Survey of Respiratory Care Professionals’ Knowledge in Early Mobilization: A Pilot Study
- DOI
- 10.2991/j.jegh.2018.06.100How to use a DOI?
- Keywords
- Early mobilization; intensive care unit; mechanical ventilation; respiratory care
- Abstract
Early mobilization (EM) is practiced for intensive care unit (ICU) patients in many hospitals in the Eastern Province in Saudi Arabia. Respiratory care professionals’ knowledge about using EM was, therefore, surveyed and investigated to improve and update its practice and ultimately to develop related regulations and policies. A survey including 156 respiratory care professionals was conducted using a validated questionnaire. The focus was on collecting information on participants’ relevant backgrounds and on proper use of EM. Knowledge and proper use of EM were calculated in relation to participants’ demographic and professional characteristics. The statistical analysis using analysis of variance and Student t-test showed that factors that affected knowledge of EM were the respiratory care professional’s age, gender, nationality, and years of experience in intensive care medicine. How many patients these professionals treated using EM also significantly correlated with their knowledge of EM. The survey showed the extent of respiratory care professionals’ knowledge about the proper use of EM. More importantly, the survey also identified important shortfalls in practice of some experienced medical practitioners.
- Copyright
- © 2018 Atlantis Press International B.V.
- Open Access
- This is an open access article under the CC BY-NC license (http://creativecommons.org/licences/by-nc/4.0/).
1. INTRODUCTION
There is a wide range of complications in critically ill patients that prolong stay in the intensive care unit (ICU). Some of these complications relate to bed confinement, such as deep vein thrombosis, critical-care illness polyneuropathy, and bed sores [1].
Prolonged mechanical ventilation (MV) causes muscle weakness, which increases with duration of MV [2]. About 25% of patients who have been receiving MV for a few days have respiratory weakness because of an increase in diaphragmatic and skeletal muscle weakness. This makes weaning more difficult and prolongs hospital/ICU stay and ultimately increases mortality [3–5]. Also, inspiratory muscle strength worsens in patients subjected to prolonged MV, so practicing inspiratory muscle training has some potential benefits on weaning [6]. It has been clearly demonstrated that short-term controlled MV leads to rapid diaphragmatic atrophy. Indeed, after 18 hours of MV, diaphragmatic protein content and mass are significantly reduced and this leads to a decrease in the cross-sectional area of all four diaphragmatic myosin heavy chain types. Heavy sedation or paralysis of mechanically ventilated patients can cause generalized myopathy and prolong ICU stay [2].
Although physical therapists work routinely with ICU patients including those on MV, their practice varies in style and intensity among hospitals. There is no standardized, valid, and functional practice or regulated policy measures for this purpose, so more investigation is required to evaluate and unify such practices in the ICU [7]. In a European ICU survey focusing on the role of physiotherapists, only 75% of hospitals had at least one physiotherapist working exclusively in the ICU. Furthermore, the study showed that these practitioners usually gave enough attention to respiratory therapy, mobilization, and positioning, but neglected recommended early training sessions [6]. In a 1-day study conducted in a hospital in Germany, only 24% of mechanically ventilated patients and 8% of patients with an endotracheal tube were mobilized out of bed as part of routine care. This was due to the factors discussed in an earlier study [8].
Healthcare workers in ICUs differ in their degree of knowledge about early mobilization (EM) of critically ill patients. Initial investigation has suggested that variations in knowledge are due to many reasons, including lack of access to updated research and proper training on EM [7].
This study aimed to measure ICU workers’ knowledge of the proper use of EM and to develop ICU healthcare workers’ knowledge towards proper use of EM for critically ill patients. The research intended to: (1) correct any ICU healthcare workers’ misconceptions that they might have and unintentionally acquired during their practice; (2) break the barrier of fear regarding EM of critically ill patients; and (3) educate ICU workers about the benefits of EM in reducing mortality and cost by reducing length of hospital/ICU stay of critically ill patients.
2. MATERIALS AND METHODS
A questionnaire was developed and distributed to respiratory therapists (RTs) in five different hospitals in the Eastern Province, Saudi Arabia. The questionnaire consisted of 28 questions in two sections. Questions 1–9 were demographic questions and the other 19 questions were developed to measure practitioners’ knowledge about the proper use of EM. The survey was based on a cross-sectional questionnaire survey design.
The questionnaire was sent to all practitioners who were involved in EM practice. Participation in the survey was voluntary and no time limit was set for completion and return. Also, collaboration with colleagues and references to textbooks could not be monitored. So, this might have caused bias and led to higher scores, but this issue was not considered to have significant detrimental influence, as the participants were aware that it was solely a measure of their own knowledge. The format and content validity of the questionnaire was confirmed by three experts in the field. It was confirmed that this survey gave a realistic and reflective measure of knowledge about proper use of EM (Institutional Review Board (IRB), Imam Abdulrahman Bin Faisal University, Dammam, KSA).
Data were translated to percentages and summarized as mean and standard deviation (SD). Each correct answer was given a score of 1 and total knowledge scores were calculated. The mean and SD of all correct answers were calculated. Knowledge and proper use of EM were calculated in relation to participants’ demographic and professional characteristics. Statistical analysis was based on analysis of variance (ANOVA) and t-tests. Two-sided p-values <0.05 were considered statistically significant. SPSS version 22 (SPSS Inc., Chicago, IL, USA) was used for all data analysis.
3. RESULTS
The response rate for the questionnaire was 78% (156/200). Five questionnaires were excluded because their respondents answered <50% of the questions. Therefore, analysis was done on 75.5% (151/200) of the total distributed questionnaires. Table 1 shows the demographic data of the respondents. The gender distribution was almost equal, 75 (58.6%) male and 53 (41.4%) female. About 70% of the participants had bachelor degrees in respiratory care and 55% had 1–4 years of ICU experience.
| Factors | Characteristics | n (%) |
|---|---|---|
| Age (years) | 20–29 | 95 (64.2) |
| 30–39 | 39 (26.4) | |
| 40–49 | 11 (7.4) | |
| ≥50 | 3 (2) | |
| Gender | Male | 75 (58.6) |
| Female | 53 (41.4) | |
| Nationality | Saudi | 97 (72.9) |
| Non-Saudi | 36 (27.1) | |
| Qualifications | Diploma | 21 (13.9) |
| Bachelor degree | 107 (70.9) | |
| RRT/CRT | 9 (6) | |
| Masters’ degree | 9 (6) | |
| PhD | 0 | |
| Others | 5 (3.3) | |
| Years of practice | 1–4 | 82 (55) |
| 5–9 | 44 (29.5) | |
| 10–14 | 13 (8.7) | |
| ≥15 | 10 (6.7) | |
| Place of work | Ministry of Health | 44 (30.3) |
| Military | 39 (26.2) | |
| University | 28 (19.3) | |
| Private | 25 (16.6) | |
| Other | 10 (6.6) | |
| Using EM | Use | 99 (72.1) |
| Not used | 76 (55.3) | |
| Patients treated with EM, n | <10 | 51 (28.1) |
| 10–20 | 68 (36.75) | |
| >20 | 65 (35) |
CRT, certified respiratory therapist; EM, early mobilization; RRT, registered respiratory therapist.
Demographic data of the respondents
3.1. EM Use
Only 42% (60/143) of respondents used EM, with about 90% of them using it in the ICU. About 40% (55/138) reported that they used EM while the patients were still intubated and 16.7% (23/138) used EM within 12 hours postextubation; 21.7% (30/138) used EM 12–24 hours postextubation, while 21.7% (30/138) used EM >24 hours postextubation.
3.2. EM Knowledge
The average of all the respondents was 62.89 ± 21.3 (mean ± SD). Table 2 shows the percentage of respondents who answered correctly or incorrectly. It is worth noting that there was a misunderstanding in the definition of EM between participants, to the extent that 63.3% (95/150) believed that EM meant bringing patients out of bed, whereas 36.7% (55/150) believed that EM may include activities other than bringing patients out of bed.
| Questions | Correct | Incorrect | |
|---|---|---|---|
| 1 | Critically ill patients who are mechanically ventilated must have complete bed rest and be immobilized. | 58 (38.9) | 91 (61.1) |
| 2 | Physical exercises should be considered a routine part of the ICU care. | 116 (77.9) | 33 (22.1) |
| 3 | Lung compliance increases in the sitting position and decreases in the supine position. | 114 (77.6) | 33 (22.4) |
| 4 | EM decreases ICU length of stay. | 103 (68.2) | 47 (31.3) |
| 5 | EM of ventilated patients in the ICU aids in weaning and reduces time spent on mechanical ventilation. | 99 (66) | 51 (34) |
| 6 | EM of ventilated patients in the ICU reduces delirium and improve patient awareness. | 90 (60) | 60 (40) |
| 7 | EM of mechanically ventilated patients is feasible and safe for them. | 67 (45.3) | 81 (54.7) |
| 8 | EM of ventilated patients in the ICU requires a multidisciplinary team approach. | 122 (80.8) | 29 (19.2) |
| 9 | EM of ventilated patients in the ICU can be performed by the RT alone. | 116 (76.8) | 35 (23.2) |
| 10 | EM should not be attempted in the patient who suffers from high ICP or spinal cord injury. | 97 (64.7) | 53 (35.3) |
| 11 | EM decreases the incidence of ventilation associated pneumonia. | 99 (66) | 51 (34) |
| 12 | Patients who have received EM require less sedation. | 104 (68.9) | 47 (31.1) |
| 13 | In order to initiate mobilization, the patient must be responsive to verbal commands. | 93 (61.6) | 58 (38.4) |
| 14 | In order to initiate mobilization, the patient must be hemodynamically stable (not requiring infusion of vasoactive drugs). | 104 (69.3) | 46 (30.7) |
| 15 | Mobilization should not be attempted if the patient refuses it. | 73 (49) | 76 (51) |
| 16 | ICU-acquired weakness is a common complication of critical illness. | 107 (71.8) | 42 (28.2) |
| 17 | EM leads to patient discomfort. | 63 (42) | 87 (58) |
| 18 | EM improves patient oxygenation. | 107 (71.3) | 43 (28.7) |
| 19 | EM means bringing patient out of bed. | 55 (36.7) | 95 (63.3) |
EM, early mobilization; ICP, intracranial pressure; ICU, intensive care unit; RT, respiratory therapist.
Number (percentage) of respondents who answered each question correctly or incorrectly
3.3. Factors that Affect Knowledge of EM
There was a significant difference in EM knowledge among different age groups (p < 0.0001). Multiple comparisons showed that the knowledge of those aged 30–39 years (69.8 ± 15.4), 40–49 years (80.4 ± 10.8), and >50 years (82.5 ± 18.5) was significantly greater than the knowledge of those aged 20–29 years (56.7 ± 18.5). Independent t-test revealed that the knowledge of women (68.3 ± 13.8) was significantly higher than that of men (59.0 ± 23.3) (p < 0.05). Comparing the knowledge of Saudi and non-Saudi nationals, independent t-test showed that the knowledge of the non-Saudis (73.1 ± 18.0) was significantly higher than that of Saudis (59.4 ± 20.5) (p < 0.001). One-way ANOVA showed that the number of years of experience in the ICU significantly affected the knowledge of RTs regarding EM (p < 0.001). Tukey’s post-hoc test showed that the knowledge of RTs with more 5–9 years’ experience in the ICU (68.1 ± 16.3), 10–14 years (76.9 ± 13.7) and >15 years (80.5 ± 14.2) was greater than that of RTs with 1–4 years’ experience (55 ± 22.6). The knowledge of RTs who used EM (72.1 ± 12.9) was significantly higher than that of respiratory therapists who did not use EM (55.3 ± 24) (p < 0.0001). However, where EM was used (within or out of the ICU) did not make a difference to the knowledge of the RTs. The knowledge of RTs who treated 10–20 patients (64.6 ± 22.6) or >20 patients (67.8 ± 14.2) was greater than that of RTs who treated <10 patients (51.8 ± 25.9) (p < 0.001). Two-way ANOVA showed that there was no significant interaction between age and experience, age and number of patients treated, nationality and experience, and nationality and number of patients treated with EM.
4. DISCUSSION
The meaning of EM to critically ill patients in ICUs, its proper use, the precautions to be considered when using it, its advantages, and its feasibility in daily clinical work were defined and discussed in this study. In addition, we examined a group of healthcare workers’ knowledge against stated definitions.
Overall, 63% of the participants in our study gave correct answers about knowledge of EM for critically ill ICU patients, which was comparable with a previous study [9]. Over half of the respondents (61%) believed that mechanically ventilated patients should not be mobilized and continued with bed rest.
Healthcare workers in ICUs differed in their degree of knowledge about EM of critically ill patients. Our initial investigation showed that there were many possible reasons for the variation in degree of knowledge, including lack of access to the latest research on EM and lack of proper EM training. There is evidence that EM for ICU patients if practiced properly and with suitable precautions, can have many advantages that reduce complications and speed weaning and recovery by shortening hospital/ICU stay, hence minimizing side effects and improving morbidity and mortality [10].
Many studies support the fact that EM is safe in mechanically ventilated patients and has positive effects [10]. About 60% of respondents believed that EM improved functional independence and reduced ICU delirium, duration of MV, and hospital/ICU length of stay and mortality. For example, a 6-minute walking exercise has been shown to improve SF-36 physical function score and muscle strength (The short form (36) health survey is a 36-item, patient-reported survey of patient health to measure the health status). EM can be initiated within 48 hours of subjecting the patient to MV and can be continued during the length of ICU stay [6]. Active mobilization appears to have a positive effect on physical function and hospital outcomes in MV patients [11]. However, there are many factors that limit the use of EM. One of the main factors is sedation, such as benzodiazepines, propofol, haloperidol, and opiates. This type of medication is sometimes given to manage agitation and anxiety, and to facilitate general medical care [12]. Other limiting factors include administration of vasoactive agents, ICU staff time, risk of self-injury, and other more persisting priorities [13].
We did not find any association between academic qualifications, place of work, and time of starting EM and knowledge of healthcare workers. However, there was a significant association between demographic factors (age, gender, nationality, and years of experience) and correct knowledge of EM (Table 3). Using early mobilization and number of patients treated with EM showed significant association between them and this finding is consistent with one of the study [14]. More research is required to identify which specific group of MV patients will most benefit from EM. In general EM is good for patients but protocols are essential if it is to be effective; as stated by Li et al. [10], “early active mobilization protocols may be initiated safely in the ICU setting and continued in post-ICU settings”. Almost all (80%) of the respondents believed that EM of ventilated patients in the ICU requires a multidisciplinary team approach [9].
| Factors | Categories | Percentage of correct answers | F/t-value with (df) | p-Value |
|---|---|---|---|---|
| Age (years) | 20–29 | 56.7 ± 18.5 | 8.07 (3)a | <0.001* |
| 30–39 | 69.8 ± 15.4 | |||
| 40–49 | 80.4 ± 10.8 | |||
| > 50 | 82.5 ± 18.5 | |||
| Gender | Male | 59.0 ± 23.3 | 2.5 (128) | <0.05* |
| Female | 68.3 ± 13.8 | |||
| Nationality | Saudi | 59.4 ± 20.5 | 3.5 (131) | <0.001* |
| Non-Saudi | 73.1 ± 18.0 | |||
| Qualifications | Bachelor degree | 64.19 ± 19.10 | 3.6 (4)a | 0.06 |
| Diploma | 55.13 ± 22.49 | |||
| Masters’ degree | 63.15 ± 24.54 | |||
| Other | 33.68 ± 43.81 | |||
| RRT/CRT | 71.34 ± 15.14 | |||
| Experience in ICU, years | 1–4 | 55.00 ± 22.68 | 10.10 (3)a | <0.001* |
| 5–9 | 68.06 ± 16.22 | |||
| 10–14 | 76.92 ± 13.68 | |||
| >15 | 80.52 ± 14.04 | |||
| Place of work | Military | 59.14 ± 22.67 | 3.21 (4)a | 0.07 |
| Ministry of Health | 66.50 ± 17.18 | |||
| Private | 70.73 ± 15.27 | |||
| University | 60.71 ± 23.55 | |||
| Other | 45.78 ± 33.19 | |||
| Using EM | No | 55.29 ± 23.99 | 4.9 (141) | <0.001* |
| Yes | 72.10 ± 12.86 | |||
| No. of patients treated with EM | <10 | 51.77 ± 25.90 | 8 (2)a | <0.001* |
| 10–20 | 64.64 ± 22.18 | |||
| >20 | 67.80 ± 14.24 | |||
| Time starting EM | 12–24 hours postextubation | 66.66 ± 13.28 | 0.93 (3)a | 0.42 |
| >24 hours postextubation | 59.29 ± 20.63 | |||
| While patient is still intubated | 65.45 ± 22.02 | |||
| Within 12 hours postextubation | 66.36 ± 18.89 |
Analysis of variance and independent sample t-test was performed to compare the mean knowledge score with the different attributes; Data are presented as n (%) or mean ± SD; • Significant association; CRT, certified respiratory therapist; df, degrees of freedom; EM, early mobilization; ICU, intensive care unit; RRT, registered respiratory therapist.
Association between demographic factors and correct knowledge of EM
In conclusion, lack of training in EM means that healthcare workers’ knowledge and skills in proper use of EM need extensive and systematic improvement. Standardized legislation needs to be developed to establish guidelines in the ICU for the proper use of EM.
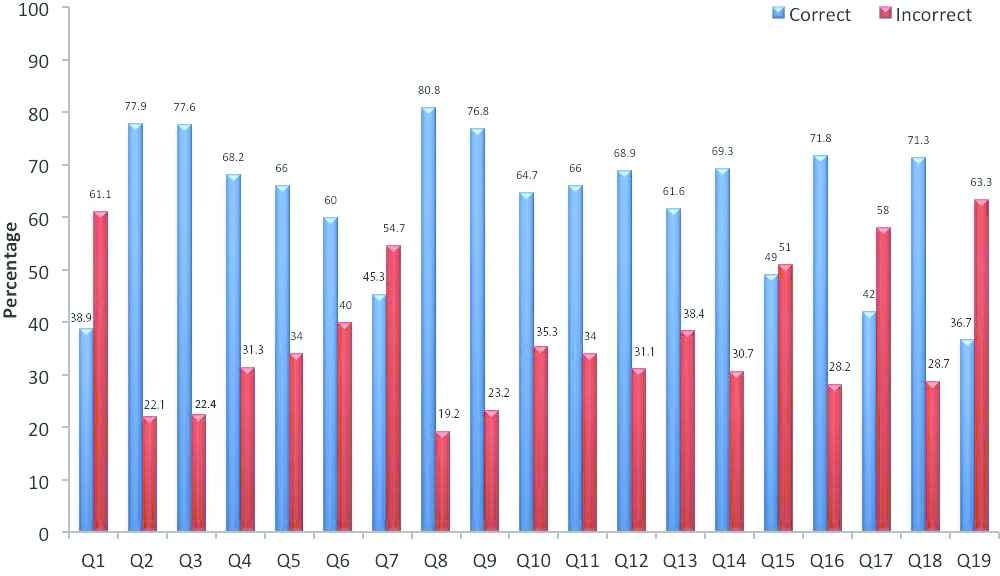
Overall percentages of correct and incorrect answers for each question in the questionnaire
CONFLICTS OF INTEREST
The authors have no conflicts of interest and the work was not supported or funded by any drug company.
REFERENCES
Cite this article
TY - JOUR AU - Hatem Othman Qutub AU - Abdelaziz Smiah Matani AU - Faraz Ahmed Farooqi PY - 2018 DA - 2018/12/31 TI - Survey of Respiratory Care Professionals’ Knowledge in Early Mobilization: A Pilot Study JO - Journal of Epidemiology and Global Health SP - 208 EP - 212 VL - 8 IS - 3-4 SN - 2210-6014 UR - https://doi.org/10.2991/j.jegh.2018.06.100 DO - 10.2991/j.jegh.2018.06.100 ID - Qutub2018 ER -
