Table 2).
| Total ENDs, n = 214, n (%) | GA = 22–27, n = 82, n (%) | GA = 28–31, n = 67, n (%) | GA = 32–36, n = 29, n (%) | GA ≥ 37, n = 36, n (%) | |
|---|---|---|---|---|---|
| Preterm delivery | 123 (58) | 72 (88) | 48 (72) | 3 (10) | 0 |
| Congenital malformation | 50 (23) | 9 (11) | 14 (21) | 13 (45) | 14 (39) |
| Birth asphyxia | 15 (7) | 1 (1) | 3 (4) | 5 (17) | 6 (17) |
| Infection | 15 (7) | 0 | 2 (3) | 6 (21) | 7 (19) |
| Other | 11 (5) | 0 | 0 | 2 (7) | 9 (25) |
Causes of early neonatal death (END) according to Wigglesworth classification with Neonatal and Intrauterine deaths Classification according to Etiology modification stratified by gestational age (GA)
4. DISCUSSION
This study confirms that the PM rate (13.6 per 1000 births in 2017) in Georgia is higher relative to most other European countries, except for Armenia [18]. In 2015, the World Health Organization (WHO) reports an average PM rate of 8.9 per 1000 total births in Europe; in the Commonwealth of Independent States the value is 11; in members of the European Union it is 6.5; and in the Nordic countries it is 5 (Figure 1) [18]. The differences in stillbirth rates are much greater than those in END rates. Consequently, stillbirths contribute much more to the PM rate in Georgia than in the WHO European region.
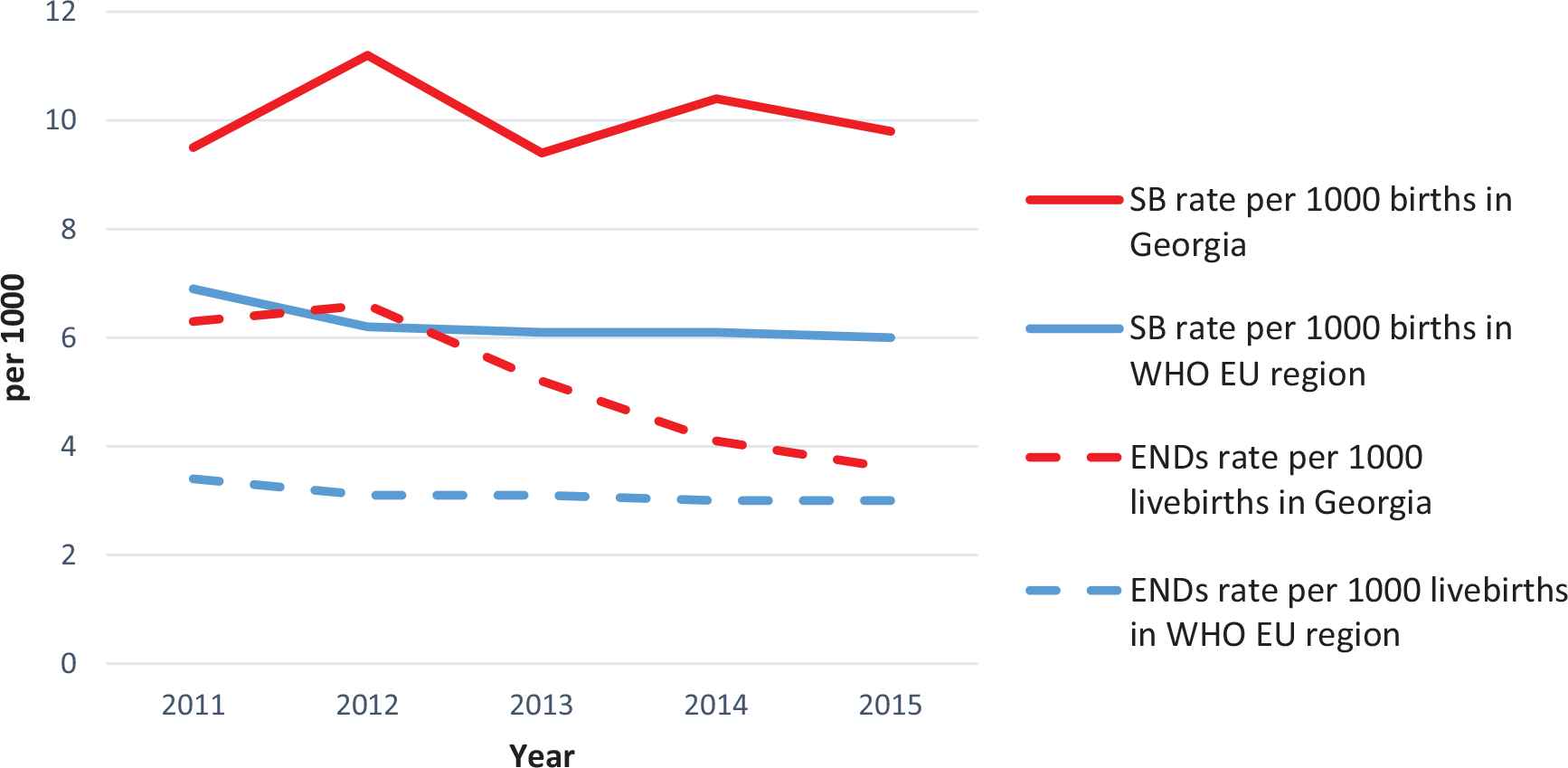
The rates of stillbirth (SB) and early neonatal deaths (ENDs) in Georgia and in World Health Organization European (WHO EU) region.
An important finding in the present study is that 70% of ENDs died after the first 24 h of life. This is very different to what was recently reported worldwide, where the majority (50–65%) of newborns die within the first 24 h of life, and the number of newborn deaths decrease with time since birth [3,7,23]. In addition, the proportion of stillbirths delivered by caesarean section was quite high in our study (≈28%), although national guidelines recommend vaginal delivery in these cases. Together these findings may indicate misclassification of ENDs as stillbirths.
The WHO published country-specific, regional and global estimates based on the different countries’ level of development, and Georgia was estimated to have a ratio of stillborn to ENDs of 1.2 [24]. However, the data from the GBR suggest that this ratio is almost twice that high, which again may indicate misclassification of ENDs as stillbirths. Furthermore, the ratio of ENDs to total neonatal deaths was 0.66 for Georgia in 2017, and the average value for Western European countries was 0.77, with few values below 0.7 [2], which suggests that the proportion of ENDs in the PM rate is lower than expected.
In high-income countries, stillbirth rates vary from 1.3 to 8.8 per 1000 total births, clearly indicating the potential for prevention in Georgia having a stillbirth rate 9.1 per 1000 births. Only four countries (Greece, Hungary, Portugal, and the United Kingdom) in Europe use a different definition of stillbirth (fetus born with no sign of life after 24 weeks of gestation). Thus, data from all other European countries are directly comparable to ours.
Previous studies have shown that more than one-third of all stillbirths occur during labor [8,24], and that intrapartum stillbirths are more common in low-income countries. Our results are not in line with these findings, as intrapartum deaths comprised only 9% of stillbirths. This finding also supports the idea about misclassification of intrapartum deaths and ENDs as stillbirths, and in addition may suggest disparities in quality of obstetric practice.
Our results show that 80% of stillbirths were registered with an unknown cause of death. Compared with other countries, this proportion is high. Indeed, previous studies reported an unknown cause of death in 32% of stillbirths in high-income countries and 43% in middle-income countries [25–27]. Possible explanations may be the high proportion of reported antepartum stillbirths (85%), incomplete input of information into the GBR about stillbirths, and the fact that few autopsies are done in Georgia as autopsy is not required by law.
In line with previous studies, preterm delivery (58%) and congenital malformations (23%) were the leading causes of ENDs in Georgia [3,21,26,28]. Whereas preterm mortality was most common at low gestational ages, the proportion of congenital malformation increased with increasing gestational age and was the most frequently occurring cause of death among ENDs born at a gestational age of 32–36 weeks, as reported by others [29,30]. It is noteworthy that the prevalence of congenital malformation among newborns who survived beyond the seventh day of life was very low (0.4%) compared with Norway (3.7%) [31]. As nonlethal malformations detected after hospital discharge are not added to the GBR, the incidence of congenital malformations is low.
Perinatal mortality and stillborn rates are higher in Georgia than in most high-income countries, but the leading causes of ENDs were similar. In low- and middle-income countries, 25% of ENDs are usually attributable to asphyxia, whereas in Georgia, asphyxia was attributed to only 7% of ENDs [3,32]. The low proportion of ENDs attributable to asphyxia also support the notion that some ENDs may be classified as stillbirths. Other studies have also confirmed that ENDs are often misclassified as stillbirths, or are underreported in low-income countries [3]. In fact, disparities in the time of death for ENDs, causes of death for both stillbirths and ENDs, and stillborn to END ratios in this study may be explained by misclassification of asphyxiated ENDs as stillbirths. This practice of reporting has been demonstrated previously [33,34]. Such misclassification increases the stillbirth rate, decreases the END rate, and changes the prevalence of causes of death in these groups. This possible selective reporting bias needs to be addressed in a validation study and in qualitative interviews with obstetric/pediatric professionals at different care levels in the Georgian healthcare system.
This study covers 98% of all officially reported PM cases in 2017, which is representative sample for Georgia. Another strength was the opportunity to merge the data from the GBR with that of the VRS, thereby validating reported cases across two independent reporting systems. Moreover, individual-level variables for each case were compared in the GBR and VRS to improve the completeness of reporting, validity of variables, and provide data for revision/defining underlying causes of death.
Nevertheless, the information in the GBR and VRS was not validated against medical records, which is a limitation. In addition, neither autopsy data nor placental histological examination were available, as these examinations are not routinely performed in Georgia; this complicates any search for the exact cause of death. The data to the GBR was transferred from medical files/records by the medical or administrative personnel, although the majority of them were properly trained, accidental misclassification could have occurred.
Future investigations of possible misclassification of ENDs as stillbirths are vital. Routine placental examinations and autopsies are recommended to identify causes of death, especially for those stillbirths who were delivered by caesarean section. More attention should also be given to birth asphyxia combined with intrapartum stillbirths, which is the main cause of death among children under 5 years of age, and which is largely invisible in healthcare policies [35]. Therefore, precise information about time of death and causes of PM will make it possible to detect knowledge gaps and provide data for further interventions.
5. CONCLUSION
Georgia has one of the highest PM rates (13.6 per 1000 births in 2017) in Europe. About 80% of stillbirths had an unknown cause of death, whereas the main causes of ENDs were preterm delivery and congenital malformations. Time of death for both stillbirths and ENDs differed from international data, which requires attention to details and integrity from the health personnel reporting to the GBR and VRS.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHOR CONTRIBUTIONS
T.M. coordinated data collection, performed statistical analysis, and drafted the first manuscript and revised it based on other authors’ comments. C.R. conceptualized and designed data collection instruments, created the theoretical framework for the analysis, and critically reviewed the manuscript. F.E.S. conceptualized and oversaw the study, and critically reviewed the manuscript. N.K. designed the study, and critically reviewed the manuscript. E.E.A. conceptualized, designed, and oversaw the study, and critically reviewed the manuscript. All authors contributed to the interpretation of the data, reviewed the draft of manuscript, and approved the final version submitted for publication.
FUNDING
The project was fully funded by the Norwegian Centre for International Cooperation in Education.
ACKNOWLEDGMENTS
Not applicable.
ABBREVIATIONS
- PM,
perinatal mortality;
- END,
early neonatal death;
- GBR,
Georgian Birth Registry;
- VRS,
vital registration system;
- NCDC,
National Centre for Disease Control and Public Health;
- ICD-10,
International Statistical Classification of Death and Related Health Problems 10th revision;
- CS,
caesarean section;
- WHO,
World Health Organization.
ETHICAL APPROVAL
The NCDC Institutional Review Board - protocol (IRB # 2017-010 31.03.2017). Regional Committee for Medical and Health Research Ethics of Northern Norway – approved the use of data from GBR for research purposes (2017/404/REK Nord).
APPENDIX 1
| Congenital malformation | Lethal congenital malformation (ICD-10 codes: Q00–Q05, Q20–Q25 (most common), Q33, Q39, Q41, Q42, Q61, Q74–Q79, and Q87–Q89). |
| Birth asphyxia | Birth asphyxia and GA > 27 weeks or weight > 1000 g Ischemic encephalopathy Apgar score < 7 |
| Prematurity | Respiratory distress syndrome and GA < 37 weeks Birth asphyxia and GA < 27 weeks or weight < 1000 g Infection with GA < 33 weeks |
| Infection | Infection and GA > 33 Sepsis, meningitis |
| Other | Respiratory distress syndrome and GA ≥ 37 Meconium aspiration syndrome All others |
GA: gestational age.
Summary of criteria for assigning case-specific cause of death for ENDs.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Tinatin Manjavidze AU - Charlotta Rylander AU - Finn Egil Skjeldestad AU - Nata Kazakhashvili AU - Erik Eik Anda PY - 2019 DA - 2019/08/28 TI - Incidence and Causes of Perinatal Mortality in Georgia JO - Journal of Epidemiology and Global Health SP - 163 EP - 168 VL - 9 IS - 3 SN - 2210-6014 UR - https://doi.org/10.2991/jegh.k.190818.001 DO - 10.2991/jegh.k.190818.001 ID - Manjavidze2019 ER -
