Syphilis Testing among Men Who Have Had Rectal Gonorrhea and Chlamydia Tests, United States
- DOI
- 10.2991/jegh.k.190620.001How to use a DOI?
- Keywords
- Rectal specimens; gonorrhea; chlamydia; syphilis; reactivity; confirmatory testing
- Abstract
The Centers for Disease Control and Prevention (CDC) recommends syphilis screening at least annually for sexually active men who have sex with men (MSM). The objective of this study is to assess the frequency of MSM testing for syphilis and how syphilis test results compared with results of rectal gonorrhea and chlamydia tests. In collaboration with a large US commercial laboratory, we identified men aged 15–60 years who had rectal chlamydia or gonorrhea tests during 09/01/2013–09/30/2015 as presumed MSM. We classified MSM as having current or past syphilis if during the study period they had (1) either a reactive qualitative non-treponemal test or at least a 1:1 quantitative non-treponemal test, and (2) they had a reactive treponemal test. Of 52,771 MSM, 14.3% had no syphilis testing, 4.8% had only treponemal testing (37.8% were reactive), 63.2% had only non-treponemal testing (2.0% were reactive), and 17.7% had both non-treponemal and treponemal testing (86.6% had current or past syphilis). Of those MSM who had reactive qualitative non-treponemal tests, at least 90% had no quantitative non-treponemal tests. Current or past syphilis was more common among MSM with positive rectal gonorrhea or chlamydia tests (24.1%) than MSM with negative rectal gonorrhea and chlamydia tests (13.0%, p < 0.005). Of MSM with any syphilis testing during 09/01/2013–09/30/2014, 64.8% also had annual repeat testing. Syphilis testing in general and repeat syphilis testing were frequent but suboptimal among MSM. It is important to continually monitor syphilis for MSM, especially for those MSM who had rectal chlamydia or gonorrhea infection.
- Copyright
- © 2019 Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Men who have sex with men (MSM) are at high risk for HIV and other sexually transmitted diseases (STD), such as gonorrhea, chlamydia, and syphilis [1,2]. The Centers for Disease Control and Prevention (CDC) recommends routine HIV and STD screening of all sexually active MSM [2]. Specifically, sexually active MSM should be tested at least annually: for HIV; for syphilis; for urethral gonorrhea and chlamydia if they report insertive intercourse; for rectal gonorrhea and chlamydia if they report receptive anal intercourse; and for pharyngeal gonorrhea if they report receptive oral intercourse. More frequent STD screening, such as at 3–6 month intervals, is recommended for higher risk MSM, such as those who have multiple or anonymous partners. CDC also recommends that patients should be tested for other STDs if they have gonorrhea, chlamydia, or syphilis.
Previous studies have shown that chlamydia, gonorrhea, syphilis, and HIV testing is suboptimal among MSM and rectal gonorrhea, rectal chlamydia, and syphilis were associated with increased risk for HIV seroconversion among MSM [3–11]. However, none of those studies has focused on the association between rectal gonorrhea or chlamydia and syphilis among MSM. The objective of this study is to assess the frequency of testing for syphilis among MSM and how syphilis test results compared with results of rectal gonorrhea and chlamydia tests.
2. METHODS
Gonorrhea, chlamydia, and syphilis testing data were obtained from a US commercial laboratory that provides laboratory testing in all 50 states and the District of Columbia. These data included all gonorrhea detection tests, chlamydia detection tests, syphilis non-treponemal tests (qualitative and quantitative), and syphilis treponemal tests performed in men and women from 09/01/2013 through 09/30/2015. The gonorrhea and chlamydia detection tests include nucleic acid amplification test or culture during this study period. Of specimens collected for gonorrhea and chlamydia testing during this study period, more than 50% had no anatomic site information. The database included information on the patient’s year of birth, gender, US geographic region of residence, test type, anatomic site for a proportion of gonorrhea or chlamydia specimens, test result, and provider specialty. We used a combination of patient characteristics to create a de-identified analytic data set that permitted us to monitor testing over time for an individual patient. The study protocol was reviewed and approved by the Institutional Review Board at the CDC (CDC protocol ID: 5935).
We limited our analysis to men aged 15–60 years who had rectal gonorrhea or chlamydia tests during the study period of 09/01/2013–09/30/2015. Men who had rectal gonorrhea or chlamydia tests were presumed to be MSM for this analysis. Among these MSM, we identified those who had any positive rectal gonorrhea or chlamydia tests and calculated the prevalence of rectal gonorrhea or chlamydia infections during the study period. We calculated the frequency and reactivity of valid qualitative or quantitative non-treponemal tests and valid treponemal tests during the study period. The qualitative non-treponemal and treponemal tests were considered valid if results were listed as reactive, positive, negative, or nonreactive. In general, weakly reactive results are not obtained from Rapid Plasma Reagin (RPR) tests, only from the Venereal Disease Research Laboratory. More than 99% of the non-treponemal tests were RPR in this database during the study period. The quantitative non-treponemal tests were considered valid if the results were listed as a ratio (e.g. 1:1, 1:2, 1:4, 1:8, or higher).
The laboratory system offered both the traditional syphilis serology testing algorithm and the reverse syphilis serology testing algorithm, although the database did not specify which algorithm was used for each syphilis test [12]. Based on their valid syphilis tests during the study period, MSM were classified into four syphilis test groups: (1) no syphilis test, (2) only non-treponemal tests, (3) only treponemal tests, and (4) both non-treponemal and treponemal tests. We classified MSM as having (1) current or past syphilis if they had both reactive treponemal and non-treponemal tests (either reactive qualitative or valid quantitative); and (2) current syphilis if they had quantitative non-treponemal tests that were ≥1:8 and reactive treponemal tests, according to the publication of the Association of Public Health Laboratories [12]. We assessed the association between positive rectal gonorrhea or chlamydia tests and current or past syphilis status.
We assessed annual repeat testing for MSM who only had syphilis testing during 09/01/2013–09/30/2014 to allow at least 12 months of follow-up time. The earliest date of any syphilis testing during 09/01/2013–09/30/2014 was defined as the index date. Annual repeat syphilis testing was defined as any syphilis testing performed during 3–14 months after the index date. The average number of days between the index date and the earliest date of repeat testing was also assessed. Annual repeat syphilis testing rates were compared for MSM with and without positive rectal gonorrhea or chlamydia tests.
All analyses were performed using SAS version 9.3 (SAS Institute, NC, USA). We used χ2 tests to assess syphilis testing rates, reactivity of non-treponemal and treponemal tests, and the association of positive rectal gonorrhea or chlamydia tests with current or past syphilis. A two-sided p-value <0.05 was considered statistically significant.
3. RESULTS
Between 09/01/2013 and 09/30/2015, 1,341,778 men aged 15–60 years had any gonorrhea or chlamydia tests in the laboratory data set; of those men, 52,771 (3.9%) had rectal gonorrhea or chlamydia tests. Of those 52,771 presumed MSM, 59.0% were aged 25–44 years, 42.9% were from the South, and 20.9% had positive rectal gonorrhea or chlamydia results Table 1.
| Characteristics | Number of MSM | Syphilis testing received during the study period | Number of current or past syphilis | |||
|---|---|---|---|---|---|---|
| N (%) | Both tests (%) | Non-treponemal test only (%) | Treponemal test only (%) | No test (%) | N (%) | |
| Total | 52,771 (100) | (17.7) | (63.2) | (4.8) | (14.3) | 8090 (15.3) |
| Age (years) | ||||||
| 15–24 | 8369 (15.9) | 12.6 | 62.2 | 5.0 | 20.2 | 841 (10.1)* |
| 25–34 | 19,303 (36.6) | 17.4 | 63.2 | 6.0 | 13.4 | 2871 (14.9) |
| 35–44 | 11,828 (22.4) | 19.8 | 62.5 | 4.7 | 12.9 | 2076 (17.6) |
| 45–54 | 10,557 (20.0) | 20.4 | 63.8 | 3.0 | 12.8 | 1922 (18.2) |
| 55+ | 2714 (5.1) | 15.8 | 66.9 | 2.8 | 14.5 | 380 (14.0) |
| Region | ||||||
| Midwest | 4130 (7.8) | 5.7 | 13.5 | 40.3 | 40.5 | 200 (4.8)* |
| Northeast | 7381 (14.0) | 14.3 | 64.8 | 0.4 | 20.5 | 846 (11.5) |
| South | 24,353 (46.2) | 20.4 | 69.1 | 2.3 | 8.2 | 4215 (17.3) |
| West | 16,907 (32.0) | 18.2 | 66.1 | 1.7 | 14.0 | 2829 (16.7) |
| Positive status of rectal gonorrhea or chlamydia tests | ||||||
| Yes | 11,036 (20.9) | 27.2 | 53.7 | 6.1 | 13.0 | 2660 (24.1)* |
| No | 41,735 (79.1) | 15.1 | 65.7 | 4.5 | 14.7 | 5430 (13.0) |
p < 0.005 between syphilis testing and characteristic variable.
Syphilis testing received and the number of current or past syphilis among 52,771 MSM aged 15–60 years during the study period, 09/01/2013–09/30/2015
Of those 52,771 MSM, 14.3% had no syphilis test during the study period. MSM who resided in the Midwest were significantly more likely to have no syphilis testing than those who resided in other regions (40.5% vs. 20.5% in the Northeast, 8.2% in the South, and 14.0% in the West, all p < 0.05). Among MSM who had no syphilis testing, 19.0% had a positive rectal gonorrhea or chlamydia test.
Overall, at least 15.3% of the 52,771 MSM had current or past syphilis. Current or past syphilis was more common among MSM with positive rectal gonorrhea or chlamydia tests (24.1%) than among MSM with negative rectal gonorrhea and chlamydia tests (13.0%, p < 0.05).
Among 9340 MSM who had both non-treponemal and treponemal tests, 8090 (86.6%) had current or past syphilis Figure 1. Of these 8090 MSM, 2660 (32.9%) had a positive rectal gonorrhea or chlamydia test. Of the 8090 with current or past syphilis, 313 had an RPR titer ≥1:8 suggesting current syphilis. Of these 313 MSM, 120 (38.3%) had a positive rectal gonorrhea or chlamydia test.
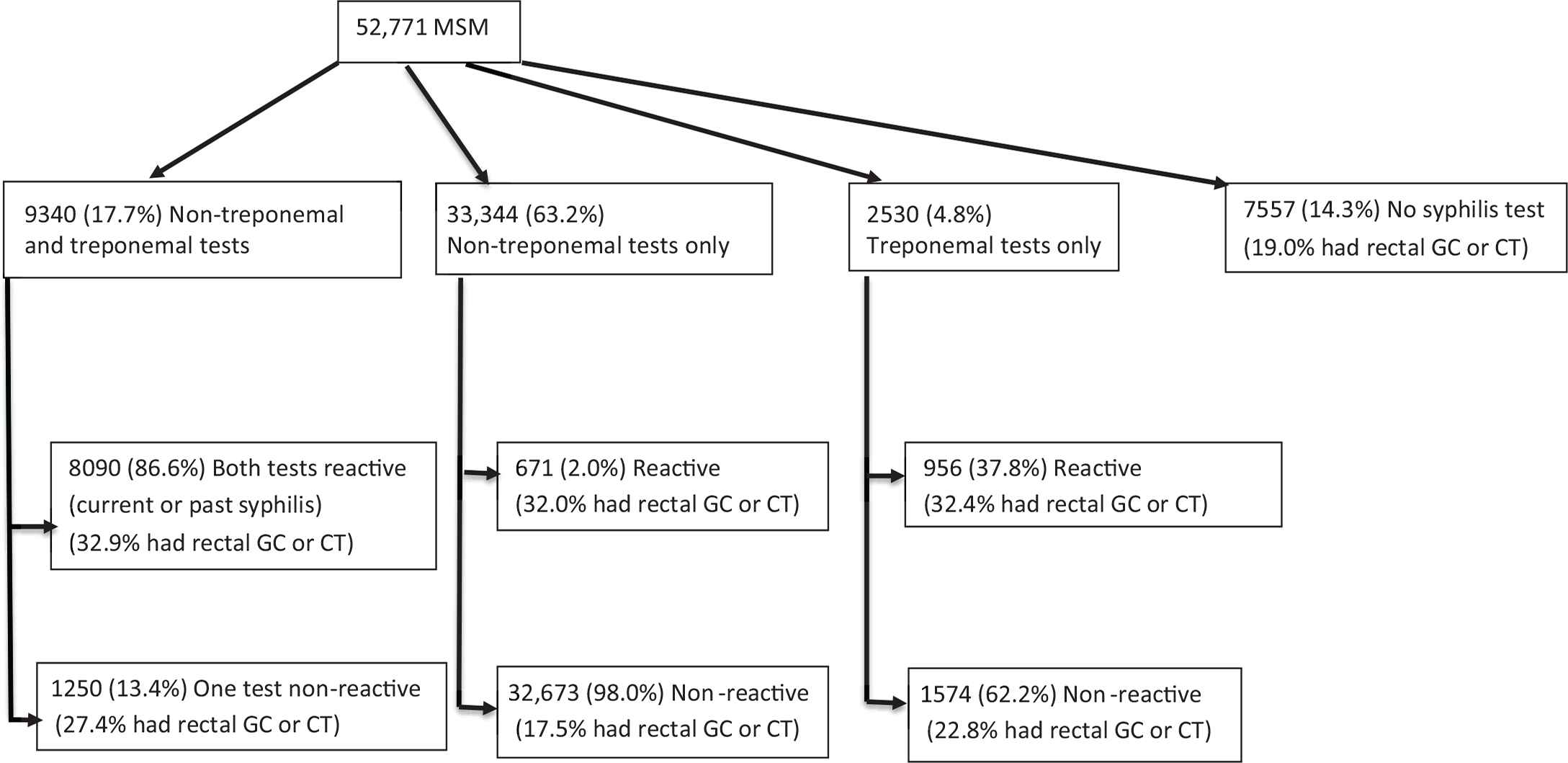
Syphilis testing status and rectal gonorrhea or chlamydial infection among 52,771 MSM aged 15–60 years during the study period, 09/01/2013–09/30/2015.
Among 33,344 MSM who had only non-treponemal tests, 671 (2.0%) had reactive qualitative non-treponemal tests. Of these 671 MSM, 59 (8.8%) had a quantitative non-treponemal test which would be helpful in identifying re-infection if these patients had past syphilis. For the others, the interpretation of the single reactive result is unclear. Of these 671 MSM, 215 (32.0%) had positive rectal gonorrhea or chlamydia tests.
Among 2530 MSM who had only treponemal tests, 956 (37.8%) had reactive treponemal tests. The interpretation of these 956 results is unclear without an accompanying non-treponemal test and we had no information on testing that may have been performed at other laboratories. Of these 956 MSM, 310 (32.4%) had a positive rectal gonorrhea or chlamydia test.
Among 27,434 MSM who had the index date for syphilis test during 09/01/2013–09/30/2014, 64.8% had an annual repeat syphilis test and the average days between the date of annual repeat syphilis testing and the index date were about 179 days (standard error = 95 days) Table 2. MSM with positive rectal gonorrhea or chlamydia tests were more likely to have annual repeat syphilis testing than MSM with negative rectal gonorrhea and chlamydia tests (75.4% vs. 61.8%, p < 0.05). MSM were also more likely to have annual repeat syphilis testing if they were aged ≥25 years, resided in non-South regions, or served by infectious disease or public health providers at the index date.
| Characteristics | Number of MSM | Annual repeat syphilis testing rate (%) | Average days between initial syphilis test date and the earliest repeat syphilis test date |
|---|---|---|---|
| N (%) | Days (standard deviation) | ||
| Total | 27,434 | 64.8 | 179 (95) |
| Age in years | |||
| 15–24 | 3107 (11.3) | 52.9* | 177 (92) |
| 25–34 | 9691 (35.3) | 61.6 | 179 (93) |
| 35–44 | 6679 (24.4) | 67.5 | 180 (96) |
| 45–54 | 6351 (23.2) | 71.6 | 181 (95) |
| 55+ | 1606 (5.8) | 70.1 | 178 (94) |
| Region | |||
| Midwest | 1801 (6.6) | 63.5* | 175 (88) |
| Northeast | 3596 (13.1) | 67.5 | 182 (96) |
| South | 12,615 (46.0) | 55.1 | 193 (101) |
| West | 9422 (34.3) | 77.2 | 166 (87) |
| Provider type at the index date | |||
| Infectious disease | 20,347 (74.2) | 66.0* | 171 (90) |
| Internal medicine | 2848 (10.4) | 65.6 | 217 (109) |
| Family practice | 2083 (7.6) | 59.9 | 199 (100) |
| Public health | 521 (1.9) | 69.1 | 187 (91) |
| Multiple group practice | 1113 (4.0) | 49.7 | 202 (105) |
| Other | 522 (1.9) | 63.4 | 191 (93) |
| Positive status of rectal gonorrhea or chlamydia tests | |||
| Yes | 6192 (22.6) | 75.4* | 164 (85) |
| No | 21,242 (77.4) | 61.8 | 185 (97) |
p < 0.005 between annual repeat syphilis testing and characteristic variable.
Annual repeat syphilis testing rate among 27,434 MSM aged 15–60 years who had initial syphilis during 09/01/2013–09/30/2014
4. DISCUSSION
Our data show (1) a high prevalence of current or past syphilis infection (15.3%) and high rectal gonorrhea or chlamydia infections (20.9%) among MSM in this database, and (2) MSM with positive rectal gonorrhea or chlamydia tests were more likely to have current or past syphilis than those with negative rectal gonorrhea and chlamydia tests. Although it is important for clinicians to screen all sexually active MSM for syphilis, MSM with a positive rectal chlamydia or gonorrhea test result are at elevated risk. Our data show current syphilis cases were highly associated with positive rectal gonorrhea or chlamydia tests: 1.1% of MSM with positive rectal gonorrhea or chlamydia tests and 0.5% of MSM with negative rectal gonorrhea and chlamydia tests were identified as having current syphilis.
Compared with previous studies on syphilis testing (ranged from 49% to 71%) [7,8], our study showed that about 85.7% of men who had rectal gonorrhea or chlamydia tests in this data set during 2013–2015 had syphilis testing. But, our study also showed that syphilis testing rates were very low for MSM who resided in the Midwest region where about 40.5% of them had no syphilis testing or for young MSM aged 15–24 years that about 20% of them had no syphilis testing. Although young MSM aged 15–24 years had lower current or past syphilis than MSM aged 25–60 years, some of them may experience with the current syphilis. Further evaluation is needed to identify the reasons for the low syphilis testing rate in general and especially in the Midwest region. The rectal testing data show that MSM in the Midwest had similar positivity to MSM in the other regions; therefore increasing syphilis testing in this region is an important preventive strategy that could improve syphilis detection and treatment substantially.
Most of the MSM tested had negative non-treponemal tests only, indicating most syphilis testing was performed using the traditional algorithm. Most of the MSM who had both non-treponemal and treponemal tests appeared to have old syphilis because they were reactive on both, and few of them had high non-treponemal test titers that would suggest new infections. MSM with a history of syphilis are at risk for other infections and should be routinely tested for gonorrhea, chlamydia, and syphilis.
The annual repeat syphilis testing rate of 64.8% in MSM, plus suboptimal follow-up of rectal gonorrhea or chlamydia detailed in a previous study [13], suggests healthcare providers should prioritize adherence with CDC recommendations and test MSM routinely for gonorrhea, chlamydia, and syphilis. Of MSM who had syphilis testing during 09/01/2013–09/30/2014, MSM were more likely to have annual repeat syphilis testing if they were served by infectious disease (66%) or public health providers (69%) than multiple group practice providers (50%) at the index date. To continually monitor quality of healthcare service for MSM, annual repeat syphilis testing is needed especially for MSM who were served by infectious disease providers because they often provided healthcare for MSM or by multiple group practice providers because they were unlikely to provide annual repeat syphilis testing.
There were several limitations in this study. First, because this laboratory system does not include self-reported sexual identity and sexual behavior and not all specimens collected for gonorrhea and chlamydia had anatomic site information, the MSM that we identified might be underestimated and might not represent all MSM in the database. The MSM defined in this study as those with rectal chlamydia or gonorrhea testing may be biased to at-risk MSM. There may have been MSM in the data who did not receive rectal testing or who did not involve in rectal sex. Second, the data collection did not include the syphilis testing algorithm used; therefore we could not determine the number of tests performed under each syphilis testing algorithm and the number of initial syphilis tests. Also, the data lack details on the reasons for testing, such as referred syphilis tests or confirmatory syphilis tests. Third, our estimated numbers of current or past syphilis may have been underestimated because (1) 14.3% of MSM had no syphilis test, (2) ≥90% of MSM with reactive qualitative non-treponemal tests did not receive quantitative non-treponemal testing, and (3) 6.5% of MSM with reactive qualitative non-treponemal tests did not receive treponemal tests. It is not clear what proportion of MSM with reactive qualitative non-trponemal syphilis had a history of reactive treponemal tests before the study period. Also, it is not clear what proportion of MSM were without quantitative non-treponemal tests because no quantitative non-treponemal test was performed in the reverse syphilis testing algorithm or because quantitative non-treponemal tests were performed but the valid results were not recorded in the data system. Finally, the data system does not include patients’ race and ethnicity or HIV infection status, although it is known that these factors are also highly associated with syphilis infection [1].
Our findings suggest that syphilis testing was suboptimal among MSM who had rectal chlamydia or gonorrhea testing. The lack of quantitative non-treponemal testing and limited repeat testing also suggest that syphilis screening of MSM could be improved. Positive tests for rectal gonorrhea or chlamydia were highly associated with current or past syphilis. Our study suggests that it is important to continually monitor syphilis for MSM, especially for those MSM who had rectal chlamydia or gonorrhea infection.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHOR CONTRIBUTIONS
G.T., T.P., T.G. and M.N. study conceptualization and writing (review & editing) the manuscript; G.T. and M.N. data curation; G.T. formal analysis and writing (original draft); G.T. and T.P. investigation and methodology; M.N. and T.G. project administration.
DISCLAIMER
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
REFERENCES
Cite this article
TY - JOUR AU - Guoyu Tao AU - Thomas A. Peterman AU - Thomas L. Gift AU - Melinda B. Nye PY - 2019 DA - 2019/07/02 TI - Syphilis Testing among Men Who Have Had Rectal Gonorrhea and Chlamydia Tests, United States JO - Journal of Epidemiology and Global Health SP - 153 EP - 157 VL - 9 IS - 3 SN - 2210-6014 UR - https://doi.org/10.2991/jegh.k.190620.001 DO - 10.2991/jegh.k.190620.001 ID - Tao2019 ER -
