Racial differences in relation between carotid and radial augmentation index☆
Grant support: JSPS Postdoctoral Fellowships for Research Abroad (JS) and NIH grant AG20966 (HT).
- DOI
- 10.1016/j.artres.2009.12.002How to use a DOI?
- Keywords
- Reflection wave; Applanation tonometry; Race; Central blood pressure
- Abstract
Background: Augmented central artery wave reflection is a cardiovascular disease risk factor. Augmentation index (AI) obtained from peripheral artery waveforms provides qualitatively similar information to AI from central artery waveforms. Little information is available, however, regarding the influence of racial difference in association between central and peripheral AI.
Methods: We studied 47 White adults (45 ± 17 yr, 20 women) and 94 age-matched Asian adults (45 ± 14 yr, 42 women).
Results: The White group was significantly taller than the Asian group, whereas there were no significant group differences in blood pressure and heart rate. Carotid and radial AI tended to be lower in White compared with Asian adults (P < 0.10 for both). Such tendency disappeared when the difference in height was taken into account using ANCOVA (P = 0.84 and P = 0.77, respectively). Radial AI was strongly and positively correlated with carotid AI in White adults (r = 0.75, P < 0.0001) as well as in Asian adults (r = 0.82, P < 0.0001). The slope and intercept of linear regression line between radial and carotid AI of White adults were highly comparable with those of Asian adults.
Conclusion: AI in the conveniently located peripheral vasculature may provide a surrogate measure of central AI irrespective of difference in race (e.g., Asian vs. White populations).
- Copyright
- © 2009 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Introduction
Augmented wave reflection in the central artery is an important determinant of cardiovascular risk,1–3 and augmentation index (AI) is a well-established indicator of arterial wave reflection.4 However, the acquisition of arterial pressure waveforms required for AI is difficult to perform in the central arteries (e.g., the aorta, carotid artery). Accordingly, many investigators have adapted the measurement of AI on the radial arteries and have used it to gain insight into carotid or aortic AI.5–7 The available evidence is encouraging in this line of research, but it is not clear if the relation between radial artery AI and central artery AI is influenced by the race or ethnic status. This is critical in order for this technique to have a greater generalizability. Accordingly, the purpose of this study was to determine the influence of race (more specifically, Whites and Asians) on association between radial AI and carotid AI.
Methods
Subjects
Forty-seven white adults and 94 age-matched Asian adults (1–2 ratio match up of subject samples) who were free of overt cardiovascular diseases were studied after at least 4 h of fasting and abstinence from caffeine. This study was reviewed and approved by the local Institutional Review Board, and all subjects signed the informed consent.
All measurements were performed after an abstinence of caffeine and a 3-h fast. After resting for at least 15 min in a quiet, temperature-controlled room, carotid and radial arterial AI were measured in a random order by two different vascular testing devices. Carotid arterial waveforms were recorded on the automatic device (VP-2000, Colin Medical Technology, San Antonio, TX) in duplicate using an arterial applanation tonometry probe incorporating an array of 15 micropiezoresistive transducers on the left common carotid artery with a collar, which is able to hold the probe on the carotid artery by an optimal constant pressure. The systolic foot (diastolic pressure), shoulder, and peak (systolic pressure) of carotid arterial pressure waveforms were automatically detected by using algorithms based on a band-pass filtering (5–30 Hz) and fourth derivatives8 (Fig. 1). The band-pass filtering was performed in order to eliminate artifacts. Carotid AI was calculated as follows:
Radial AI was measured using an applanation tonometry-based automated radial AI measurement device (HEM-9010AI; Omron Healthcare, Kyoto, Japan). The arterial applanation tonometry probe, incorporating an array of 40 micropiezoresistive transducers, was held on the left radial artery while pressure against the radial artery was automatically modulated in order to obtain an optimal radial arterial waveform. Systolic foot (e.g., diastolic pressure) and the first and second systolic peaks were automatically detected using fourth derivatives for each radial arterial waveform and averaged. Radial AI was calculated as follows:
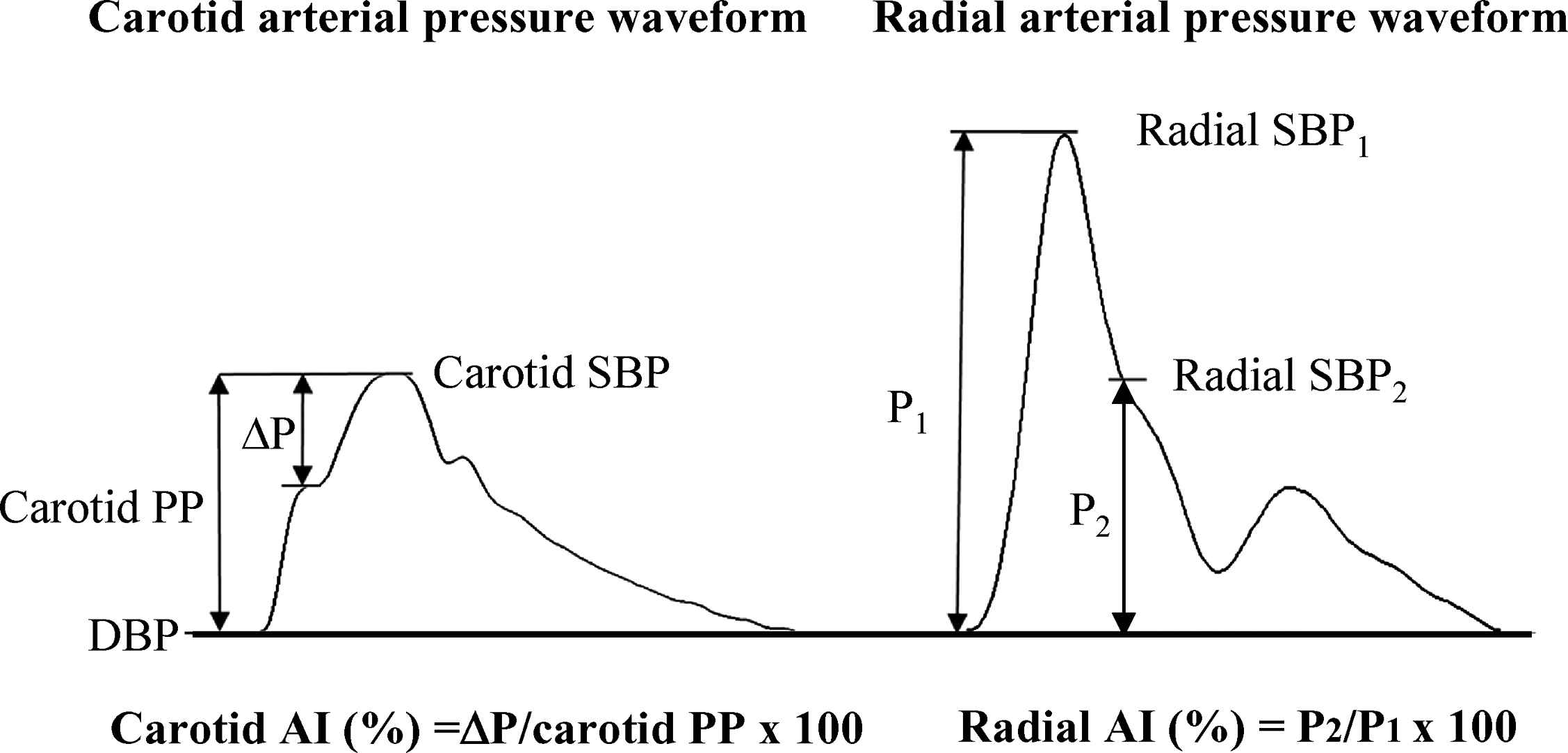
Augmentation index (AI) (left: carotid artery; right: radial artery). SBP = systolic blood pressure, DBP = diastolic blood pressure, PP = pulse pressure, P1 = first systolic peak – DBP, P2 = second systolic peak – DBP.
Unpaired t-test and ANCOVA were performed to compare variables of interest between groups. Univariate correlation analysis and Bland–Altman plots were used to assess relationships between variables of interest. The effect of the race on the relation between carotid and radial AI was assessed by a general linear regression model.
Results
White adults were significantly taller and heavier than Asian adults, whereas no significant group differences were observed in blood pressure and heart rate (Table 1). Carotid and radial AI tended to be lower in white compared with Asian adults (P < 0.10 for both). However, such tendency was disappeared when the difference in height was taken into account using ANCOVA (P = 0.84 and P = 0.77, respectively).
| Asian | White | P-value | |
|---|---|---|---|
| N, male/female | 52 / 42 | 27 / 20 | n.s. |
| Age, yrs | 45 ± 14 | 45 ± 17 | n.s. |
| Height, cm | 166 ± 8 | 171 ± 10 | < 0.01 |
| Body mass, kg | 63 ± 12 | 73 ± 15 | < 0.0001 |
| BMI, kg/m2 | 22.9 ± 3.0 | 25.1 ± 4.4 | < 0.001 |
| Heart rate, bpm | 61 ± 9 | 60 ± 10 | n.s. |
| Systolic BP, mmHg | 117 ± 10 | 120 ± 16 | n.s. |
| Diastolic BP, mmHg | 71 ± 8 | 69 ± 9 | < 0.10 |
| Mean BP, mmHg | 88 ± 8 | 88 ± 11 | n.s. |
| Carotid AI, % | 9.3 ± 18.0 | 3.4 ± 21.5 | < 0.10 |
| Radial AI, % | 75.9 ± 15.9 | 70.8 ± 17.0 | < 0.10 |
| ΔAI, % | 66.5 ± 10.3 | 67.3 ± 14.1 | n.s. |
Data are mean ± SD. BMI = body mass index, BP = blood pressure, AI = augmentation index.
ΔAI = Radial AI – Carotid AI.
Physical characteristics.
Radial AI was correlated with carotid AI in White adults (r = 0.75, P < 0.0001) and in Asian adults (r = 0.82, P < 0. 0001) (Fig. 2). The regression line for White adults (y = 0.95x−64.1, black line) was almost superimposed on that for Asian adults (y = 0.93x−60.9, gray line). As seen in Bland–Altman plots, the differences between radial and carotid AI were not different between White and Asian adults (66.5 ± 10.3% vs. 67.3 ± 14.1%, P = 0.71, Fig. 2).
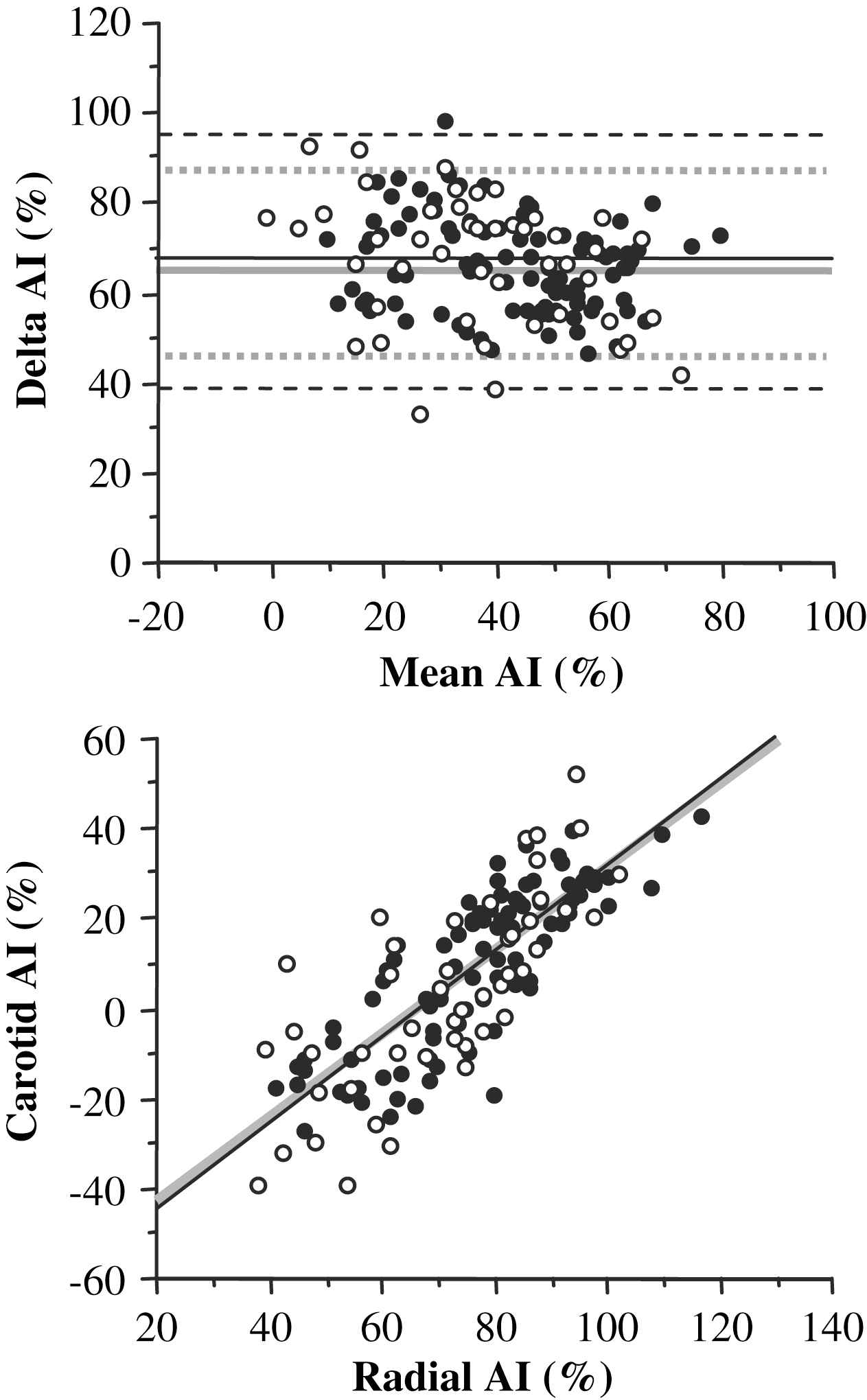
(Top) Relation between carotid augmentation index (AI) and radial AI in Asian (closed circles) and White (open circles) adults. Asian (gray line): y = 0.93x–60.9, r = 0.82, P < 0.0001; White (black line): y = 0.95x–64.1, r = 0.75, P < 0.0001. (Bottom) Bland and Altman’s Plots between carotid AI and radial AI in Asian and White adults. Mean differences were 66.5 ± 10.3% in Asian (gray lines) and 67.3 ± 14.1% in White (black lines).
In the pooled subjects, general linear regression model reveled that radial AI (beta = 0.57, P < 0.0001) and age (beta = 0.17, P < 0.01) were significant independent correlates for carotid AI (R2 = 0.71, P < 0.0001), whereas race, sex, height, body weight, body mass index, heart rate, and blood pressure were ejected from the model by not being independently significant.
Discussion
Increase in central artery wave reflection is gaining a reputation as a risk factor for cardiovascular disease. Because of its clinical importance, the development of promising noninvasive techniques to screen high-risk patients is desirable. We and others have reported that radial AI, which is easier to measure and implement, may be able to provide qualitatively similar information to carotid AI.5–7 These relations have been observed in some populations, including general populations5,6 and medicated hypertensive populations.7 The results of the present study extend these previous by suggesting that these relations can be extrapolated to different racial populations, including Whites and Asians.
A cohort study composed of monozygotic and dizygotic female twin pairs indicated that AI has significant hereditable component (approximately 37% of total variation in AI).11 These results imply that genetic components might affect association between carotid and radial AI. Contrary to this hypothesis, radial AI was significantly correlated with carotid AI similarly in both White and Asian groups. Furthermore, the Bland–Altman plot revealed that differences between radial and carotid AI of White adults were highly comparable with those of Asian adults. General linear regression model reveled that radial AI and age were significant independent variables for carotid AI, whereas race, sex, height, body weight, body mass index, heart rate, and blood pressure were ejected from the model by not being independently significant. These results suggest that the race does not affect the relation between carotid and radial augmentation index.
To our knowledge, this is the first study to assess the effect of race on association between measures of arterial wave reflection evaluated from central and peripheral arterial pulse waves. In the present study, carotid and radial AI tended to be greater in Asian subjects than in White subjects. This group difference was primarily due to the smaller height in Asian subjects compared with White populations as the group difference was disappeared when height was taken into account. AI, measure of central wave reflection, is influenced by various factors (i.e., sex, aging, height, arterial stiffness, heart rate, blood pressure).6,12–15 Since shorter height is associated with the smaller length from the heart to major wave reflection sites16,17 and earlier return of reflection waves from periphery to the heart, a person, who has short stature, tends to exhibit a greater AI. East-Asian is known to be smaller in height than Caucasian or other white populations,18,19 and this was reflected in our study sample.
There is an increasing recognition that central systolic and pulse pressure is more relevant than peripheral (brachial) measure for the prediction and pathophysiology of cardiovascular disease.20 Several investigators indicated that the late systolic peak of peripheral (radial) pressure wave closely approximates central (aortic) systolic pressure.21–24 Our present results extend these findings by showing that the association between central and peripheral AI is similar in different racial populations. Hence, peripheral AI reflects the ratio between central and peripheral pulse pressure.21 It is important to emphasize that radial AI derives information about central wave reflection and central pulse pressure without using the general transfer function.
In conclusion, measurement of AI in the conveniently located peripheral vasculature may provide a surrogate measure of central AI irrespective of difference in the race. Future cross-sectional studies comparing the Black adults (not studied in the present study) with other populations (Whites, Asians, etc.) as well as future prospective longitudinal studies to clarify the relation between radial AI and the morbidity and mortality of cardiovascular disease are warranted.
Acknowledgements
This work was supported by JSPS Postdoctoral Fellowships for Research Abroad, and NIH grant AG20966. The AI measurement device tested for the present study was kindly provided by the Omron Healthcare Corporation, Kyoto, Japan.
References
Cite this article
TY - JOUR AU - Jun Sugawara AU - Hidehiko Komine AU - Mutsuko Yoshiwaza AU - Takashi Tarumi AU - Seiji Maeda AU - Hirofumi Tanaka PY - 2010 DA - 2010/01/25 TI - Racial differences in relation between carotid and radial augmentation index☆ JO - Artery Research SP - 15 EP - 18 VL - 4 IS - 1 SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2009.12.002 DO - 10.1016/j.artres.2009.12.002 ID - Sugawara2010 ER -
