Systematic Review: Awareness, Knowledge, Attitude, and Practice of Cancer Screening Program in the Kingdom of Saudi Arabia

- DOI
- 10.2991/dsahmj.k.200626.001How to use a DOI?
- Keywords
- Cancer screening; awareness; attitude; knowledge; practice; Kingdom of Saudi Arabia
- Abstract
Cancer is the second most frequent cause of death worldwide after ischemic heart disease. Early detection of cancer is a cornerstone of cancer survival. The aim of this review is to summarize the current knowledge, awareness, attitude, and practice of cancer screening programs in Saudi Arabia. A literature review was conducted using PubMed, Embase, and Google Scholar to identify which cancer screening programs have been studied in Saudi from 2015 to 2019. The search was done using the key terms with Boolean operators “Cancer, Tumor, Saudi, Screening, Knowledge, Awareness, Attitude, Practice, Breast, Colorectal, Cervical, Prostate, Head and Neck.” Twenty-three articles were included. There were eight articles about the screening of Colorectal Cancer (CRC), eight articles about the screening of Breast Cancer (BC), five articles for Cervical Cancer (CC) screening, one article for the screening of prostate cancer, and one for the screening of head and neck cancer. All the included studies reported poor awareness levels about the cancer screening program (CRC screening: 19.1%), and (BC screening: 25%). However, the awareness level of CC screening was the highest among them (52.5%). Majority of the population had never done or had been advised by a healthcare provider to perform the screening test before. All types of cancer showed a low level of practicing cancer screening programs, ranging from 10% to 15%. Several studies demonstrated that most of the Saudi population had never been screened for cancer. There is a need for population-based interventions to fill the gap of knowledge and practice of cancer screening in Saudi Arabia.
- Copyright
- © 2020 Dr. Sulaiman Al Habib Medical Group. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Worldwide, cancer is the second leading cause of death after ischemic heart disease [1]. The International Agency for Research on Cancer (IARC) reported that the global burden of cancer worldwide has increased to 18.1 million new cases and 9.6 million deaths in 2018 [2]. As a part of the IARC, the Global Cancer Observatory predicts that the future incidence and mortality of cancer will increase to 29.5 million new cases and around 16.4 million deaths worldwide by 2040 [3]. The World Health Organization (WHO) showed that cancer-related deaths in the Kingdom of Saudi Arabia (KSA) exceeded 9000 in 2014 [4], whereas it increased to 10,518 in 2018 [5]. In addition, the number of new cancer cases in KSA in 2018 was 24,485, whereas in 2014 the number of reported cases was 15,807 [4,5].
Data from the Global Burden of Disease (2017) database showed that colon cancer has the highest mortality rate among all types of cancer, accounting for 1.6% of deaths worldwide and 1.43% of deaths in Saudi Arabia. Breast cancer represents 1.09% of deaths worldwide and 0.96% of deaths in Saudi Arabia. Prostate cancer is the cause of death in men in 0.74% of the population worldwide and 0.58% of Saudis. Females’ deaths from cervical cancers represent 0.46% of mortality cases worldwide and 0.12% in Saudi population. Deaths from lip and oral cavity cancer worldwide and in Saudi Arabia are 0.35% and 0.22%, respectively. Overall, these five types of cancer represent 4.24% of mortality cases worldwide and 3.31% of mortality cases in Saudi Arabia [1,4].
Early detection of cancer is a cornerstone of cancer survival [6]. It can be achieved by focusing on two major components: screening and education of healthcare providers and the general public [7]. Cancer screening programs can lead to early diagnosis, which contributes to early intervention and better impact on the disease [8]. Available evidence-based practice and research show the benefits of screening programs and their impact on incidence and mortality rates. The American Cancer Society (ACS) provides annual guidelines for screening of certain cancers; for example, it recommends that Colorectal Cancer (CRC) screening should start from the age of 50 years. However, the recent recommendation, which was published in May 2018, recommends to start CRC Screening (CRCS) from the age of 45 years with either stool-based test or visual examination [9,10]. Between 2000 and 2014, screening has contributed in the decline of CRC incidence rate by 32% and decrease in mortality rate by 34% among adults aged 50 years and older [11].
Breast Cancer (BC) screening should start from the age 45–54 years annually with a mammogram. Then, screening with mammogram should be performed every 2 years starting from 55 years and older. According to the ACS, since the implementation of BC screening, age-adjusted breast cancer mortality rates have declined 39% from 1989 through 2015 [11,12]. Meanwhile, Cervical Cancer (CC) screening using Papanicolaou (Pap) test has played a crucial role in decreasing mortality from squamous cell cervical cancer, which comprises 80–90% of cervical cancers, since it was introduced in the mid-20th century [13]. From 2003 to 2014, SEER Cancer Statistics Review reports that cervical cancer mortality rates have declined at an average annual rate of 0.8% [11,14]. The ACS recommends to start screening at the age of 21–29 years every 3 years with a Pap smear testing. Then, from the age of 30–59 years, women are advised to undergo screening every 3 years with Pap smear alone or every 5 years if screening is performed with both Pap smear and human papillomavirus test [15].
Prostate Cancer (PC) screening depends on the patient’s preference after they are informed about the benefits and harms of the screening with Prostate-specific Antigen (PSA). The healthcare providers should discuss PC screening in asymptomatic men at the age of 50 years and older [16]. PC screening has decreased the mortality rate among men with age-adjusted death rates from about 40 deaths per 100,000 men in 1992 to about 20 per 100,000 in 2013 [17]. Head and Neck Cancer (HNC) screening is carried out via systematic clinical examination of the head and neck region including lymph nodes starting from the age of 18 years. It is not clear whether HNC screening is recommended owing to a lack of supporting evidence [18,19].
There have been several studies conducted in Saudi Arabia about the knowledge of cancer screening programs. However, evidence needs to be summarized in a systematic review to obtain a broader picture of the situation to plan and implement health promotion and education related to cancer screening. The aim of this review is to summarize the current knowledge, awareness, attitude, and practice of cancer screening programs in Saudi Arabia.
2. MATERIALS AND METHODS
2.1. Data Collection Strategy
Studies were systematically retrieved and extracted from PubMed, Embase, and Google Scholar. Studies published from 2015 to 2019 were included to ensure that the review included the most updated published articles. To broaden the scope and enrich the review, cross-referencing and local journals search, have been performed. The search was done in two steps. First, general search was done using the key terms “Cancer” AND “Saudi” AND “Screening” to decide which types of cancer screening programs should be included in the review based on the published articles. Therefore, 522 articles have been reviewed, and among those articles, five types of cancer screening programs were identified and included. In the second step, specific search was conducted on the included cancer screening programs using the following keywords: “Cancer OR Tumor” AND “Saudi” AND “Screening” AND “Knowledge OR Awareness OR Attitude OR Practice” AND “Breast OR Colorectal OR Cervical OR Prostate OR Head and Neck,” which resulted in the retrieval of 133 relevant articles. The search was conducted on February 27, 2019 and the last update was made on August 2, 2019.
2.2. Study Eligibility Criteria
Inclusion criteria were articles published in 2015 and beyond, among the Saudi population, reporting knowledge, awareness, attitude, or practice related to screening programs of colorectal, breast, prostate, cervical, and head and neck cancers in Saudi Arabia. Exclusion criteria were studies that measured cancer screening programs in healthcare workers, and not in the general population. In addition, studies performed outside Saudi Arabia, systematic review or meta-analysis, and studies that are nonrelevant to the review were not considered.
2.3. Identification and Study Selection
The abstract of screened articles were reviewed by two researchers (DA and GA). A more specified search was then conducted for each type of cancer, and the results were reviewed by two independent reviewers (AA and ZA) to assess for inclusion in this review and for the removal of duplicates. If there was any conflict between the reviewers’ decision, the assessment of third reviewer (AE) was considered. Selection of articles to be included followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
2.4. Data Analysis
A total of 522 articles were identified in the original search. Duplicate articles were removed. The remaining papers were further scanned on the basis of their relevance to the topic. Titles and abstracts of each article were reviewed in order to apply the inclusion criteria. All articles with irrelevant topic or different population were excluded. A total of 64 full-text articles were assessed for eligibility. Twenty-three relevant articles that met the inclusion criteria were included. The data collected (summarized in Tables 1–5) were formulated and included details on type of cancer, year, outcome measure, setting/sampling technique, study design, sample size, and key study findings (Figure 1).
| First author, year | Study design/data collection | Region/population | Main results |
|---|---|---|---|
| Khoja et al., 2018 [20] |
|
|
|
| Zubaidi et al., 2010 [21] |
|
|
|
| Almutairi et al., 2015 [22] |
|
|
|
| Almadi et al., 2013 [23] |
|
|
|
| Al Sharif et al., 2018 [24] |
|
|
|
| Almadi et al. [25] |
|
|
|
| Al-Thafar et al., 2017 [26] |
|
|
|
| Alsayed et al., 2018 [27] |
|
|
|
CI, confidence interval; FOBT, fecal occult blood test; FHL, functional health literacy which is defined as “the degree to which individuals have the capacity to obtain, communicate, process, and understand basic health information and services needed to make appropriate health decisions”; SD, standard deviation.
Colorectal Cancer Screening (CRCS) program
| First author, year | Study design/data collection | Region/population | Main results |
|---|---|---|---|
| El Bcheraoui et al., 2013 [28] |
|
|
|
| Al-Zalabani et al., 2015 [29] |
|
|
|
| Binhussien and Ghoraba, 2018 [30] |
|
|
|
| Alshahrani et al., 2017 [31] |
|
|
|
| Abdel-Aziz et al., 2015 [32] |
|
|
|
| Al-Wassia et al., 2017 [33] |
|
|
|
| Al Otaibi et al., 2017 [34] |
|
|
|
| Almutairi et al., 2016 [35] |
|
|
|
AOR, adjusted odds ratio; BSE, breast self-examination.
Breast Cancer (BC) screening program
| First author, year | Study design/data collection | Region/population | Main results |
|---|---|---|---|
| Salem et al., 2017 [36] |
|
|
|
| Al Khudairi et al., 2016 [37] |
|
|
|
| Dhaher et al., 2017 [38] |
|
|
|
| Aldohaian et al., 2018 [39] |
|
|
|
| Alnafisah et al., 2018 [40] |
|
|
|
King Khaled University, Alyamamah, King Saud Hospital, and King Fahad Medical City. AOR, adjusted odds ratio; BSE, breast self-examination.
Cervical Cancer (CC) screening program
| First author, year | Study design/data collection | Region/population | Main results |
|---|---|---|---|
| Arafa et al., 2015 [41] |
|
|
|
Prostate Cancer (PC) screening program
| First author, year | Study design/data collection | Region/population | Main results |
|---|---|---|---|
| Alhazzazi, 2016 [42] |
|
|
|
Head and Neck Cancer (HNC) screening program
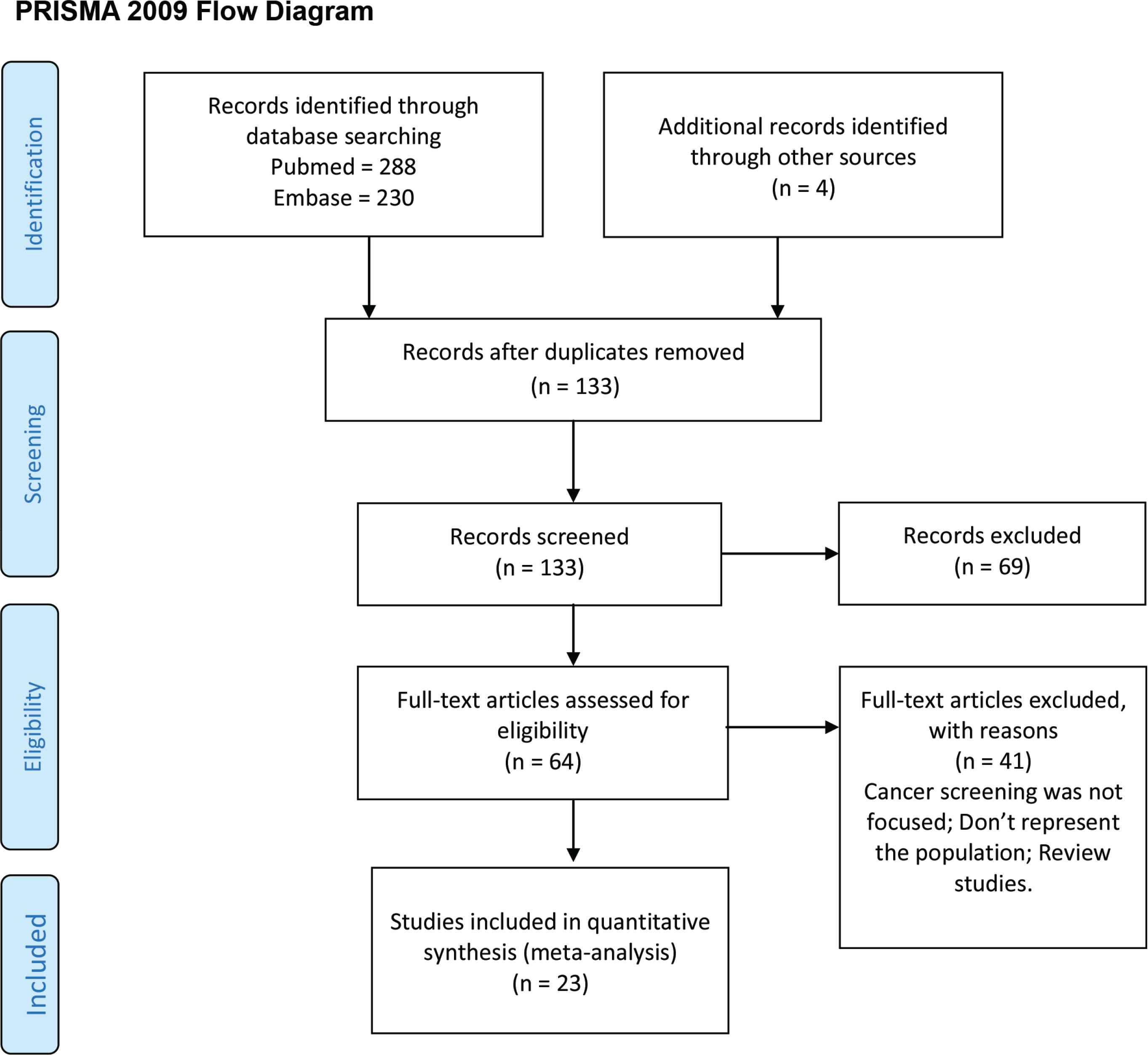
Process of research used in this study.
3. RESULTS
The Tables 1–5 describe each article that met the inclusion criteria and the objectives of this review. As summarized in the tables, there were 23 articles included that focused on awareness, knowledge, practice, or attitude toward screening of different types of cancer. There were eight articles on screening of colorectal cancer, eight articles on screening of breast cancer, five articles for cervical cancer screening, one article for screening of prostate cancer, and one for screening of HNC.
3.1. Colorectal Cancer Screening Program
Table 1 summarizes CRCS articles. Only one out of eight studies measured the awareness of CRCS (Table 1). Al-Thafar et al. [26] showed that only 19.1% of participants acknowledged the presence of CRCS. Five out of eight studies assessed knowledge about the recommended age for CRC screening [21,23–25,27] and stated that the prevalence of participants who knew the correct age for screening, which were 13.1%, 22.1%, 25%, 35.1%, and 49.6%, respectively. Four studies investigated knowledge about the recommended screening tool. Almutairi et al. [22] found a significant association between knowing the correct age for colonoscopy and sigmoidoscopy, and functional health literacy (p = 0.001). Almadi et al. [23], Al-Sharif et al. [24], Almadi et al. [25], Al-Thafar et al. [26], and Alsayed et al. [27] showed the prevalence of awareness of the recommended screening tool (50.56%, 15.5%, 34.6%, 35%, and 2.2%, respectively). Al-Sharif et al. [24] considered sex and age as factors affecting the knowledge about the time of screening and used test. For sex, there was no significant difference in the knowledge of the recommended time for screening and its test (p = 0.717 and 0.534, respectively). However, participants aged between 50 and 59 years were more likely to answer correctly the time of screening but not the modality (p < 0.001 and 0.285, respectively).
Attitude and willingness to undergo the screening test were evaluated by four studies. Almadi et al. [23] found that willingness to undergo CRC screening test was 70.7% and increased to 83% among those with a family history of CRC. Moreover, colonoscopy was accepted as a screening tool in 68.9%. In addition, there was no difference in the acceptance to undergo screening with colonoscopy if offered for free or if a participant had to pay for it (68.5% vs. 69.7%, respectively). Almadi et al. [25] noted that CRC screening was accepted by 73%, and this rate increased to 80% if there was a history of CRC in the family. Of the participants, 81% expressed willingness to undergo a colonoscopy as a screening test. If colonoscopy was offered for free, the acceptance of the test decreased to 56%, whereas if respondents had to pay, it increased to 92%. In addition, participants who were accepting of the screening changed their minds when they were invited to undergo the screening. Meanwhile, participants who refused to do the screening in the survey were more accepting to undergo the test. Alsayed et al. [27] and Al Thafar et al. [26] showed that acceptance of colonoscopy as the chosen tool for screening was 20.8% and 68.1%, respectively. Almadi et al. [23] reported factors that were more associated with an increase or decrease in willingness to undergo a screening test. Participants were more likely to undergo screening if they believed that age and being male were risk factors for CRC (p = 0.02 and 0.01, respectively). Their willingness increased when participants thought abdominal pain is a symptom of CRC (p < 0.01). In addition, participants who answered colonoscopy as the screening tool were more likely to say they would undergo the screening [Odds Ratio (OR) = 3.01; 95% Confidence Interval (CI), 1.85–4.90]. Moreover, if they strongly disagreed that colonoscopy is harmful, their willingness increased (p < 0.01). Conversely, their willingness decreased if they did not want to know if they had cancer (p < 0.01) or if they believed that screening starts at the age of 70–79 years (OR = 0.53; 95% CI, 0.30–0.93).
Three studies measured the current practice and adherence to the recommended screening guidelines. Almadi et al. [23] found that 6.7% of participants aged 50–55 years had undergone the screening, whereas only 6.5% of those aged 55–60 years had undergone the screening and the majority of them had colonoscopy. Meanwhile, Khoja et al. [20] reported that 5.6% had undergone CRC screening, with the fecal occult blood test being the most often used screening tool. Furthermore, 16.8% of those who were screened reported blood during the interview. Moreover, it was noticed that there was a statistically significant relationship between history of weight loss (p = 0.039) or blood in the stool and increased likelihood of screening (OR = 2.80; 95% CI, 1.3–6.00). Almadi et al. [25] stated that the proportion of CRC screening takers in their study was 15.24%, with 72.73% of them having undergone colonoscopy.
3.2. Breast Cancer Screening Program
Table 2 summarizes BC screening articles. In general, the included studies showed that there is poor knowledge about breast cancer screening among Saudi females, with more than 80% of the respondents having a low level of knowledge. In their study, Al Otaibi et al. [34] showed different results with 62% of participants having poor knowledge of BC screening. Among those who showed good knowledge, the participants appeared to be familiar with the tools and methods used for BC screening (clinical breast examination and mammogram). But their knowledge of the right age to undergo BC screening was low. Nevertheless, two of the studies [26,31] reported that females living in the western region of Saudi Arabia have better knowledge of BC screening. Predictors of participants’ awareness of the screening were measured by Al-Wassia et al. [33] and Al Otaibi et al. [34], and results showed that women with a higher level of education, and marital and the occupational status have a greater awareness of BC screening (p < 0.001).
In addition, some of the studies have reviewed sources of information about BC screening. Alshahrani et al. [31] and Al Otaibi et al. [34] showed that the major sources of such information were the social media, TV shows, and awareness campaigns, whereas fewer respondents (8.8%) had been instructed by their healthcare providers. By contrast, Abdel-Aziz et al. [32] showed that more than 40% of the participants were advised by their healthcare providers to undergo the screening.
In a study by Abdel-Aziz et al. [32], participants were asked if they are willing to go for BC screening after the study. Their response showed that 86.5% were seriously planning to have BC screening in the near future, and 80.4% of them expressed willingness to go if the procedure is free and painless, and if the examiner is a female.
3.3. Cervical Cancer Screening Program
Table 3 summarizes the CC screening articles. Salem et al. [36], Al Khudairi et al. [37], Aldohaian et al. [39], and Alnafisah et al. [40] measured the awareness of respondents regarding the CC screening program, and results showed that only 26.7%, 46.2%, 48.7%, and 52.5% respectively, were aware of it. Several studies [36,37,39] have also reported a low level of knowledge about the appropriate age for screening (30%, 18.1%, and 33.1%, respectively). Salem et al. [36] and Aldohaian et al. [39] reported that 71.9% and 82%, respectively, of the participants recognized Pap smear as the screening test for CC, whereas Al Khudairi et al. [37] reported that 61.5% of women were not aware of the importance of Pap smear. Al Khudairi et al. [37] reported that 92.9% of the participants did not know how frequently they needed to undergo the screening test, and 93.9% did not know when to stop undergoing the screening. Alnafisah et al. [40] showed that only 35.8% of the participants answered correctly the frequency of the screening test. Aldohaian et al. [39] questioned participants about the source of their knowledge, and most of them said that they gained such knowledge from health professionals (59.8%), followed by the media (23.7%). In addition, Al Khudairi et al. [37] reported that most of the participants who heard about the screening program cited their gynecologist 56.1%, followed by healthcare facilities and staff (15.4%), media (9.9%), friends (9.2%), and posters (8.4%). However, 75.5% of the participants stated that their physicians had never advised them to undergo the screening. Regarding the clinical practice of CC screening, Dhaher [38], Salem et al. [36], Alnafisah et al. [40], Al Khudairi et al. [37], and Aldohaian et al. [39] reported that only 0.8%, 14.6%, 15.3%, 24.9%, and 26%, respectively, of the participants have undergone CC screening. Al Khudairi et al. [37] also showed that 84.6% of women have never asked their physicians to perform Pap smear. Moreover, Al Khudairi et al. [37] and Aldohaian et al. [39] showed that 95.3% and 70%, respectively, were interested to learn more about the screening. Meanwhile, Dhaher [38] noted that 38% of women were willing to undergo the screening.
3.4. Prostate Cancer Screening Program
Table 4 summarizes PC screening article. In assessment of knowledge related to prostate function and disorder, the mean of total correct knowledge score of men in Riyadh was 10.25 ± 2.5 out of 20 (51.25%). The average score of their attitude toward prostate cancer was 18.3 ± 4.08 out of 28 (65.3%). Although 70% of participants believed that men older than 45 years will benefit from prostate cancer checkup, only 10% of men in Riyadh had prostate cancer screening either by Digital Rectal Examination (DRE; 3.2%) or by PSA (6.8%). A large number of participants (41.4%) believed that undergoing prostate cancer examination is costly, and 48% would not prefer having their checkup because it would increase their worries and anxiety. The main factor that played a role in their attitude toward prostate cancer screening was total knowledge (p < 0.001).
3.5. HNC Screening Program
Table 5 summarizes HNC article [42]. For the general population in Jeddah, 68% indicated that they never received any information about HNC. The rest received some information from the social media (39%), dentists (33%), educational lectures (28%), or television (28%). The majority of participants (86%) had never been screened for HNC.
4. DISCUSSION
To the authors’ knowledge, this is the first review about awareness, knowledge, practice, and attitude toward screening of different types of cancer in Saudi Arabia done in the past 5 years. Based on the results of this review, we found that the Saudi population showed poor knowledge of all types of cancer screening programs. Furthermore, the majority of them have never undergone or have never been advised by a healthcare provider to undergo screening. However, participants expressed an interest to know more about the cancer screening program, and consequently, they were more willing to go through the screening test.
4.1. Colorectal Cancer
Unfortunately, there are no previously published articles about the CRCS awareness, attitude, or knowledge with which to compare the current review to evaluate CRCS implementation through the years. The current review has reported that the estimated knowledge of CRCS is between 22% and 50%. By contrast, in Europe the knowledge level in 2004 was 51%. Hence, the awareness in Europe was higher than in Saudi Arabia even about 15 years ago. Nevertheless, the willingness to undergo screening was nearly the same between both Saudis and Europeans [43]. Regarding the implementation of screening in the United States and Canada, there is a report published by WHO and Pan American Health Organization showing that the CRC screening program coverage was about 43% in Canada and 58.2% in US populations [44]. Unfortunately, the reported results from the review have showed low implementation of CRCS. Less than 7% of the participants have undergone screening with colonoscopy or fecal occult blood test. Moreover, many of the screened participants reported a history of bleeding with defecation or weight loss prior to undergoing the screening. A published article about the practice of implementing CRCS by family physicians showed that 56.2% of 130 physicians were not practicing CRCS. Interestingly, 94.6% of the physicians believed that CRCS is an effective tool for early detection of CRC [45].
4.2. Breast Cancer
The included studies of BC screening focused mainly on measuring knowledge and awareness of screening, which revealed overall poor knowledge among Saudis.
Most of them indicated that the main source of their information was campaigns whereas healthcare providers play only a very small role in instructing their patients to undergo screening. In a similar review that was conducted to analyze the barriers to BC screening among American women, George [46] found that the lack of physician recommendation plays a major barrier to BC screening. Kurashi and Al Alaboud [47] determined that the barriers blocking physicians from recommending mammograms to their patients were mainly attributed to the lack of national screening programs followed by lack of training, facilities, and time.
In 2007, the first national public breast cancer screening program was started, Abulkhair et al. [48] showed that there is public acceptance of breast cancer screening programs since the program started. However, since the first implementation of the national screening program until today, studies have shown poor knowledge of BC screening. Hussein et al. [49] noted that more than 60% of women who live in the northern region of Saudi Arabia had poor knowledge about BC screening; even among those who had good knowledge, some exhibited reluctance to undergo the screening and fear was cited as the main barrier. In another study, Ravichandran et al. [50] demonstrated that about 68% of the participants in Riyadh had never heard of BC screening, which is comparable to our results; this shows that an increased level of education is associated with better knowledge.
Moreover, Mahfouz et al. [51] found that less than half of southwestern Saudi women knew about BC screening and less than 7% had been examined by mammography. The common barrier between this study and our findings is fear.
In addition, a systematic review by Bowser et al. [52] identified barriers to BC screening programs in the Middle East and North Africa, and showed that physician recommendations increase the odds of mammogram use. Furthermore, our findings revealed that fear of pain, availability of the test, and the sex of the examiner were regarded as barriers to using the test. The latter was identified by Bowser et al. [52], who stated that having a female examiner helps to increase the utilization of mammograms. Although no information was found in the literature to support the first two issues (fear of pain and availability of the test), further studies should be done to identify these barriers and come up with health education models that will contribute in increasing the utilization of screening tests.
4.3. Cervical Cancer
Healthy People 2020 (HP2020) provides health objectives to improve national health. The cervical cancer screening objective espoused by HP2020 is to increase cervical cancer screening takers up to 93% among women in the appropriate age bracket (21–64 years). In the United States, national data analysis in 2008 reported that only 60.2% of women in the targeted age range were screened. Unfortunately, the cervical cancer screening objective could not be achieved; moreover, the percentage is declining [53,54]. Meanwhile, the results of the reviewed articles have shown that the percentage of screened women ranged from 0.8% to 26%, depending on the region. In addition, more than 40% of Saudi women are diagnosed with cervical cancer at advanced stages, compared to 25% in British Columbia, Canada. The high prevalence of diagnosis of cervical cancer in advanced stage is probably the consequence of lack of effective prevention and screening programs in Saudi Arabia [55]. It is essential to enhance the role of primary healthcare facilities, private practices, and government agencies to increase the level of knowledge and awareness of cervical cancer and screening methods among women and provide the accepted screening facilities. Many countries have implemented educational campaigns to improve public knowledge about cervical cancer prevention and encourage women to accept new methods for screening [56].
4.4. Prostate Cancer
The prostate cancer knowledge score was similar for the Saudi population in 2011 and 2015 (10.25 ± 2.5 out of 20) with 55% agreement with the statement (physicians can discover PC through DRE) in both studies [41,57]. In 2009, surveyed primary care physicians in Riyadh identified that PSA (79.1%) and DRE (68.9%) are used for routine prostate cancer screening [58]. The motives for undergoing prostate cancer screening among Saudi males remained the same over the period 2011–2015 and included assurance and routine checkup (44%), physicians’ medical advice (22.2%), and appearance of symptoms (6.7%) [41,57]. The main sources of information regarding prostate cancer and screening for Saudis were their physicians (62.4%), followed by their friends and family, and the media [41]. For physicians, the preferred source of information for prostate cancer was the internet (69.6%), followed by continuous medical education courses, textbooks, and peer-reviewed journals [57]. The percentage of men who underwent prostate cancer screening in Riyadh was very similar to the percentage recorded in Southwest Nigeria (10.2%) [41,59]. Although most of Jamaican men thought that prostate cancer screening may not help in early detection, 88% of them believed that screening, exercising, and engaging in activities are favorable to prevent prostate cancer [60].
4.5. Head and Neck Cancer
In Jeddah, 68% of participants in a cross-sectional survey indicated that they never received any information about HNC, which is consistent with the total knowledge score (57.8%) of undergraduate medical students about oral cancer prevention, which was below the expected standard (72%) [42,61]. For Saudi dental students, the knowledge score was higher (87.1%), and they were more confident than medical students to undergo systematic oral examination in order to detect any changes (87% vs. 28%) [61,62]. Saudi individuals in Jeddah identified dentists (33%) as a source of information on oral cancer; however, only 32.3% of dentists and physicians in Saudi Arabia assessed for oral cancer and 36% thought that this is attributable to their busy schedules and the high number of patients to be accommodated [42,63]. More than 37.6% of dentists and physicians in Saudi Arabia admitted their need for more training in order to prevent and detect oral cancer [63]. Similar to Saudi Arabia, a cross-sectional study performed in South Dakota among American Indians reported a total knowledge score of 26 out of 44 (59%) about HNC and demonstrated the feasibility of community-based screening program [64].
4.6. Implication of Cancer Screening
Cancer screening tests have been identified as an effective tool in the detection of preinvasive stages of cancer when it could still be curable. Some types of cancers have high prevalence in a preclinical state when detection is possible. In an early stage of cancer, suitable treatments can be applied. The availability of a good screening test is characterized by accepted sensitivity and specificity, low cost, and little direct harm to a given subject. Several cancers are suitable for screening because of their extensive morbidity and mortality. A little assessment of screening tests will help to define cancers that could be suitable for early intervention—i.e., breast, cervical, colorectal, prostate, and head and neck cancers. In conclusion, knowledge and awareness of cancer screening programs is poor among Saudi citizens. To overcome this challenge, the implementation of education programs and enhancement of awareness campaigns to educate the general public of the importance of undergoing these lifesaving programs, along with proposing rules and policies for the healthcare institutions that will require all healthcare providers to refer their patients to the appropriate cancer screening, is needed. Moreover, addressing the barriers mentioned in this review will help policymakers to develop strategic plans to overcome the financial and social barriers, and improve public perception and attitude toward performing cancer screening.
4.7. Limitations
This study is not devoid of limitations. We limited our review retrieval to PubMed, Embase, and Google Scholar search engines. Although we have done cross-referencing, which added a few studies in our review, we still cannot claim that we had access to all the relevant articles related to this topic in Saudi Arabia. In addition, all the studies that met the inclusion criteria were only cross-sectional. Furthermore, there was only one appropriate article each for HNC screening and prostate cancer screening that met our inclusion criteria.
5. CONCLUSION
A variety of cross-sectional studies that focused on cancer screening in different regions of Saudi Arabia were identified and included in this systematic review. These studies demonstrated that the majority of Saudi citizens had never been screened for cancer. Their sources of information about cancer screening were their physicians and the media. Most of the Saudi respondents in these studies were willing to be screened for cancer, but they were not aware about the screening tools for different types of cancers. Several factors affected the level of knowledge regarding cancer screening including age and educational level. Given the limited knowledge about cancer screening and willingness of Saudi population to be screened for cancer, there is a need for population-based interventions to fill the gap of knowledge and apply the primary prevention for cancer.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
REFERENCES
Cite this article
TY - JOUR AU - Demah AlAyadhi AU - Ghadah Alyousif AU - Afnan Alharbi AU - Zainab Alnjeidi AU - Ashraf El-Metwally PY - 2020 DA - 2020/07/02 TI - Systematic Review: Awareness, Knowledge, Attitude, and Practice of Cancer Screening Program in the Kingdom of Saudi Arabia JO - Dr. Sulaiman Al Habib Medical Journal SP - 151 EP - 161 VL - 2 IS - 4 SN - 2590-3349 UR - https://doi.org/10.2991/dsahmj.k.200626.001 DO - 10.2991/dsahmj.k.200626.001 ID - AlAyadhi2020 ER -
