Prevalence of Low Birth Weight in Urban Dhaka and its Association with Maternal Age and Socioeconomic Status
 , Medha Roy
, Medha Roy , Aklima Anny, Nelufa Yeasmin Shova, Tasmia Hema
, Aklima Anny, Nelufa Yeasmin Shova, Tasmia Hema
- DOI
- 10.2991/dsahmj.k.200905.001How to use a DOI?
- Keywords
- Low birth weight; mother’s age; Dhaka City; socioeconomic status
- Abstract
Low Birth Weight (LBW) is a major risk factor for neonatal and infant mortality worldwide. In 2015, the LBW rate was 22.6% in Bangladesh. The present study was conducted to estimate the rate of LBW in urban Dhaka and to observe its association with maternal age and socioeconomic status. This retrospective study was carried out at selected hospitals in Dhaka City. Birth weight, type of facility, mode of delivery and age of mothers of 736 babies born from 2014 to 2016 were collected from the recorded database of these facilities. Frequency analysis, bivariate analysis, with Chi-square test (χ2) and Pearson’s correlation were conducted as test of significance. The prevalence of LBW was 30.2% in Dhaka City, and the mean birth weight of neonates was 2.65 kg. The results of the study indicated that at least three children in every 10 live births are born with LBW in urban Dhaka. Younger maternal age (≤19 years) was significantly associated with LBW (p = 0.020). Pearson’s correlation found a weak positive linear relationship between mother’s age and birth weight of babies (r = 0.108; p = 0.01). Neonates from government facilities, representing the lower socioeconomic group, had a significantly higher LBW rate. The findings of the study will help to initiate preventive programs and to develop public health nutrition interventions to reduce LBW in Bangladesh.
- Copyright
- © 2020 Dr. Sulaiman Al Habib Medical Group. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Low Birth Weight (LBW) has been defined by the World Health Organization (WHO) as weight at birth of <2500 g [1]. The global LBW prevalence is 15.5% [2]. In 2015, 20.5 million LBW babies were born worldwide, and 47% of these babies were in South Asia [3]. According to WHO, 60–80% of all neonatal deaths indirectly occur as a result of LBW [2]. The infants who survive face lifelong consequences including a higher risk of stunted growth [4], impaired cognitive function [5], and adult-onset chronic conditions such as obesity, diabetes [6], and renal disease [7].
Low birth weight is a multifactorial condition but the immediate cause responsible is either Intrauterine Growth Restriction (IUGR) or preterm birth (born prior to 37 weeks of pregnancy), or both [8]. Infants with a birth weight and/or birth length below the 10th percentile for gestational age are diagnosed with IUGR and labeled small for gestational age [9]. Although preterm birth and IUGR have different etiologies, low weight gain during pregnancy (<9.1 kg), short stature (<155 cm), and stress have been reported to be common risk factors for both outcomes [10].
The primary cause of IUGR is placental insufficiency or inadequate uterine blood flow [11]. Nonplacental risk factors of IUGR include decreased oxygen carrying capacity, maternal malnutrition, teratogens, short inter pregnancy intervals, race, maternal age, low pre-pregnancy Body Mass Index (BMI) (<18 kg/m2), smoking during pregnancy, and low socioeconomic status. The fetal etiologies of IUGR consist of genetic diseases, congenital malformations, infections, multiple gestations, and placental/cord abnormalities [10,12].
Risk factors for preterm birth include high BMI (>25 kg/m2), heavy physical activity, history of previous abortion or previous Cesarean Section (C-section), shorter cervical length, abnormal uterine Doppler flow, pre-pregnancy marijuana use, Caucasian ethnicity, family history of diabetes and/or preeclampsia, family history of LBW babies, longer time to conceive, hormonal fertility treatment (excluding clomiphene), mild hypertension, family history of recurrent gestational diabetes, and maternal family history of any miscarriage [13,14].
In Bangladesh, nearly half of newborns are not weighed at birth. According to the Multiple Indicator Cluster Survey (MICS) 2019, the percentage of children weighed at birth is only 52% in Bangladesh [15]. On top of that, only a limited number of reports demonstrated birth weight prevalence in this country from time to time. The LBW rate was 36% in 2004, 37.7% in 2012–2013 [16], and 22.6% in 2015 [17], according to the National LBW Survey (NLBWS) 2003–2004, MICS 2012–2013 and NLBW 2015 (published in April, 2017), respectively. The MICS 2019 documented the crude LBW rate to be 14.8% and it was also noted as a likely underestimate of true LBW prevalence [15]. Besides limited surveys on true LBW prevalence, studies exploring the associating factors of LBW regarding Bangladesh are also very few in number, which led us to our study. The aim of the study was to find out the current rate of LBW in urban Dhaka and evaluate the association of LBW with factors, namely, maternal age and socioeconomic status.
2. MATERIALS AND METHODS
2.1. Design and Setting of the Study
This retrospective descriptive study was conducted by analysis of birth weight related variables in different regions of Dhaka City. Neonates from six selected hospitals in two city corporations in Dhaka City—Dhaka North City Corporation and Dhaka South City Corporation—constituted the study population. From each city corporation, three hospitals were selected for data collection so that the entire city can be represented (Figure 1). This study was conducted over 4 months starting from June 2016 to September 2016.
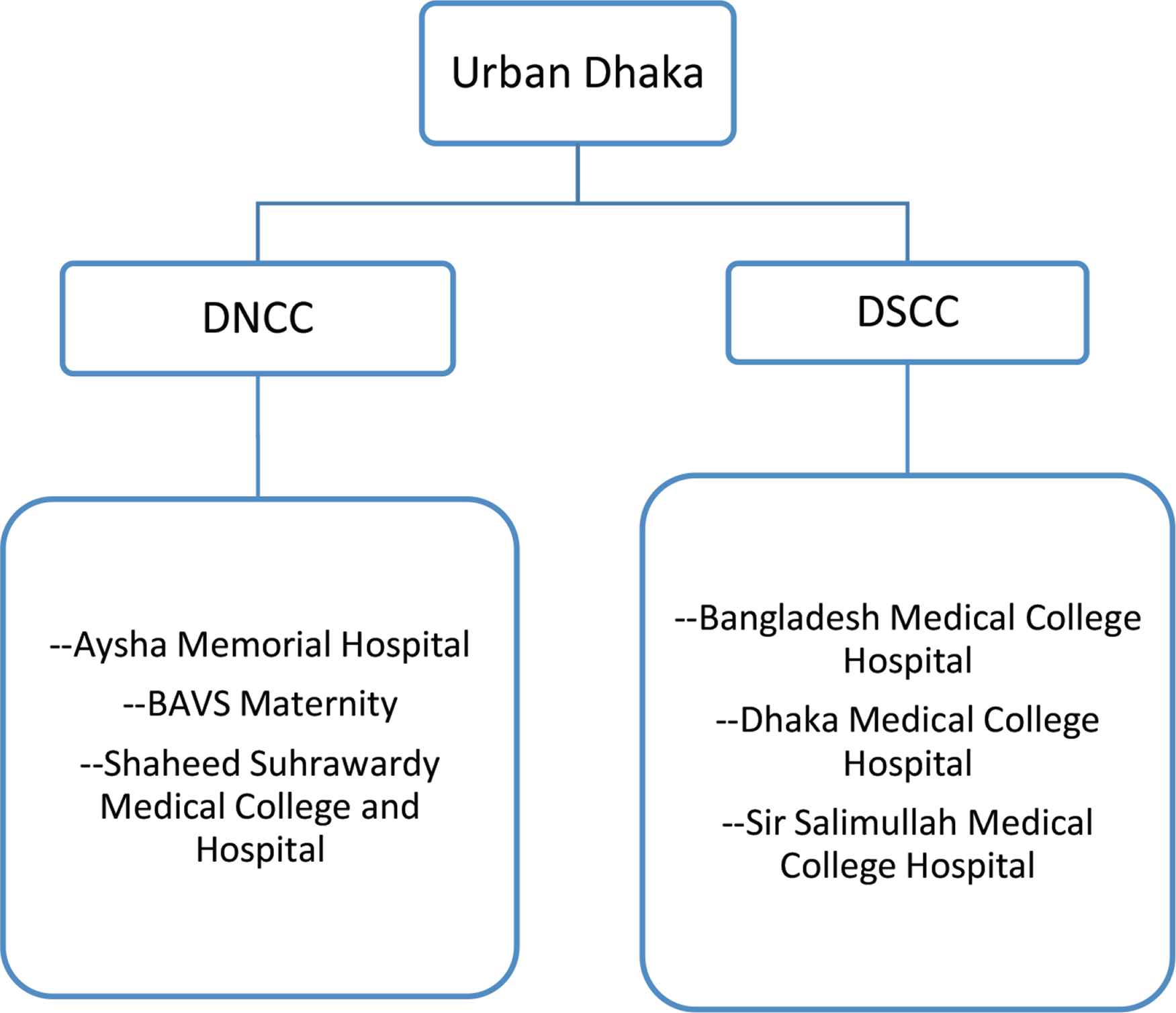
Selected hospitals from two city corporations. Three selected hospitals from each city corporation—Dhaka North City Corporation (DNCC) and Dhaka South City Corporation (DSCC).
2.2. Description of Materials
Birth-related data of 736 singleton neonates born over the period of 2014–2016 in selected hospitals were extracted for the study. Weight of the newborn baby, age of the mother, mode of delivery, and type of facility used for delivering the baby were the outcome variables. The type of facility used for childbirth, that is, government and nongovernment hospitals, was selected as representative of two socioeconomic classes of the population, namely, high socioeconomic status and low socioeconomic status. In Bangladesh, the cost of childbirth service is significantly higher in private hospitals than in government hospitals [18]. Nonetheless, mothers in the higher socioeconomic group, who have access to private facilities, usually avoid going to government-run facilities because of the poor quality of service in such hospitals [19]. As a result, the poorer segments of the population are the major beneficiaries of government healthcare facilities [20]. This attribute served the purpose of socioeconomic classification of our sample.
2.3. Processes
Sample size was calculated to estimate the prevalence of LBW with a precision of 0.25% at 5% statistical significance. Our target sample size was 736 after adjusting the design effect for two cluster zones, based on 90% power to detect a 36% prevalence of LBW. Initially, ethical approval was granted by the National Research Ethics Committee of Bangladesh Medical Research Council after we had submitted a detailed research proposal. Next, official written permission for data collection from hospital records was obtained from both the Director and Department of Gynecology and Obstetrics of the selected hospitals. The authors of this study, a researcher team of five, collected data themselves. Sequential data of outcome variables of the children born from 2014 to 2016 in the selected hospitals were collected using a structured questionnaire form.
2.4. Statistical Analysis
Bivariate analysis with Chi square test (χ2) was used to test the association between birth weight and type of hospital, mother’s age, and mode of delivery, separately. Pearson’s correlation was done to test the correlation between birth weight and mother’s age. We conducted all the analyses using IBM SPSS version 23 (IBM Corporation, Armonk, NY, USA). Statistical significance was set at p < 0.05.
3. RESULTS
A total of 736 neonates and their mothers were enrolled as participants in this study. Maternal age ranged from 15 to 45 years. The mean age of the mothers is 24.7 years with a Standard Deviation (SD) of ±5. The neonates’ mean (±SD) birth weight was 2650 ± 615 g. Slightly less than one-third of the neonates (30.2%) had LBWs (<2500 g) and 3.7% weighted <1500 g at birth. About two-thirds of the samples were taken from government facilities representing the population of low socioeconomic status. The number of babies of both sexes was almost equal. Nearly three-quarters of the babies were born via normal vaginal delivery.
Table 1 presents the basic characteristics of participants, who were divided into two groups: women with infants of normal birth weight (≥2500 g) and LBW (<2500 g). By using Pearson’s Chi-square test, significant association of birth weight with maternal age, type of facility, and mode of delivery was found. About 16% of the mothers were adolescent (≤19 years), and the rest represented all age groups. The LBW rate was highest (41%) in this group. This association between birth weight and younger maternal age was found to be statistically significant (χ2 = 7.808; p =0.020). The LBW rate in nongovernment hospitals was 17%, whereas in government facilities, this rate was 38%. The LBW rate is significantly higher in government hospitals than in private hospitals (χ2 = 37.244; p ≤ 0.001). In contrast to 27.6% LBW in normal vaginal delivery, the LBW rate is 37.2% in C-section deliveries. Association between mode of delivery and birth weight was also found to be statistically significant in Chi-square test (χ2 = 6.386; p = 0.012).
| Determinants | Frequency, n (%) | Normal weight, n (%) | Low birth weight, n (%) | p-value |
|---|---|---|---|---|
| Maternal age group (years) | ||||
| ≤19 (adolescent) | 117 (15.9) | 69 (59) | 48 (41) | |
| 20–35 (adult) | 604 (82.1) | 434 (71.9) | 170 (28.1) | |
| ≥36 (advanced age) | 15 (2) | 11 (73.3) | 4 (26.7) | |
| Total | 736 (100) | 514 (69.8) | 222 (30.2) | 0.020 |
| Type of facility used | ||||
| Nongovernment hospital | 267 (36.3) | 223(83.5) | 44 (16.5) | |
| Government hospital | 469 (63.7) | 291 (62) | 178 (38) | |
| Total | 736 (100) | 514 (69.8) | 222 (30.2) | <0.001 |
| Mode of delivery | ||||
| Normal vaginal | 537 (73) | 389 (72.4) | 148 (27.6) | |
| Cesarean | 199 (27) | 125 (62.8) | 74 (37.2) | |
| Total | 736 (100) | 514 (69.8) | 222 (30.2) | 0.012 |
Basic characteristics of the participants by normal and low birth weight (n = 736)
Figure 2 gives an overview of the percentage of LBW in different hospitals of Dhaka City. The LBW rate was highest in Shaheed Suhrawardy Medical College Hospital (a free government hospital) and lowest in Bangladesh Medical College Hospital, which is private and requires payment for service.
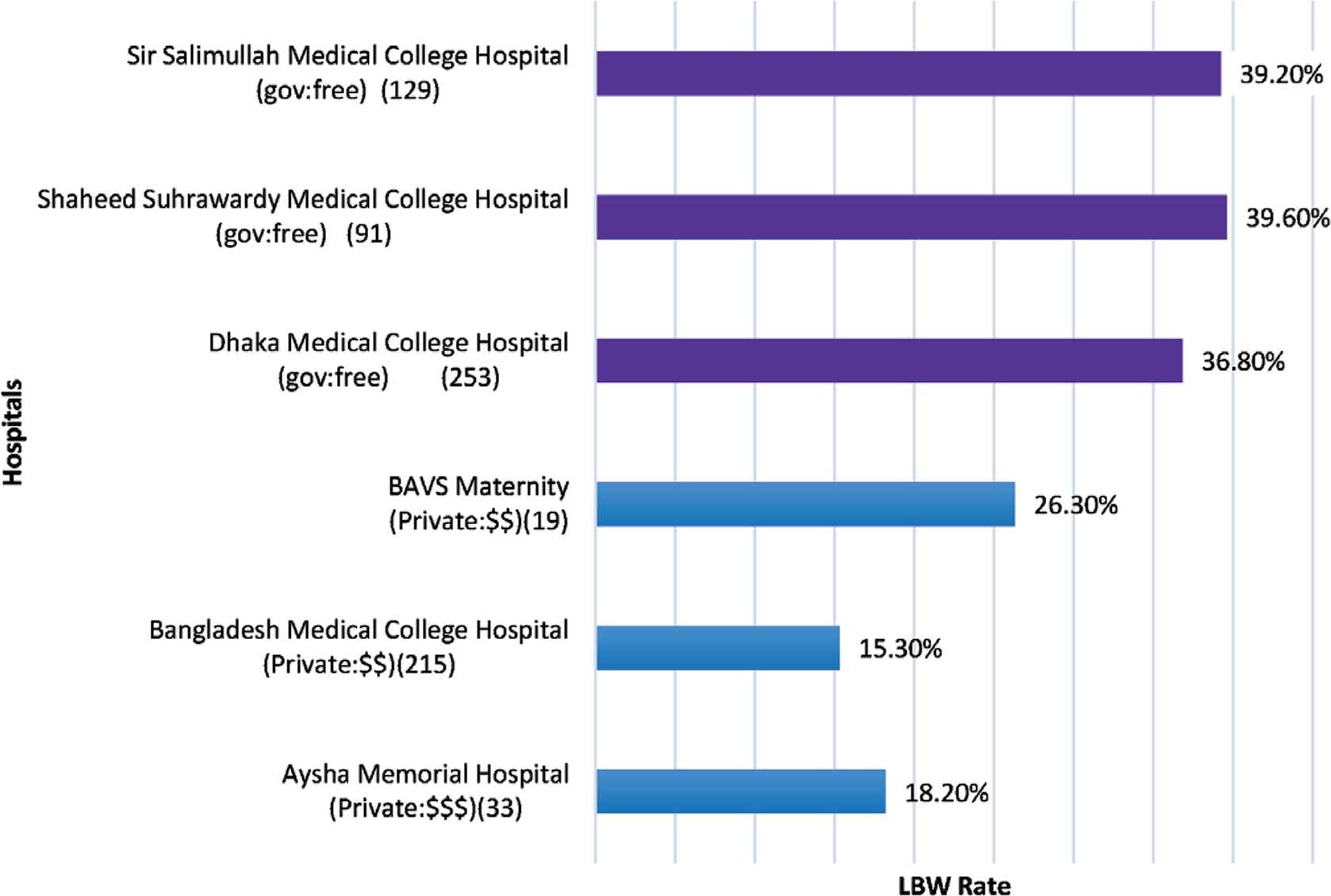
Low Birth Weight (LBW) rate at different hospitals. Illustration of the LBW rates along with manegarial body, service cost, and sample number from selected hospitals.
Pearson’s correlation was conducted between mother’s age and birth weight. A weak positive correlation was found between these two variables, which was significant at 0.01 level (r = 0.0108), as shown in Figure 3.
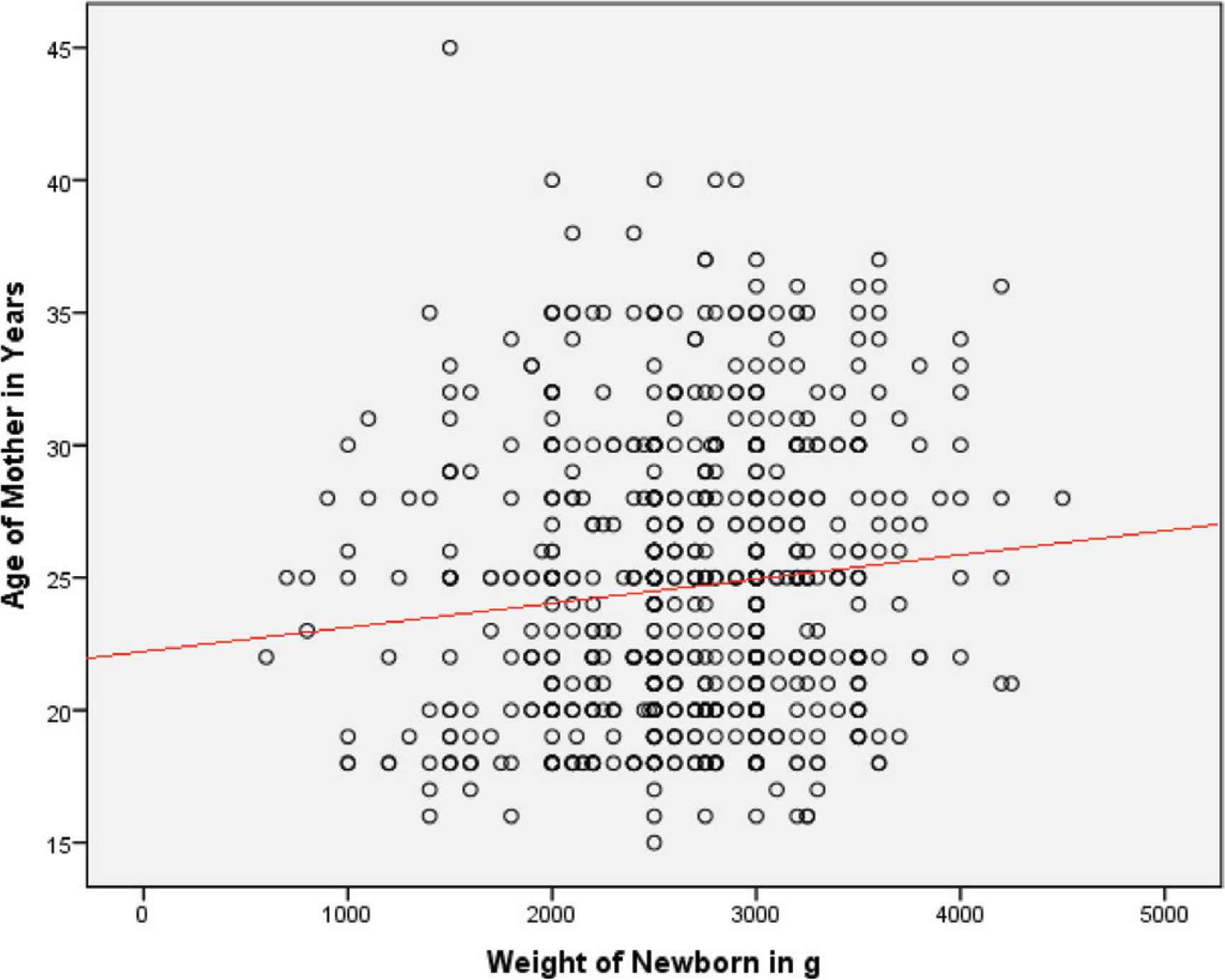
Correlation between mother’s age and birth weight. Mother’s age and birth weight have a weak positive correlation (r = 0.108).
4. DISCUSSION
This was a retrospective descriptive study portraying the picture of birth weight status in urban Dhaka. Our presented data differ from the available data in this country. The LBW rate found in this study is lower than that of the NLBWS 2004 but higher than that of the NLBWS 2015. In contrast to 30.2% LBW in urban Dhaka, the first and second National LBW Survey of Bangladesh, respectively, found this rate to be 43.7% in 2004 and 24.5% in 2015 [16]. We found the mean birth weight to be 2649.71 g, which contrarily is lower than that of the NLBWS 2015 (2898 g). Compared to global 2015 data, the prevalence of LBW was 16.4% in our neighboring country, India [21], 7% in high income regions (Northern America, Europe, Australia, and New Zealand), and 26.4% in Southern Asia [22]. Southern Asia is one of the regions with the highest burden of LBW. Being a country in this region, the LBW rate is high in Bangladesh compared to both developed and developing countries.
We found that younger maternal age (≤19 years) was associated with increased risk of LBW. The result of our study is in accordance with that of a recent case control study in India, in which maternal age is younger than 19 years was identified to be a risk factor of LBW by univariate regression analysis [23]. However, our result partially complied with those of two large cohort studies. Lawlor et al. [24], in a population of Danish women, found a U-shaped relationship between maternal age and risk of preterm birth, with the lowest risk age at 24–30 years. A more recent study in Canada found similar results, in which both younger age (20–24 years) and advanced maternal age (40 years and over) was associated with an increased risk of preterm birth [25]. Owing to the small number of samples (2%) from the advanced maternal age group, this criterion remained unexplored in our study.
There was a total of 469 (64%) mothers from government hospitals, where child delivery services are almost free of charge and hence preferred by rural or low socioeconomic communities. As the type of facilities used in childbirth represents socioeconomic status of the respective families in Bangladesh, the association between type of hospital and birth weight is interpreted as association between birth weight and socioeconomic status. Neonates born in government facilities had significantly higher LBW rate than those born in private facilities. Our results are consistent with those of previous studies from both developed and developing countries. Manyeh et al. [26] demonstrated significant association between LBW and socioeconomic status of household in a large population of 6777 mothers in southern rural Ghana [26]. Another study in the United States reported that birth weight increases with earned income tax credits [27]. It is evident that working conditions have an adverse effect on pregnancy outcome [28]. In a recent case–control study, working conditions were considered as socioeconomic parameters and unfavorable working conditions, characterized by manual labor and long working hours in particular, were associated with preterm birth among Cypriot women [29].
We found that the LBW rate was significantly higher in the C-section deliveries, as proven earlier [30]. The reason behind these C-section deliveries, however, is not recorded and remains unclear. In fact, conducting unnecessary C-section deliveries for financial gain is a common scenario in Bangladesh [31], for which institutional C-section deliveries are alarmingly increasing in the country [32]. Authors from a previous study suggested that elective C-section may be associated with LBW among full term infants [33].
A strength of this work is that this LBW study has a large sample size of 736 births from Dhaka City. Inclusion of births from both government and nongovernment facilities from two different City Corporations of Dhaka constituted a representative population for our study. Because we extracted the data directly from hospital databases, which is documented by medical professionals, the quality of our data is also a strength.
Nevertheless, the design of the current study is subject to limitations as with the majority of studies. Because it was a facility-based study, home births were excluded from the design. Another potential limitation is the unexplored area of advanced maternal age owing to scarcity of samples. Also, we could not differentiate between premature and small for gestational age babies owing to lack of information on hospital databases, which can be considered a weakness of this work.
5. CONCLUSION
The results of the study indicated that at least three children in every 10 live births are born with LBW in urban Dhaka. The teenage mothers experienced significantly more LBW babies than the adult mothers. The findings of the study will help to initiate preventive programs and to develop public health nutrition interventions to reduce LBW in Bangladesh.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
This study was designed by all of the author’s discussion. RS directed the study, conducted literature search and wrote the manuscript. MR, AA, NYS and TH contributed to data collection and data entry. All authors discussed the results and contributed to the final manuscript.
FUNDING
This study was completely funded by the authors themselves. No financial aid was received from any institution or individual.
ACKNOWLEDGMENTS
The authors gratefully acknowledge technical support from Nutrition Foundation Bangladesh (NFB) and supervisory support from College of Home Economics, Azimpur, Dhaka.
Footnotes
Data availability statement: The datasets generated and/or analyzed during the current study are available in the Birth Weight Data repository (https://doi.org/10.6084/m9.figshare.12315734.v1).
REFERENCES
Cite this article
TY - JOUR AU - Razia Shaheen AU - Medha Roy AU - Aklima Anny AU - Nelufa Yeasmin Shova AU - Tasmia Hema PY - 2020 DA - 2020/09/10 TI - Prevalence of Low Birth Weight in Urban Dhaka and its Association with Maternal Age and Socioeconomic Status JO - Dr. Sulaiman Al Habib Medical Journal SP - 162 EP - 166 VL - 2 IS - 4 SN - 2590-3349 UR - https://doi.org/10.2991/dsahmj.k.200905.001 DO - 10.2991/dsahmj.k.200905.001 ID - Shaheen2020 ER -
