Health-Seeking Behavior of People in Indonesia: A Narrative Review
- DOI
- 10.2991/jegh.k.200102.001How to use a DOI?
- Keywords
- Concept of health and illness; health-seeking behavior; Indonesia; pathway of seeking care; social determinants of health; traditional medicines; utilization of health care
- Abstract
This review aims to locate existing studies on health-seeking behavior of people in Indonesia, identify gaps, and highlight important findings. Articles were retrieved from Medline, Scopus, Web of Science, Academic Search Complete (via Ebsco), and ProQuest with a number of key words and various combinations. Articles from Indonesian journals were also searched for with Google Scholar. A total of 56 articles from peer-reviewed journal databases and 19 articles from Indonesian journals were reviewed. Quantitative designs were applied more frequently than qualitative, and mixed methods designs were used in some studies. The majority gathered retrospective information about people’s behaviors. Communicable diseases and maternity care were the most frequently studied conditions, in contrast to noncommunicable diseases. In terms of geographical distribution, most research was conducted on Java island, with very few in outside Java. Important findings are a model of Indonesian care-seeking pathways, an understanding of determinants of people’s care choices, and the role of sociocultural beliefs. The findings from this narrative review provide insight to what and how Indonesians make decisions to manage their illness and why. This makes an important contribution to understanding the problem of underutilization of medical services despite the government’s extensive efforts to improve accessibility.
- Copyright
- © 2020 Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Indonesia is the fourth most populous country in the world with more than 261 million people [1]. The population is spread unevenly, with more than half living on Java, which is only about 6.5% of the total land area [2,3]. Health care in Indonesia is delivered by a mixed system in which government-financed and privately financed health centers coexist. Government health centers consist of community health centers (Puskesmas) at subdistrict level and state hospitals at district and province level [4]. Privately owned health-care services range widely from not-for-profit religious charitable-group-owned health facilities to for-profit non-state health-care facilities including ambulatory clinics and hospital chains [5].
To improve access to medical care, in January 2014 the Indonesian government introduced the Indonesian Universal Health Coverage program, known as the National Social Health Insurance Scheme (Jaminan Kesehatan Nasional, JKN) [6]. The insurance scheme covers most health interventions for people registered under the scheme [6].
Increasing access to health-care services is a key component of improving a nation’s health status. However, at the individual and community level, understanding people’ health-related behaviors is a crucial element in improving community health [7]. Greater understanding of people’s health-related behaviors might shed light on the problems that still exist in the community despite greatly increased access to health services. For example, although the number of deaths from noncommunicable diseases in Indonesia dropped significantly in the last two decades, such diseases including tuberculosis and malaria remain significant health problems [8]. Gaining understanding of people’s health-related behavior is also an important step to establish effective interventions [7,9].
In the Indonesian context, people’s health-related behavior is made more complex due to it being a multicultural, ethnically diverse country with a variety of health providers. As in other low- and middle-income countries, despite wide availability of formal health providers, informal health providers or nonconventional health providers comprise a significant component of health services [10]. In the Indonesian context, these nonformal health providers – known as traditional health providers – are categorized into biologically based therapies (traditional therapies using substances from nature); physical therapies with tools (e.g., acupuncture, acupressure, and cupping therapy); physical therapies without tools (e.g., massage); and mind body therapies (e.g., hypnotherapy and meditation) [11].
With wide availability of these traditional providers, the use of complementary and alternative medicines is also prevalent. This complicates attempts to understand factors driving health-seeking behavior. Health-seeking behavior is defined as “steps taken by an individual who perceives a need for help as he or she attempts to solve a health problem” [12]. It has been the focus of numerous studies in developing countries [13–20]. Other terms with similar meaning include treatment-, care-, and help-seeking behavior [21–23].
This review aims to document existing literature on health-seeking behavior in Indonesia, identify areas and medical conditions that are understudied, and highlight the major findings related to people’s behavior in seeking care.
2. MATERIALS AND METHODS
2.1. Narrative Review
We undertook a narrative review as we aimed to get a deeper understanding of the health-seeking behavior of people in Indonesia. Greenhalgh et al. [24] recommend conducting a narrative review as opposed to a systematic review when the purpose of the review is to get a deeper understanding on the topic. Health-seeking behavior is a broad topic that covers a wide range of health issues. With narrative review, we were able to interpret the patterns of health-seeking behavior among various topics with a wide range of literature available and include literature that may have been excluded with a systematic search. We also aimed to gather as much information as possible from the Indonesian context, so we searched diverse literature sources, including articles in the Indonesian language.
2.2. Data Sources
As health-seeking behavior straddles medical and social sciences, multiple databases were searched in July–August 2017. The databases included: Medline, Scopus, Web of Science, Academic Search Complete (via Ebsco). Anthropological and social sciences databases (via ProQuest) were also used to locate relevant articles. A number of key words and Boolean combinations were applied. The searches used were: “health seeking” OR “help seeking” OR “care seeking” OR “health seeking behavio*r*” OR “treatment seeking behavio*r*” OR “treatment seeking” OR “health behavio*r*” OR “health related behavio*r*” OR “seek medicine*” OR “seek care” OR “delay* treatment” OR “delay* care” OR “self medicat*” OR “self care” OR “self treatment” AND “Indonesia*”. Articles found were assessed for relevance.
We assessed relevance to the topic of health-seeking behavior studies in the Indonesian communities. We found very limited articles when we searched with specific keywords “health-seeking behavior” or “care-seeking behavior”. Therefore, we expanded search to also include a much broader topic “health behavior” as a keyword. With this keyword, we gathered a larger number of papers, but not all were relevant to health-seeking behaviors. We rejected the articles in the scope of health behavior but not relevant to health-seeking behavior.
Further papers identified in reference lists of relevant articles were retrieved. Searches were also carried out of Indonesian journals, using Google Scholar with the same key words translated into Indonesian.
3. RESULTS
3.1. Description of Relevant Literature
Fifty-six peer-reviewed articles were found from 1987 to 2017 [21–23,25–77], and 19 articles from Indonesian journals from 2001 to 2016 [78–96]. Looking at the publication dates, health-seeking behavior in Indonesia drew little attention before 2000, with only six articles before that time.
3.1.1. Methodologies
Quantitative cross-sectional designs (39) were more frequent than qualitative designs (26), with the same pattern for Indonesian journals. Quantitative studies usually used an interviewer-administered questionnaire, possibly to reduce misunderstandings with self-administered questionnaires due to literacy and language issues.
Quantitative studies provide evidence of factors determining people’s behavior, but are limited in their ability to explore the wider narrative of reasons for choosing specific care, which can be explored in qualitative studies. There were also 10 studies that applied mixed methods design [29,43,44,58,61,70,71,92,93,95]. For example, Brooks et al. [29] explored secondary data from the Indonesian Demographic and Health Survey to quantify the effect of the insurance program on maternity services, and explored barriers of the services utilization qualitatively [29].
Most studies were community based. Of those conducted in health-care facilities, Indonesian journals were more likely to carry studies based in traditional medicine clinics. Clinic-based studies exclude people who never seek care [97]. However, recruiting participants with a specific condition from the community means a large number of people need to be screened to find respondents. Some researchers, however, have conducted household surveys to study health-seeking behavior related to acute respiratory illness, tuberculosis, and malaria [21,22,33,62]. Some studies used secondary data from national surveys, revealing patterns of health-care utilization, and sociodemographic determinants [29,52,65,84,89,94,96].
One study asked about a hypothetical scenario [36], but hypothetical behavior can differ from actual behavior. Most other studies gathered retrospective information from people who have a certain illness and asked them to recall what they have done to manage it [98]. This can lead to recall bias. To minimize this, some researchers set up inclusion criteria, for example, newly diagnosed or having symptoms during the last month. In contrast, Utarini et al. [61] used a longitudinal prospective design to explore people’s behavior in seeking care for malaria over 1 year. They detected malaria cases in six endemic malaria villages and what people did during that period. Thus, prospective studies collect more accurate data on health-seeking behavior from the beginning of symptom experiences to the final stage of recovery.
3.1.2. Medical conditions covered
Many studies focused on infectious diseases such as malaria, tuberculosis, and leprosy. Maternity-related health was also common. Tuberculosis, malaria, and mothers’ and infants’ health are important focus areas of the Sustainable Development Goals [99].
Tuberculosis, malaria, and infant health remain significant health problems in Indonesia. Approximately 10% of global tuberculosis patients live in Indonesia with an incidence rate of 399 per 100,000 population in 2016 [100]. Some areas in Indonesia are also endemic to malaria with about 261,617 cases reported in 2018 [101]. In 2015, the maternal mortality and infant mortality rate were recorded as 305 per 100,000 life birth and 22 per 1000 life birth, respectively [4].
Noncommunicable diseases studied included mental illnesses and cancer, but there were fewer studies on stroke, hypertension, and diabetes. The prevalence of noncommunicable diseases in Indonesia is rising and they became major causes of death in 2012 [4,8]. With a prevalence of 47.8%, hypertension has become a leading cause of mortality [102]. The other alarming noncommunicable disease in Indonesia is diabetes. The current diabetes prevalence was 7% with more than a half of them undiagnosed [103,104]. Thus, more studies of health-seeking behavior should focus on chronic diseases.
Other diverse studies included health-seeking behavior of infertility patients and transgender people related to HIV risk [41,47].
3.1.3. Study location
Indonesia is situated between the continents of Asia and Australia, and between the Pacific and Indian Oceans. It is an archipelago of more than 13,000 islands (total land area 1,913,578.68 square kilometers) [2], administratively divided into 34 provinces [2]. It is culturally diverse with more than 1300 ethnic groups and six official religions. Although Islam is the predominant religion, in Bali, Papua, and East Nusa Tenggara, the dominant religions are Hinduism, Protestantism and Catholicism, respectively [105].
Most reviewed studies were on Java, the most populated island of Indonesia, which also includes the capital Jakarta (Figure 1). Java is the most developed region in the country. Within Java, more studies were located in Yogyakarta and Jakarta.
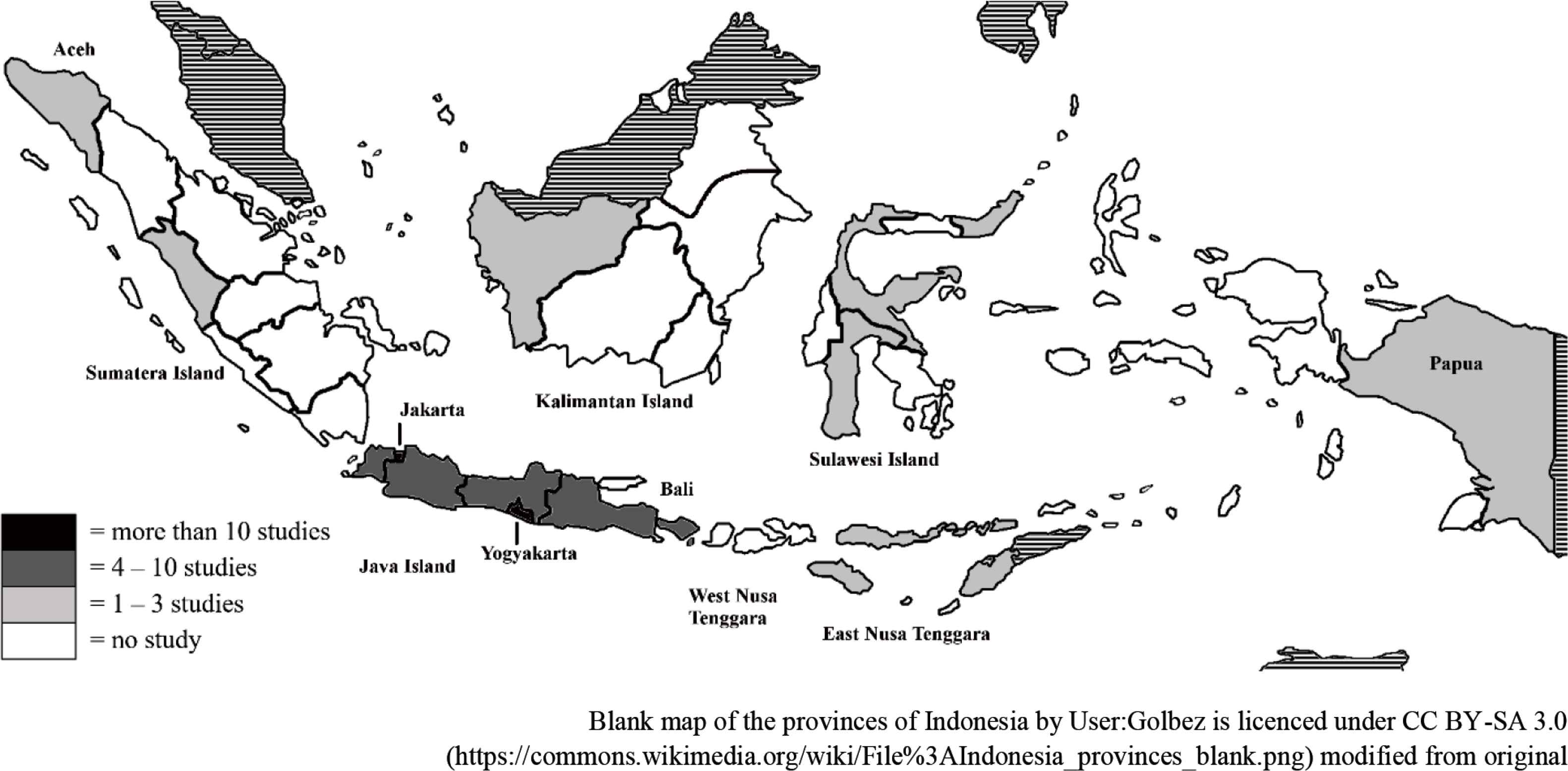
Coverage of geographical areas in the studies reviewed.
Beyond Java, some studies were performed in Aceh and Bali Provinces. Aceh is located on the far north of Sumatera, whereas Bali is an island to the east of Java. Socioculturally, these provinces are different, most people in Aceh are Muslim and in Bali, Hindu.
More studies need to be conducted outside Java, particularly in the East. This area lags behind western Indonesia in terms of economic activities, infrastructure, and population, including health indicators [4].
3.2. Important Findings
3.2.1. Lay concepts of health and illness
Concepts of health and illness are influenced by people’s sociocultural background [106]. Indonesian people consider themselves healthy if they can perform their everyday activities without disruption. Thus, people generally sought help when symptoms hindered these [21,22,25,28,37,39,42,45,51,56,66,67,71,77]. For example, Eeuwijk [71] described that most older people sought care from health professionals for rheumatism because it hindered their activities. In contrast, they did not seek professional help for problems with eyes, ears, or teeth because there was less impact on their daily lives. Thus, people delayed seeking care until their diseases were severe.
There is also a strong concept of “balance and harmony”, particularly among Javanese. Health is a physical status that cannot be achieved without individuals’ spiritual wellbeing. Life in general should be balanced physically and spiritually, between individual and social life, so that a status of “harmony” can be reached [42,57]. The Indonesian government recognizes six official religions: Islam, Catholicism, Protestantism, Hinduism, Buddhism, and Confucianism [105]. Regardless of specific religion, people tend to believe that health is God’s gift and illness is their fate, sometimes viewed as God’s punishment [28,42,46].
3.2.2. Determinants of health provider choices
Indonesian people’s choice of health providers is determined by complex and interrelated factors: sociodemographic characteristics, influence of significant others, sociocultural beliefs, perception about diseases and their causality, and perception of medical services including accessibility and availability, particularly in rural and areas, and its related cost [23,28–30,34,35,38,40–42,45–48,52,54–57,59,60,64,65,67,72].
3.2.2.1. Sociodemographic characteristics
Age, household size, education, and economic status determine people’s choices of health providers [65,74,94]. Poorer households were more likely to use traditional medicines for treating malaria [25], older people and those in rural areas were more likely to seek traditional and alternative treatment [84,89,96]. Women were also more likely to seek health care for tuberculosis-related symptoms [21]. However, other studies did not find a link between seeking care and sociodemographic characteristics [21,53,75,78,81], suggesting other factors may have greater impact in influencing people’s choices in health providers.
3.2.2.2. Influence of significant others
In most Indonesian communities, seeking care involves not only patients but also family, friends, and other community members [21,28,30,31,34,35,38,45,55,59,64,67,72]. Recommendations from significant others were associated with visiting alternative health-care providers for treating tuberculosis [21] and cancer [28,45]. Religious leaders influenced tuberculosis patients’ choices [30]. The husband and older family members made decisions related to birth attendant choices [34].
3.2.2.3. Sociocultural beliefs
Most women chose to give birth at home, helped by a traditional birth attendant, despite the proximity of health facilities or health professionals, mainly because the birth attendant also performed prayers and other traditional practices and ceremony. People believed that birth is sacred and should be consistent with traditional beliefs [29,34,55].
Cultural beliefs also favored traditional remedies or alternative treatments. These practices have been passed down for generations, and this embedded culture cannot be ignored. They are commonly used for treating most diseases, including malaria [25,44,61,69], tuberculosis [21,39,51,59,67,72], leprosy [46], rheumatoid arthritis [76], cancer [28,38,45], hypertension [93], stroke [56], and diabetes [95]. Traditional remedies are also used for promoting health and preventing disease. For example, women took traditional herbal drinks to stay healthy during pregnancy and breastfeeding [26,49], and some people took bitter-tasting plants to prevent malaria [44,62,69,85,90].
People perceived that biomedicine was failing to cure illness; fear of side effects, dependence on medication, and medical procedures were other common reasons cited for using traditional or alternative treatments [28,32,38,92,93,95]. People viewed full cure as successful treatment. Biomedicine was not believed to cure diabetes and hypertension, leading to the choice of traditional treatment [93,95].
Indonesians regard traditional remedies as safe because they are made from natural resources [87,92]. People also perceived that traditional healers provided comprehensive services as they were also dealing with patients’ feelings [45], and in some cases, payment can be made in kind, for example with food [72].
Many forms of traditional remedies and alternative treatments are available in Indonesia. Jamu, a traditional herbal drink is the most popular [107]. Other popular alternative treatments include traditional Chinese medicines, known as sinshe [87], treatment with animal media such as leeches [79], traditional bone setters [82], cupping therapy [86], and coin scratching [83].
3.2.2.4. Perception of causality
Health-seeking behavior was also influenced by perceptions related to diseases and causality. For example, there were strong beliefs that mental illnesses have supernatural causes, so people first sought care from traditional, spiritual, or religious healers [23,35,64]. In some areas, tuberculosis and leprosy were also believed to be caused by black magic or bad spirits and so people sought help from traditional healers [46,67,72].
Communities commonly have their own local term, description, and interpretation of illnesses or symptoms. For example, tuberculosis was believed to be caused by smoking, stress, sleeping on the floor, or other physical causes [59,67,72]. Thus, early symptoms of tuberculosis were not perceived as serious. People in central Java did not recognize malaria, but the local term katisen has similar symptoms to malaria. Again, katisen is seen as a minor illness, leading to self-medication [69]. Javanese often misidentified heart diseases with masuk angin (wind sickness), using the term angin duduk (sitting wind sickness) for heart disease. Masuk angin is a mild illness caused by over exposure to wind, and people treated it with coin scratching, so heart disease is treated in the same way [57].
3.2.2.5. Perception about health-care systems
Perceptions about medical services also influence health-seeking behavior. Many people were reluctant to go to public health facilities as they experienced complex administrative procedures, one-sided communication style of health professionals, and long waiting times [28,29,35,40,41,67]. Thus, many people choose to go to private health providers [22,33,36,51,59,65,67]. Further reasons driving the choice of private providers include perceived quality of provider, availability of brand name medicines, and short waiting times [36,59,66,67].
3.2.2.6. Health cost and people’s perception of health insurance
Expanding health insurance alone was not enough to increase health-care utilization for people residing in rural areas [52]. Indirect costs of treatment, such as transportation, are barriers to medical treatment [28,34,35,45,54]. In many cases requiring hospitalization, family members accompanied the patient during their stay. Extended families were often a source of finance for extra cost [28,34,35,45]. Therefore, the healthcare cost burdened not only the patients, but also their extended families.
People experienced the insurance scheme as complicated and time consuming, poorly socialized and understood [28,29,55,58]. Therefore, people only applied once they perceived the need for help. People also perceived that health providers offered a low quality of service for the poor under the scheme [28,29,55,58]. This might be true, as from the providers’ perspective there has been incomplete reimbursement and low payment [58].
3.2.3. Care pathways
After experiencing symptoms, people generally used self-care: taking rest, self-medicating with medicines bought from drug stores or pharmacies, or taking traditional medicines. If they perceived that the symptoms persisted, they would seek help from formal health care. If that failed, they then would try other traditional or alternative treatments (Figure 2) [28,30,38,43,45,59,62,69,72,73,88,96]. Most then went to either formal or informal health providers, often combining or alternating medicines from different providers [51,67,77,78]. However, if the sick person is a child, going direct to formal health care is common [40,68,73,88,91,96]. A strong belief exists that the effectiveness of treatment is a matter of being “suited to you”, so they would try alternatives to find one that suits [43,69].
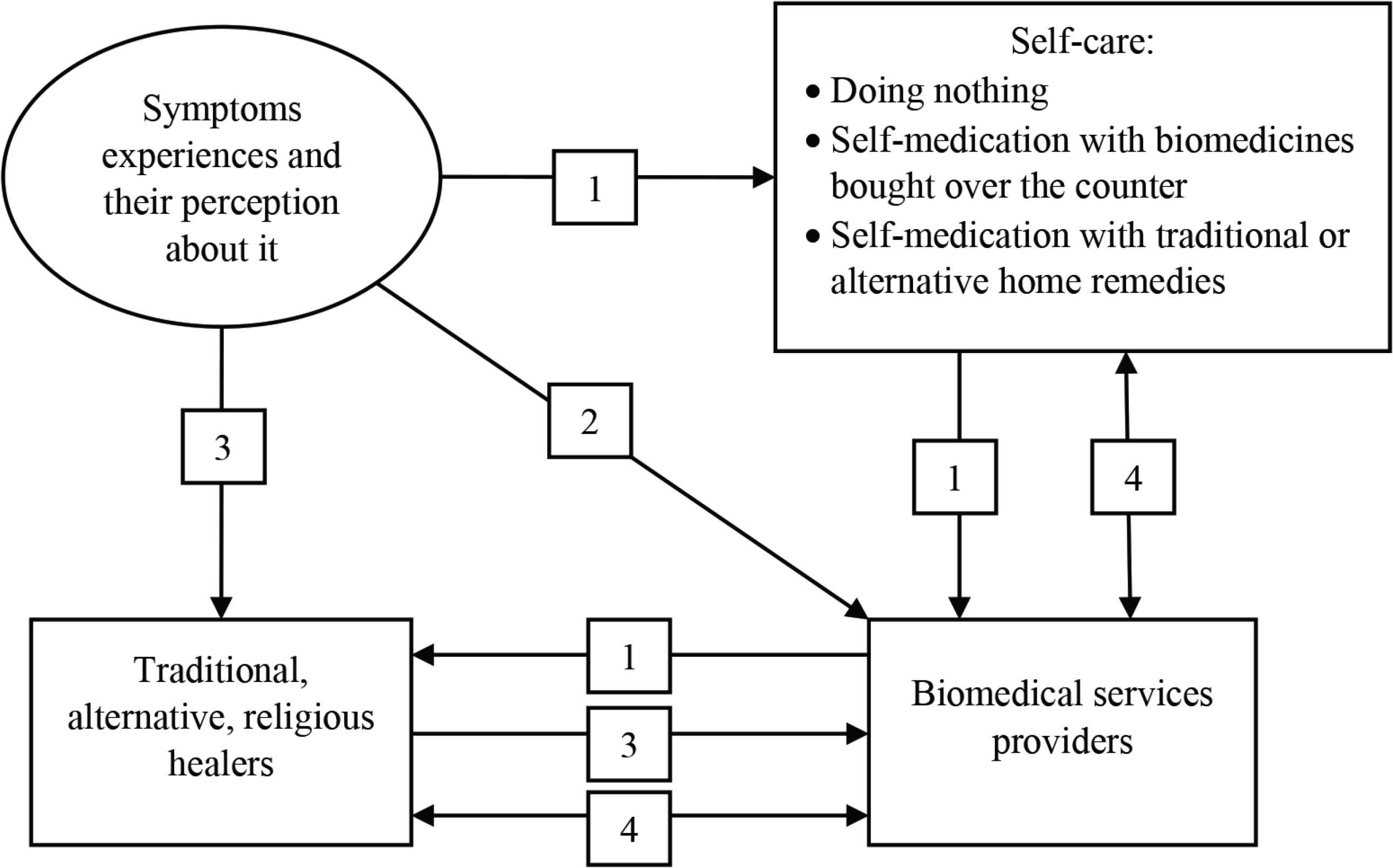
The pathway of seeking care. (1) General process of seeking care. (2) If the sick person is a child. (3) If the disease is strongly attributed to supernatural diseases such as mental illness, or if they perceive that their disease is caused by any supernatural power. (4) Both providers, medical services providers and alternative providers, or type of medications, traditional and biomedicines, are used as an alternate or in combination to find “fit” treatment to them.
Another pathway, as mentioned before, was when people first went to any alternative treatments for illness attributed to supernatural causes, switching to formal health care when they perceived alternative treatments as ineffective [23,35,46,63,64,67,72].
3.2.3.1. Self-medication
Self-medication with biomedicines was a common practice [96]. As with many developing countries, most prescription medicines are available over the counter. People self-medicated with antibiotics for treating a common cold, headache, and other minor symptoms [27,40,50]. People also self-medicated for malaria and tuberculosis [30,39,51,59,61,62,67,69,73,80], and musculoskeletal pain [76]. Many self-medication practices are inappropriate [73].
4. DISCUSSION
This is the first review to look into health-seeking behavior in Indonesia. This review shows that there are significant gaps in the literature about health-seeking behaviors in the Indonesian context. Many studies on health-related behavior focused on a restricted range of health problems. Research on health behavior on child immunization has not been updated for a long time, and very limited studies explored the behavior of people with chronic illnesses such as hypertension and diabetes. Research on the health-seeking behavior of people in Indonesia needs to be conducted in these understudied areas. Understanding people’s behavior related to immunization is particularly important as Indonesia has lower immunization coverage compared with most other countries in the Southeast Asia region [99]. Research suggested that understanding people’s perspectives and behavior related to child immunization is the key to success for immunization programs [108].
Health-seeking behavior studies also need to cover chronic diseases. The prevalence of chronic diseases such as hypertension and diabetes in Indonesia has increased during the past decade [102,103]. Studies in other countries found that people’s behavior in managing chronic illness, for example diabetes, were very complex and influenced by cultural beliefs and values [109–112]. Understanding people’s cultural beliefs and values were key elements for a successful diabetes intervention program [113]. We found that, in terms of geographical areas, most of the studies were conducted within Java island. Some studies outside Java were focused only in particular areas including Aceh and Bali Province. Limited studies were observed from the eastern part of Indonesia. With the wide cultural diversity in Indonesia, research on health-seeking behavior needs to also be expanded to cover understudied areas.
This review also suggests that people’s behavior in seeking care was determined by a range of internal and external factors. The internal factors include individual characteristics and perceptions and beliefs about the disease and its treatments. The external factors may include influence of significant others and perceptions about the health-care and health insurance systems. These findings are similar to studies in other low- and middle-income country contexts [13–16,19,20] and align most with the Kroeger’s model of determinant of choices of health-care services [97]. The Kroeger model incorporates three major factors influencing people’s choices within the wide range of health providers: characteristics of person, characteristics of disorders and their perceptions, and characteristics of the health services system [97].
Health interventions should be developed based on this knowledge on factors determining behavior. This review found that traditional treatments were chosen when people perceived supernatural causes of the disease and when they perceived the biomedical system have failed to cure their chronic diseases, similar to research in Zambia and Kenya [15,20]. The choice of care was also influenced by people’s perception related to the disease and its causality. Therefore, interventions should be made to address misconceptions related to diseases and perceived causality, which hinder people from seeking care. One study attempted to do this through implementing tuberculosis leadership groups within the community, who held meetings to discuss peoples’ perceptions about tuberculosis and to address any misunderstanding found, leading to greater engagement with formal health care [39]. This effort should be expanded to other communities and diseases.
On the other hand, traditional medicine systems are important in developing countries. People value their efficacy, and they are widely accepted. Thus, integrating these into formal health care may be more effective than discouraging them. For example, mothers’ preference for a traditional birth attendant has resulted in collaboration between village midwives and birth attendants in some areas of Indonesia [34]. The Indonesian government has also initiated efforts to ensure the safety and effectiveness of traditional herbal medicines [107]. However, in many cases, the safety and efficacy of techniques used in traditional medication systems are questionable and not scientifically proven. Therefore, their existence should not replace formal health care.
The characteristics of the medical care provider, including availability and cost, also influenced people’s behaviors in seeking care [17,18]. This review shows that the cost mentioned as a barrier to seeking care included transport and other costs related to hospitalizations. The insurance program or the government also need to consider this nonmedical cost as a financial burden to the patients.
Negative past experiences with the public health-care system has made people reluctant to engage. Therefore, improving availability and accessibility may have to be balanced with improving quality of care. Another health system issue is the availability of prescription medicines over the counter, driving increased self-medication.
The other important finding in this review is the pathway of seeking care. Before people in Indonesia seek biomedical help, most of them would self-medicate, including with antibiotics. The government should develop serious efforts to prevent the misuse of antibiotics as the problem of antibiotic resistance in Indonesia and worldwide is alarming. A study in a hospital in Indonesia showed that most bacteria were resistant to the third generation of cephalosporins and quinolone [114]. Worldwide, more than 70% of bacteria were also resistant to most antibiotics available in the market [115].
In summary, studies on health-seeking behavior is important to understand factors determining people’s behavior. This understanding would allow more evidence-based health-care intervention and policy.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
AWW contributed in acquisition and analysis the data and prepared the initial draft of the manuscript. JAG, SH and PN critically reviewed and revised the initial draft.
REFERENCES
Cite this article
TY - JOUR AU - Anna Wahyuni Widayanti AU - James A. Green AU - Susan Heydon AU - Pauline Norris PY - 2020 DA - 2020/01/30 TI - Health-Seeking Behavior of People in Indonesia: A Narrative Review JO - Journal of Epidemiology and Global Health SP - 6 EP - 15 VL - 10 IS - 1 SN - 2210-6014 UR - https://doi.org/10.2991/jegh.k.200102.001 DO - 10.2991/jegh.k.200102.001 ID - Widayanti2020 ER -
