Acute and chronic effects of acupuncture on radial artery: A randomized double blind study in migraine
- DOI
- 10.1016/j.artres.2009.12.003How to use a DOI?
- Keywords
- Acupuncture; Radial artery; Migraine; Hemodynamics; Randomized trial
- Abstract
Background: Acupuncture is an accepted treatment for migraine. Palpation of the radial pulses is one of the most important techniques in traditional Chinese medicine both for diagnosis and monitoring of treatment efficacy. The objective of the present study was to investigate the acute and chronic effects of acupuncture on the radial artery of patients suffering from severe migraine.
Methods: A double-blind parallel group study was conducted in 31 patients never exposed to acupuncture and randomized in two groups : real acupuncture versus sham acupuncture, applied 3 times at one month interval. At baseline and after 2 months, radial artery diameter was measured with a high resolution echotracking system before and during a 20 min’s acupuncture session. Migraine severity was assessed by self administrated questionnaires and visual analogic scale for pain at each visit. Patients and investigators (not acupuncture physician) were blinded as to the treatment allocation.
Results: During the first session, radial artery diameter significantly increased after real acupuncture, (+3.1% IQR [−3.2–8.5], P = 0.03 vs 0.9% IQR [−5.3–5.8], P = NS), and remained significantly higher after the two months treatment course 5.2% IQR [−3.9–14] vs. −4.4% IQR [−10.0–3.5], respectively; P < 0.01). Patients with the most severe pain at baseline were less prone to dilate their arteries during follow-up (P < 0.05). A larger arterial vasodilatation after real acupuncture was observed for any given level of pain intensity (P < 0.01).
Conclusion: an acupuncture-induced vasodilatation was observed at the site of the radial artery in patients suffering from severe migraine and naïve to acupuncture. The vasodilatation was maintained after chronic treatment.
Condensed abstract: This double-blind randomized, controlled trial aimed at showing the acute and chronic vasodilatory response to acupuncture in migrainers naïve to acupuncture. We show that real acupuncture is accompanied by acute and chronic vasodilation of the radial artery, the chronic vasodilation is inversely related to the level of pain at baseline.
- Copyright
- © 2010 Published by Elsevier B.V. on behalf of Association for Research into Arterial Structure and Physiology.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Introduction
Despite its alleged irrational principles,1 acupuncture is the most frequent type of unconventional medicine in developed countries,2,3 but with little objective benefit reported in controlled studies.4 Traditional Chinese medical syndromes, treated by acupuncture, are diagnosed by recorded history and symptoms, together with examination of the tongue and the pulses at both radial arteries.4 Acupuncture therapy is adjusted according to the observed alterations of the radial pulses, and monitored through changes in radial pulse patterns on an individual basis. However, the changes in radial artery diameter have never been objectively measured before a randomized double-blind study that we conducted several years ago.5 Vasodilatation was observed only in patients suffering from pain and previously exposed to acupuncture, and not in healthy volunteers, naïve to acupuncture.5 We thus raised the hypothesis that either sensitization by repeated acupuncture sessions or a high chronic level of pain was necessary to observe acupuncture induced-vasodilatation.
Migraine is a chronic disease with periodic exacerbation of pain during attack. Migraine is considered benign, yet it is a devastating disease in which acupuncture has been demonstrated to be more efficient and cost-saving than placebo.6,7 Moreover, migraine is characterized by an inadequate vasoreactivity in meningeal and cerebral arteries.8 To test these hypotheses, we studied the effects of acupuncture on radial artery diameter in patients naïve for acupuncture, suffering from chronic migraine, during a 2 month course of acupuncture. We thus designed a randomized, double-blind, parallel group clinical trial in order to study radial artery diameter in response to acute and chronic acupuncture, by comparison to sham acupuncture, and to determine whether radial artery vasodilatation was related to pain intensity.
Methods
Patients and experimental design
34 patients were recruited through the “migraine outpatient clinic” of the anesthesiology ward of Hôpital Européen Georges Pompidou. Patients fulfilled the definition of migraine without aura, according to the criteria of the International Headache Society.9,10 Selection criteria included an age of 18–60 years; a severe migraine (>6 attacks per month and/or with severe interference with daily life); migraine symptoms resistant to a first line chronic treatment and stabilization of favoring or associated conditions before entry into the study. Exclusion criteria were any life threatening condition, any acupuncture treatment within the previous year, migraine with aura, or pure catamenial migraine. Prophylactic treatments were kept constant throughout the study duration.
Real acupuncture therapy was given by a French physician (R.C.) trained in both “orthodox” western medicine together with traditional Chinese medicine. Disposable stainless steel needles 4.0 cm in length (European Marco Polo company, Albi, France) were used. The diagnostic workup before acupuncture included recording of medical history and symptoms, together with examination of the tongue and the pulses at both radial arteries, according to the Chinese medicine principles. Acupuncture therapy was adjusted according to the perceived alterations of the radial pulses, and monitored through changes in radial pulse patterns (which are the only signs to change acutely during the acupuncture session). Acupuncture therapy was delivered as previously published.5 In the case of real treatment, acupuncture needles were inserted into so-called specific acupuncture points corresponding to the established diagnosis. The physician (R.C.) aimed at achieving “de Qi” (in which patients experienced an irradiating feeling considered to be indicative of effective needling), and needles were stimulated manually by rotation in each direction (until de Qi is obtained) at the beginning of each session and remained untouched until the end of the session. No additional electrical or laser stimulation was used. In the case of sham treatment, insertion points were chosen outside the specific acupuncture points. In both cases, needles were maintained in place for 20 min, and removed thereafter. “Sham treated” patients were assessed in the same ways, were given the same amount of attention, and received the same number of needles, which were left for the same length of time, as their pairs. The only difference was that needles were inserted into non-acupuncture “dead” points. The trial was truly double-blind since both patients and clinical investigators (P.B., B.L. and S.L.) measuring radial artery parameters were strictly blinded to the real or sham character of the acupuncture therapy. The practitioner of traditional Chinese medicine (R.C.) assessed each patient individually in a separate room before each treatment, then opened a sealed envelop (the random list was computer-generated) informing him whether real or sham acupuncture treatment should be given.
Hemodynamic measurements
The measurements were performed in a quiet room with a stable ambient temperature of 24 ± 1 °C. Blood pressure and radial artery hemodynamic parameters were studied with the subject in the supine position and after a rest of at least 20 min. Brachial blood pressure was monitored every 3 min with an oscillometric method (Dinamap model 845, Critikon) during the whole investigation.
Measurements of radial artery internal diastolic diameter and stroke change in diameter were obtained with a 10 MHz ultrasound system analyzing the RF signal (NIUS 02; SMH, Bienne, Switzerland), as previously described, validated, and used in clinical studies.11–14 Only diastolic diameter was used. Measurements were performed over 3 min by a single investigator, highly trained at measurements (B.L.), before the insertion of the needles, then during min 7–10, and min 17–20 after insertion. For practical reasons, the right radial artery was selected for diameter measurements. Reproducibility of radial artery diameter has been published before in our unit, the standard deviation for intra-investigator intersession was 130 μm, coefficient of variation 5.6%.13 Reproducibility was thoroughly tested in our unit to the same level.
Migraine assessment
Patients were assessed by an experimented anesthesiologist (C.V.), in charge of the migraine consultation. After baseline evaluation, patients were asked to fill a diary notebook in which they had to report all headache characteristics, using predefined scales.15 Frequency, intensity (visual analogic scale – VAS – 0 (no pain) to 10 cm (maximal pain) and duration of migraine were assessed from these individual reports during the run-in period, during the study and after the last administration of acupuncture.
Ethic aspects
The protocol was reviewed by the Ethics Committee of Saint-Germain-en-Laye, and all patient signed the informed consent form.
Statistical analysis
The primary goal was to analyze the arterial changes after real or sham acupuncture treatments. Data are expressed as mean ± SD or median [interquartile range, (IQR)], as appropriate. Data were analyzed with a repeated measure ANOVA, including comparison between real and sham acupuncture as “between factor”, and period (baseline and month 2) and time (“before needle implantation”, “7th to 10th min” and “17th to 20th min” after insertion) as “within factors”.16 Post-hoc tests were performed with non parametric Wilcoxon paired (time effect) or unpaired (treatment effect) tests. Categorical data were compared with χ2 test. Based on our previous study,5 the inclusion of 14 patients per group yielded a 80% power for an alpha risk at 5% to detect a 7% difference in vasodilatation between real and sham acupuncture. Given an expected dropout rate of 10%, 31 patients were recruited. Twenty-nine completed the study.
Statistical analysis was performed using the NCSS2004 software package (Gerry Hintze, Kaysville, Utah, USA). Statistical significance was assumed for P < 0.05.
Results
Fifteen and 14 patients were randomized to real or sham acupuncture, respectively. Two patients (one in each group) declined the last acupuncture session (Table 1). Patients were slightly (but not significantly) older in the sham group (48 ± 10 vs. 40 ± 11 yrs, respectively, P = 0.09) and 2/3 were female. No difference was observed for blood pressure and heart rate values (Table 1). Typical migraine was present in all patients at baseline. No significant difference was observed for migraine characteristics. Patients scored positive for the three criteria proposed by ISH.9,10 Migraine was severe with a self reported VAS value of 8.7 cm in the sham group and 8.1 cm in the real acupuncture group (P = NS). The average number of days with headache was 7.4/month, corresponding to 5 crises per month. First line chronic treatments (beta-blockers (7/15 versus 6/14), calcium antagonists (2 in each group), and other agents (dihydroergotamine, 6/15 versus 6/14), active acupuncture versus sham acupuncture, respectively) administered before entering the study, and attack medications throughout the study (paracetamol, aspirin, NSAID, ergot alkaloids, triptans) did not differ between groups.
| Real acupuncture verum (n = 15) | Sham acupuncture (n = 14) | ||
|---|---|---|---|
| mean ± SD | mean ± SD | ||
| Baseline | Real versus sham | ||
| Sex (M, F) | 3/12 | 3/11 | NS |
| Age (years) | 40±11 | 48±10 | 0.09 |
| Height (cm) | 169±8 | 170±9 | NS |
| Weight (kg) | 62±14 | 65±11 | NS |
| Use of beta-blockers (Y/N) | 7/6 | 6/8 | NS |
| SBP (mmHg) | 122±20 | 119±18 | NS |
| DBP (mmHg) | 81±14 | 75±13 | NS |
| MBP (mmHg) | 96±14 | 92±14 | NS |
| HR (mmHg) | 72±7 | 70±10 | 0.03 |
| Month 2 | Time effect | ||
| SBP (mmHg) | 124±20 | 118±25 | NS |
| DBP (mmHg) | 82±12 | 80±14 | NS |
| MBP (mmHg) | 97±14 | 93±17 | NS |
| HR (mmHg) | 67±9 | 67±10 | NS |
Baseline characteristics of patients randomized to real or sham acupuncture. Changes in brachial blood pressure and heart rate (HR) after 2 month course of acupuncture are also indicated. Two patients in each group were treated by verapamil.
Acute effects of acupuncture
During the first session, the time-course of changes in radial artery diameter were significantly different between real and sham acupuncture (P < 0.01; repeated measure ANOVA, Fig. 1). Radial artery diameter significantly increased after real acupuncture: radial artery diameter increased by 3.1% IQR [−3.2–8.5] (P = 0.03) during the 17–20 min period (Fig. 1). By contrast, radial artery diameter did not significantly change after sham acupuncture (0.87% IQR [−5.3–5.8].
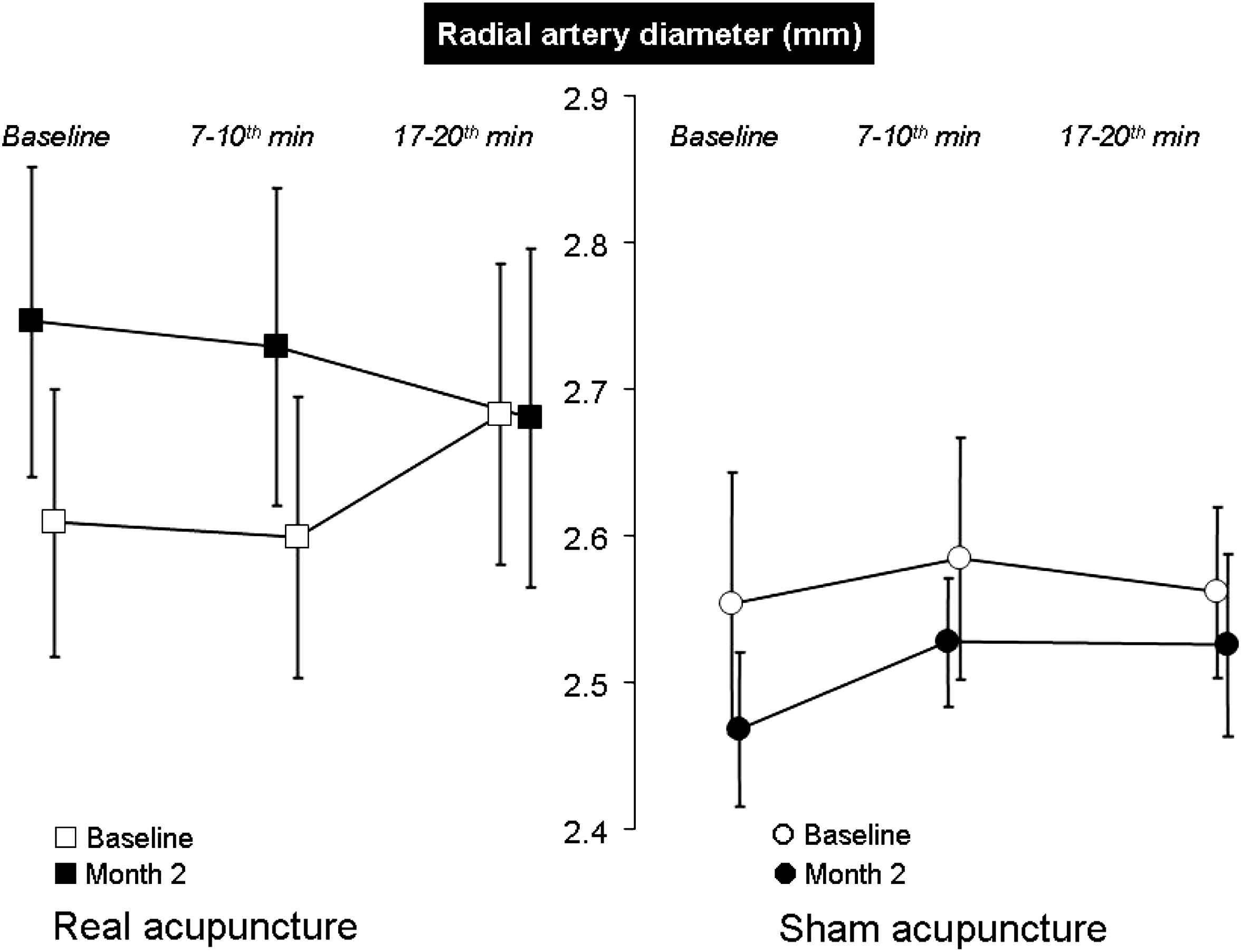
Changes in radial artery diameter after real or sham acupuncture (mean ± SEM). The arrow indicates the time of needle implantation. At baseline, i.e. during the first session, radial artery diameter significantly increased (P = 0.03) after real acupuncture. By contrast, radial artery diameter did not significantly change after sham acupuncture. The time-courses of the changes in radial artery diameter were significantly different between real and sham acupuncture (P < 0.01; repeated measure ANOVA). In the real acupuncture group, radial artery dilatation was maintained after 2 months. Indeed, before needle implantation at month 2, radial artery diameter was significantly higher than before needle implantation at baseline, whereas diameter was smaller in sham treated patients.
At the second visit (month 2), the administration of needles did not significantly change radial artery diameter, whatever the acupuncture groups (real acupuncture −1.5 IQR [−8.8 to 2.2] and sham acupuncture 2.0% IQR [−5.4–7.13]). There was no significant interaction between groups, concerning the time-course of the changes in radial artery diameter during the session (Fig. 1).
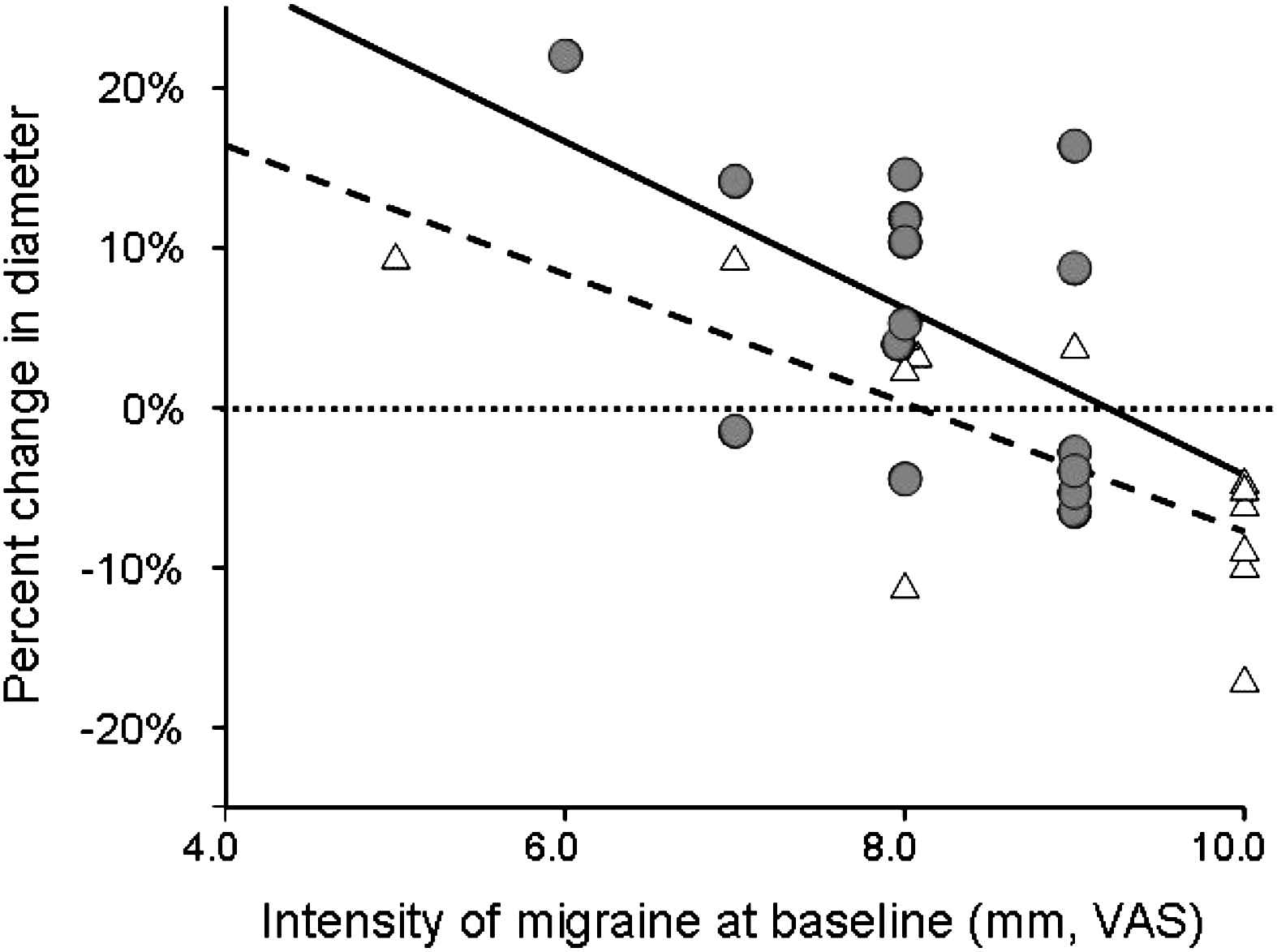
Influence of the baseline intensity of migraine, evaluated from VAS, on the chronic response of the radial artery to real (circles) or sham (triangles) acupuncture. Diameter changes were calculated as [(month 2 session minus baseline)/baseline], thus a negative change in diameter means vasoconstriction. For each session, radial artery diameter was measured before needle implantation. The higher the baseline intensity of migraine, the lower the chronic vasodilatation (and the higher the vasoconstriction) under acupuncture, either sham (dotted line, P < 0.001) or real (continuous line, P = 0.03). The relationship between the baseline intensity of migraine and chronic vasodilatation was shifted upwards (P < 0.01) in patients receiving real acupuncture.
Chronic effect of acupuncture
In the real acupuncture group, radial artery dilatation was maintained after 2 months. Before needle implantation at month 2, radial artery diameter was significantly higher than before needle implantation at baseline. This difference was significantly different from that observed in the sham acupuncture group (5.2% IQR [−3.9–14], −4.4% IQR [−10.0–3.5], respectively; P < 0.01, repeated measure ANOVA) (Fig. 1).
The chronic increase in radial artery diameter, observed before needle implantation at month 2 in the real acupuncture group, was maintained during the whole acupuncture session (“before needle implantation”, “7th–10th min” and “17th–20th min”), and was significantly different from the changes observed in the sham acupuncture group (P < 0.01, repeated measure ANOVA) in which diameter was actually smaller at month 2 than at inclusion. No differences were observed for other radial artery parameters such as distensibility coefficient or elastic modulus. Adjustment on age and utilization of beta-blockers did not significantly alter the effect of acupuncture.
Effect of acupuncture on migraine
There was a tendency (P = 0.064) for a larger improvement of migraine symptoms by real acupuncture, compared to sham acupuncture, when all parameters (intensity, frequency and duration) were combined, although no significant difference was observed when each parameter was analyzed separately. Intensity of pain associated with migraine crises improved significantly (P < 0.01) with time in both groups (8.13 ± 0.91 cm–4.3 ± 2.46 cm in the real acupuncture group, and 8.71 ± 1.48 cm–5.71 ± 2.58 cm in the sham acupuncture group), without any significant difference between groups.
Influence of the intensity of migraine associated pain on radial artery diameter changes
We evaluated the chronic response of the radial artery to real or sham acupuncture according to the baseline intensity of pain, assessed from VAS (Fig. 2). The changes in radial artery diameter were calculated as percent changes [(month 2 session minus baseline)/baseline]. Fig. 2 shows that the higher the baseline intensity of migraine, the lower the chronic vasodilatation under acupuncture, either sham (P < 0.001) or real (P = 0.03). The relationship between the baseline intensity of migraine and chronic vasodilatation was shifted upwards (P < 0.01) in patients receiving real acupuncture. No significant correlation was observed between the chronic radial artery vasodilatation on the one side, and the frequency or duration, of migraine on the other side (data not shown).
Discussion
The main findings of the present study are the followings : (a) in patients with migraine exposed for the first time to real acupuncture, radial artery diameter increased whereas it did not change in the sham group; (b) radial artery diameter remained elevated one month after the last course of real acupuncture whereas a vasoconstriction was observed in sham treated patients; and (c) a higher baseline intensity of migraine associated pain was associated with less chronic vasodilatation under acupuncture, either real or sham.
Interpretation of findings
The present controlled study confirms our previous findings5 that acupuncture can acutely induce a significant vasodilatation of the radial artery. The amplitude of the radial artery vasodilatation observed during real acupuncture in the present study (+2.9%) was smaller than our previous finding in patients regularly exposed to acupuncture (+7.5%),5 but was of the same magnitude as flow-dependent vasodilatation (+3.1%) (15) and +3.6%17 in studies measuring radial artery diameter with the same echotracking system. It was lower than the pharmacological vasodilatation observed with nitrates, either given sublingually (+18%)18 or intra-arterially (+12.5%).17
The present findings extend our previous observation of an acute effect of real acupuncture to the demonstration of a chronic vasodilatation, persisting one month after the last acupuncture session. The magnitude of chronic vasodilatation (+5.5%) tended to reach the magnitude of the acute effects of acupuncture in regular users in our previous study (+7.5%).5
Because radial artery vasodilatation has been observed in patients complaining of various functional symptoms (dorsalgia, headache, dyspepsia, anxiety) and previously exposed to acupuncture, and not in healthy volunteers naïve to acupuncture,5 we raised the hypothesis that either sensitization by repeated acupuncture sessions or a high chronic level of pain were required for acupuncture induced-vasodilatation. Our results suggest that the first explanation is the most likely. Indeed, the magnitude of acute vasodilatation after real acupuncture in the present study was lower than previously observed in sensitized patients.5 In addition, sensitization by 2 courses of real acupuncture one month apart led to a chronic radial artery vasodilatation, reaching a higher lumen enlargement (+5.5%) than after acute acupuncture at baseline (+2.9%) (Fig. 1).
However, by contrast to our original hypothesis relating vasodilatation to pain intensity, Fig. 2 shows that the higher the baseline intensity of migraine, the lower the chronic vasodilatation under real acupuncture. Whether acupuncture-related vasodilatation of the radial artery is caused by active dilatation above the physiological diameter or by the suppression of pain-related vasoconstriction remains to be determined. Vasoconstriction is a major feature of the pathophysiology of migraine, although this is not the triggering event.19 Indeed, the common understanding of migraine is the occurrence of a severe diffuse vasoconstriction in the cerebral and meningeal arteries,20 contemporary of the aura symptoms, followed by a sustained vasodilatation, accepted as the cause of headache. This sequence is discussed for migraine without aura,8 however, most (if not all) treatments of migraine crisis are vasoconstrictors. Peripheral reactivity of large and medium size arteries has been seldom studied in migraine,21,22 and no evidence of susceptibility to vasoconstriction in patients with migraine was shown. The present study was not specifically designed to investigate the pathophysiology of migraine. However, the findings that (a) patients with the most severe cephalagia at baseline were less prone to dilate their arteries during follow-up and (b) a larger radial artery vasodilatation after real acupuncture was observed for any given level of pain intensity, suggest an interaction between the mechanisms of pain and the vasodilatory effects of acupuncture.
The mechanisms by which acupuncture may determine vasodilatation of the radial artery were discussed before.5 Several papers by Langevin et al.23–25 showed that the insertion and manipulation of acupuncture needles may have both local and remote therapeutic effects based on the same underlying mechanism: mechanical coupling of needle to connective tissue. The winding of tissue around the needle could generate a mechanical signal into cells, by pulling of collagen fibers during needle manipulation. These authors23 suggested that downstream effects of this mechanical signal may include cell secretion, modification of extracellular matrix, amplification and propagation of the signal along connective tissue planes, and modulation of afferent sensory input via changes in the connective tissue milieu. Mechanistic studies have demonstrated effects of acupuncture on the activity and plasma concentrations of vasomotor agents, including norepinephrine, angiotensin II, serotonin, enkephalins, beta-endorphins and glutamate.26–28 In our study, acupuncture was able to decrease smooth muscle tone at the site of a muscular artery. Inhibition of sympathetic vasoconstriction by acupuncture has been suggested through various mechanisms including a centrally mediated reflex response and a presynaptic inhibition of sympathetic nerves.29,30 Particularly, endogenous opioids, including beta-endorphin, have been suggested to play a role in the regulation of sympathetic activity in response to acupuncture since naloxone was able to suppress the acupuncture-induced sympatho-inhibition.31,32 Since the peripheral effect of beta-endorphin on endothelial cells is potentialisation of endothelin and inhibition of NO production,33 it is likely that the observed effect of naloxone was centrally mediated. In a previous study,5 we showed that naloxone, a non specific antagonist of μ receptors for opioids induced vasoconstriction, thus demonstrating an endogenous vasodilation by enkephalins. However, we could not demonstrate any interaction with acupuncture. In the present study, vasodilation was related to the level of pain at inclusion. Since vascular hyperreactivity of migrainers is not related to impaired response to nitric oxide,34,35 it could be deduced that part only of the vasodilation observed in response to acupuncture is mediated by the enkephalin pathway. Other mechanisms could be involved. Taken together, the results of the previous5 and present studies suggest that the effects of acupuncture on the radial artery are likely very complex, involving other mediators than opioids.
In the present study, no significant change in blood pressure accompanied the chronic vasodilatation. Although the radial artery is a conducting artery, playing only a minor role in total peripheral resistance, its vasomotor status may reflect the vasomotor tone of smaller resistive arteries. Data from the literature are scarce concerning the effects of acupuncture on blood pressure, and two recent randomized clinical trails yielded conflicting results.36,37 Another interesting finding is that we observed a trend (P = 0.064) for a larger improvement of migraine symptoms by real acupuncture, compared to sham acupuncture. Data from the literature show that acupuncture may be more efficient than placebo on symptoms of migraine.6,38 In the present study, the lack of significant higher efficacy of real compared to sham acupuncture is likely due to a type 2 error, because of the limited number of patients. The existence of a relationship between peripheral vasculature abnormalities and migraine is highly discussed. Previous attempts to demonstrate this point yield conflicting results, two reports finding no alteration in large artery.21,39 or small artery endothelial function,40 whereas two recent report show marked alterations of vascular smooth muscle cells sensitivity to GMPc and NO.41,42 There is no definitive answer whether migraine is a generalized arterial disease with focal expression, however, all drugs used for prevention (or induction) of migraine crisis have major effects on systemic circulation. We did not find any interaction between background drugs (beta-blockers) and response to acupuncture. Whether monitoring of radial artery diameter to assess the efficacy of acupuncture is unlikely but it demonstrates objective quantifiable effects of acupuncture.
Methodological features
The radial artery was studied for three main reasons. First, radial artery pulse characterization is a major base of diagnosis and treatment adjustment in Chinese medicine. Second, it is possible to determine, with a very high precision, small changes in arterial diameter, thanks to high resolution echotracking devices.11,13 Third, we have previously demonstrated that radial artery diameter increased in response to real acupuncture, in patients previously exposed, but not in normal subjects naïve for acupuncture.5 The vasodilation observed during the study was very variable, although this is a common feature of vasodilation studies performed by us,5,18 or by others.17,43 This was taken into account in the calculation of the number of patients, and part of the variability was explained by patients characteristics such as pain intensity at baseline (Fig. 2).
Randomized controlled studies in acupuncture are rare. Double-blinded studies are even scarcer and led to extensive controversies after publication when providing positive results.6,7,36,37,44 In the present paper, we applied good clinical practices of clinical trials and recent recommendations for acupuncture studies.4 Our study was randomized and blinded for both the patients and the physicians who measured the radial artery parameters during the whole study period until database freezing. The skill necessary for practicing acupuncture (either diagnosis and/or treatment) foreclosed the use of a blind investigator for applying acupuncture. Our aim was to measure the effects of needles inserted into specific acupuncture points by comparison with those induced by needles inserted into non-acupuncture “dead” points, in preference to sham needles.45 Indeed, as recommended by the NIH,4 we wanted to test the specificity of site implantation, rather than the act of sticking needles in the skin. Indeed, acupuncture practice is optimized according to the practitioner feelings before and during the session. The practitioner of traditional Chinese medicine (R.C.) was well advised to optimize acupuncture therapy in the real acupuncture treatment group, and to be as neutral as possible in the sham treated group. An equal number of needles was given over an equal length of time thus giving similar levels of care and attention to real and sham groups. Patients could not differentiate between their treatment allocation group (question included in the standardized questionnaire), showing that they were truly blinded according to treatments. We could not exclude a nocebo effect in sham treated patients, neither could we exclude the fact that the practitioner of traditional Chinese medicine (R.C.) was perceived differently by the patient when performing real or sham acupuncture.
In conclusion, an acupuncture-induced vasodilatation was observed in patients suffering from severe migraine and naïve to acupuncture. The vasodilatation was maintained after chronic treatment. In the context of an ongoing controversy about whether acupuncture has more than a placebo effect, the present study gives support to a measurable objective effect of acupuncture therapy in patients with migraine.
Clinical perspective
Acupuncture is an accepted treatment for migraine. Practice of acupuncture is based on palpation of the radial pulses and we have previously shown in a randomized double-blind study that vasodilatation could be observed only in patients suffering from pain and previously exposed to acupuncture, and not in healthy volunteers, naïve to acupuncture. In the present randomized double-blind study, we demonstrated an quantifiable effect of acupuncture on the radial artery diameter of patients suffering from severe migraine, with significant vasodilatory effect both during the first session, and 1 month after the last acupuncture session in patients receiving real acupuncture, not in sham treated patients. We confirmed our hypothesis that either sensitization by repeated acupuncture sessions or a high chronic level of pain were required for acupuncture induced-vasodilatation. We also observed that patients with the most severe pain at baseline were less prone to dilate their arteries during follow-up. Taken together, these results suggest an interaction between the mechanisms of pain and the vasodilatory effects of acupuncture. In the context of an ongoing controversy about whether acupuncture has more than a placebo effect, the present study gives support to a measurable objective effect of acupuncture therapy in patients with migraine.
Disclosure statement
None.
Acknowledgement
This study was performed with grants from
References
Cite this article
TY - JOUR AU - Pierre Boutouyrie AU - Robert Corvisier AU - Kim-Than Ong AU - Claire Vulser AU - Catherine Lassalle AU - Michel Azizi AU - Brigitte Laloux AU - Stéphane Laurent PY - 2010 DA - 2010/02/19 TI - Acute and chronic effects of acupuncture on radial artery: A randomized double blind study in migraine JO - Artery Research SP - 7 EP - 14 VL - 4 IS - 1 SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2009.12.003 DO - 10.1016/j.artres.2009.12.003 ID - Boutouyrie2010 ER -
