Prevalence and risk factors of human papillomavirus infection types 16/18/45 in a cohort of French females aged 15–23 years
- DOI
- 10.1016/j.jegh.2013.11.003How to use a DOI?
- Keywords
- HPV infection; Genotyping; Young females; Screening; Epidemiology
- Abstract
Investigation of the prevalence and risk factors of human papillomavirus (HPV) infection is the basis for developing prophylactic strategies against cervical cancer, especially for young women. This study aimed to assess the prevalence and risk factors of HPV infection among a cohort of sexually active young French women eligible for catch-up vaccination. Between 1997 and 2007, 2163 women aged 15–23 years attending consultations at the department of gynecology in the Hospital of Besançon (France) were screened for high risk HPV (HR HPV) infection. Risk factors were investigated through a questionnaire sent to all participants in 2010. HPV DNA was detected by HC2 and Probe Set assays. The overall prevalence for HR HPV and HPV16, 18 and/or HPV45 was 44.6% (95% CI, 42.5–46.7%) and 19% (95% CI, 17.3–20.7%), respectively. The response rate to the questionnaire was 22.6%. The prevalence of independent risk factors (age older than 19, smoking, and oral contraception) for HPV 16/18/45 infection in this population was less than 20%. Based on this study, HPV vaccination should be offered not only to teenage girls, but also to young women, regardless of their sexual activity.
- Copyright
- © 2014 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
1. Introduction
Human papillomavirus (HPV) infection is the most common sexually transmitted infection around the world [1,2]. A large majority of women are usually infected soon after they become sexually active in their teens or early twenties [3,4]. Most infections are cleared within two to 3 years [5], but women with persistent infection are at high risk of developing high-grade cervical intraepithelial neoplasia and invasive cancer years later [6]. The main risk factor for cervical cancers is high-risk HPV (HR HPV). Of these viruses, HPV types 16 and 18 are responsible for up to 70% of cervical cancers worldwide [1]. Different co-factors play a role in the persistence of HPV and the risk of development and progression of cervical lesions [7]. They are related to the host (hormones, genetic, immune response) [8], the virus (genotype, multiple infection, viral load and integration) [7] and the environment (high parity and long-term oral contraceptive use [9,10], tobacco smoking and co-infection with other sexually transmitted diseases [11]). However, the key risk factor is sexual behavior especially age at first intercourse and number of life-time partners which reflects exposure to HPV [12,13]. Since 2006, two vaccines have been approved and designed to protect against cervical intraepithelial neoplasia (CIN) grades 2 and 3 and cancers related to HPV 16 and HPV 18 infection in women with no evidence of previous exposure to vaccine-specific HPV types [14]. Until 2013, the French health authorities recommended vaccinating 14-year-old girls before their first sexual intercourse, and proposed a catch-up vaccination for 15- to 23-year-old women only if they have not yet had any sexual activity, or during the first year following their first sexual intercourse [15,16]. In France, there are consistent data documenting HPV prevalence in cervical lesions in women aged over 18 [17], but data from the specific population targeted by the vaccines are scarce [18]. Monitoring HR HPV infections in young women prior to vaccination is necessary to detect early changes in HPV prevalence in vaccine era and to adjust the cervical cancer screening policies.
To give an accurate description of HPV circulation in women who met the criteria of French recommendations for vaccination until December 2012, the prevalence of HPV types 16, 18 and/or 45 was estimated in a cohort of unvaccinated women enrolled between 1997 and 2007. The potential risk factors related to HR HPV, and HPV 16, 18 and/or 45 infection, were also reported.
2. Methods
2.1. Patients and study design
2,163 sexually active women aged 15–23 years living in the geographic region of Franche-Comté, France, who attended a consultation in the gynecology department of the University Hospital of Besançon, France, between January 1, 1997 and December 31, 2007 were included in the study. The Local Medical Ethics Committee (Besançon, France) and the National Committee for the protection of privacy and personal data (Commission Nationale de l’Informatique et des Libertés, CNIL) approved the study. Informed consent was obtained from all participants.
2.2. Specimen collection, cytology and HPV testing
At the time of the gynecology consultation, all women had a pelvic examination and two cervical smears were obtained. The first specimen was collected with a Cytobrush® Plus (Medscand Medical, Malmö, Sweden) for conventional cytology and sent to the pathology laboratory. Pap smear results were reported using the Bethesda system. The second cervical sample was collected with the DNAPAP Cervical Sampler™ (Qiagen, Gaithersburg, MD, USA) for HPV testing. The brush was transferred into a vial containing 1 mL Specimen Transport Medium® (STM) (Qiagen) and the specimen was then processed for routine HR HPV DNA testing with the Hybrid Capture 2 assay (HC2) (Qiagen) according to the manufacturer’s instructions. This test permits the detection of the HPV DNA of 13 HR-HPV types, namely HPV 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68. Samples were then stored at −20 °C.
All cervical specimens positive for HR HPV and from which enough material was available were retested in 2008 using the HPV 16/18/45 Probe Set Test (Qiagen). This test is also based on liquid hybridization with specific probes that make it possible to confirm the presence of HPV16 and/or HPV18 and/or HPV45 DNA in the samples without identifying the specific type. The HPV 16/18/45 Probe Set Test has an analytical sensitivity (1 pg/mL) similar to that of the HC2 test.
2.3. Questionnaire investigating risk factors for HPV infection
In June 2010, a questionnaire was sent with an explanatory letter to all females enrolled in the study between 1997 and 2007, to the postal address indicated in their medical file. Questions were regarding socio-demographic characteristics (educational level, smoking) at the time of HPV testing performed between 1997 and 2007, gynecological history (age at first HPV test, age at first menstruation, age at first pregnancy, number of children at HPV test, previous sexually transmitted diseases), and sexual behavior (age at first intercourse, duration between age at first intercourse and age at HPV test, contraceptive use). Due to privacy legislation, the CNIL authorized to ask the question regarding the number of sexual partners at the time of the questionnaire, but not at the time of the HPV test. A reminder was sent by post four weeks later if the questionnaire was not returned.
2.4. Statistical analysis
The number of females enrolled in the cohort (n = 2,163) allowed the study team to estimate the overall prevalence of HR HPV and HPV 16/18/45 with a precision of 5% and 10%, respectively.
Continuous data are presented as mean (range) and categorical (qualitative) variables as number and percentage. A Mac Nemar test was performed to test the association between HPV and cytology results.
Prevalence was defined as number of women positive for HPV infection at the time of the first gynecology consultation between 1997 and 2007/total number of women screened by HPV test. Further analysis was performed to verify the representativeness of the sample of women who responded to the questionnaire in 2010 in comparison with the overall cohort of women included between 1997 and 2007.
To assess the association between HPV infection and the characteristics of women at the time of the HPV test, a crude odds ratio (OR) with exact 95% confidence interval (CI) was calculated. The number of subjects to be included in the risk factors analysis was based on the detection of a minimum OR of predictors using logistic regression. For an OR = 1.5, with an alpha risk of 5% and a power of 80%, 450 subjects are sufficient.
Continuous variables such as age at HPV test and the period of inclusion were categorized and tested by the Wald χ2 test. When potential risk factors were found to be associated with infection with a p value <0.10 by univariate analysis, they were subsequently entered into the multivariate logistic regression model (stepwise selection) to identify factors independently associated with HR HPV infection or 16/18/45 HPV infection. Goodness of fit for the final model was assessed using the Hosmer–Lemeshow test. The multivariate models tested were adjusted for the period. All tests were two-sided and a p-value <0.05 was considered statistically significant. All analyses were performed using SAS version 9.2. (SAS Institute, Cary, NC, USA).
3. Results
From 1997 to 2007, 2163 females aged 15–23 years who attended a consultation in the gynecology department were enrolled in the study. The average age of the cohort was 21.1 years (median: 21.4, standard error 2.0). The questionnaire investigating retrospectively the potential risk factors was returned by 511 women, of whom 491 had completed the questionnaire, and 20 refused to respond (Fig. 1).
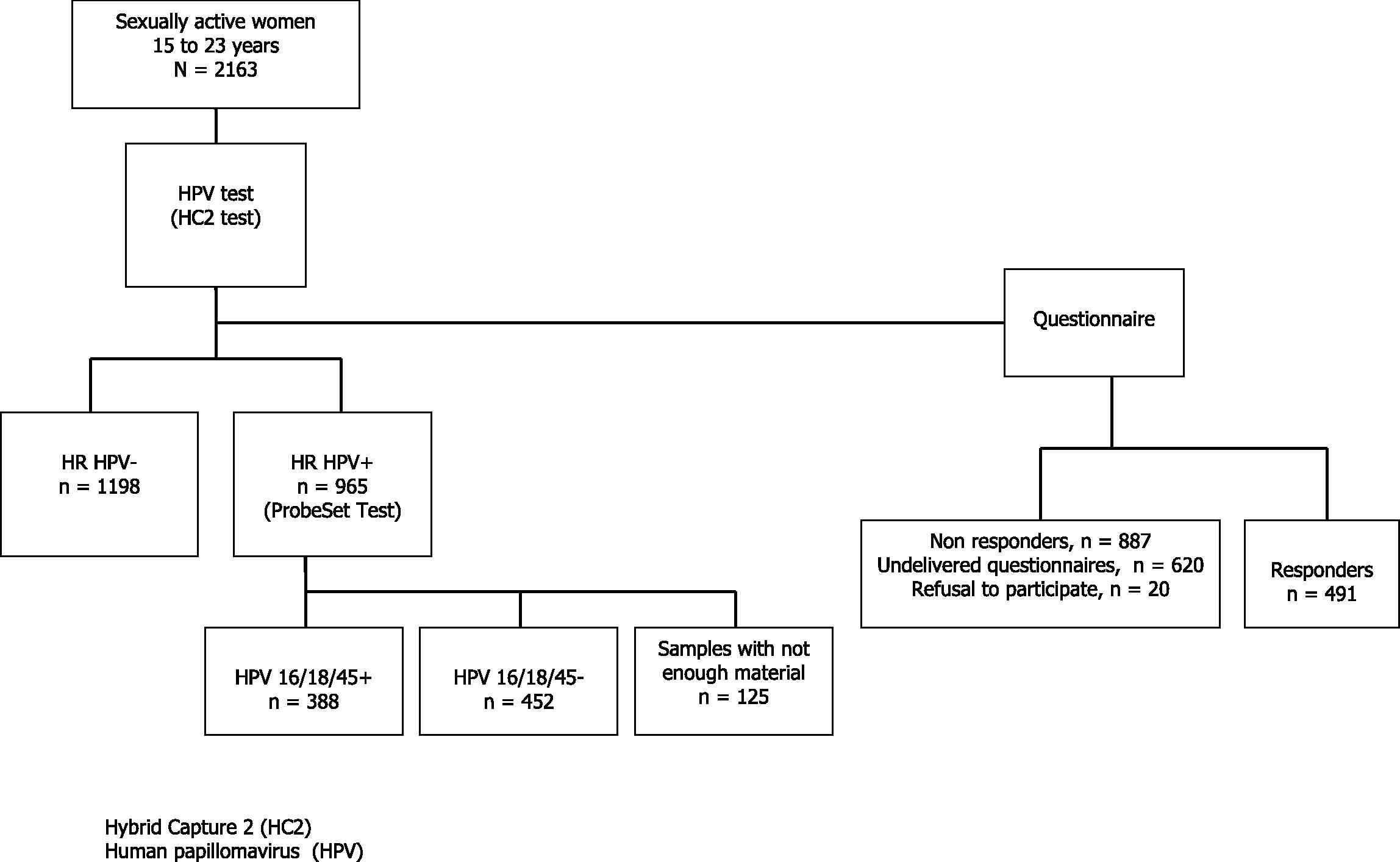
Flow chart presenting the design of the study. 145 questionnaires could not have been sent because addresses were not available.
3.1. Prevalence of high risk HPV and HPV types 16/18/45 according to age
Out of the 2163 specimens collected, 44.6% (95% CI: 42.5–46.7%) were positive for HR HPV. The results from ProbeSet test showed that out of the 2038 analyzable specimens, 19% (95% CI: 17.3–20.7%) were positive for HPV 16/18/45 (Table 1).
| Age | Proportion in population (%) | HR HPV positive | HPV 16/18/45 positive | ||
|---|---|---|---|---|---|
| Sample size | Prevalence (%) (95% CI) | Sample size | Prevalence (%) (95% CI) | ||
| [15–18] | 34.81 | 182 | 35.71 (28.8–42.7) | 175 | 16.57 (11.1–22.1) |
| [18–19] | 12.19 | 178 | 39.33 (32.2–46.5) | 170 | 17.06 (11.4–22.7) |
| [19–20] | 11.76 | 249 | 43.37 (37.2–49.5) | 238 | 15.55 (11.0–20.2) |
| [20–21] | 10.81 | 330 | 43.94 (38.6–49.3) | 307 | 19.54 (15.1–24.0) |
| [21–22] | 10.19 | 350 | 46.29 (41.1–51.5) | 335 | 22.09 (17.7–26.5) |
| [22–23] | 10.10 | 436 | 49.08 (44.4–53.8) | 405 | 19.75 (15.9–23.6) |
| [23–24] | 10.10 | 438 | 45.89 (41.2–50.6) | 408 | 19.36 (15.5–23.2) |
| Total | 100.00 | 2163 | 44.61 (42.5–46.7) | 2038a | 19.04 (17.3–20.7) |
The data are based on results for 2038 women whose specimens could have been tested.
Prevalence of HR HPV and HPV 16, 18 and/or 45.
The overall prevalence by age is reported in Table 1 and Fig. 2. There was an overall significant increase in HR HPV prevalence with age until 22 years (29.4–49.1%, p = 0.0013, β = 2.29). Women over 20 years of age were at a significantly higher risk of being infected by HR HPV (p = 0.006) in comparison with women under 20 (46.4% and 39.7%, respectively). However, prevalence of HPV 16/18/45 showed an almost similar age-distribution around 18%.

Prevalence of high risk HPV and HPV 16, 18, and/or 45 by age. Abbreviations: HR, high risk; HPV, human papillomavirus. Note: One age class was created for women aged 15 and 16 years because of low number in each group.
Of the 2,163 cervical swabs, cytology was available for 63% (1377/2163) of the samples at the time of the study. Among those samples 68.8% (948/1377) were within normal limits (WNL), whereas 8.4% (116/1377) showed atypical squamous cells of undetermined significance (ASCUS), 19.0% (262/1377) low-grade squamous intraepithelial lesion (LSIL) and 3.7% (51/1377) high-grade squamous intraepithelial lesion (HSIL). Over the 1377 samples, 558 (40.5%) were HR HPV-positive. This proportion increased significantly according to cytological diagnosis severity from 24% in normal specimens to 59% in ASCUS, 81% in LSIL and 92% in HSIL (p < 0.0001). Among 948 women with normal cytology the overall HR HPV prevalence varied according to age from 19% below 19 years to 25.2% above 19 years (p < 0.0001).
As for HPV 16/18/45, they were detected in 9.9% of WNL samples, 25.2% of ASCUS, 33.6% of LSIL and 59.1% of HSIL.
3.2. Risk factors associated with HR HPV and HPV 16/18/45 infection
The response rate to the questionnaire was 22.6% and the mean age of responders was 27.3 years in 2010.
Table 2 shows the number of young women enrolled every year (starting from 1997) and the number of women who completed the questionnaire. The percentages of responders per inclusion year were similar at the exception for year 1998. Thus the responder sample is representative of the entire cohort. Moreover, there was no statistical difference between women who responded to the questionnaire and those who did not respond in terms of age at HPV test, HR HPV-positivity (41.1% vs. 44.6%) and HPV 16, 18, and/or 45 (17.5% vs. 17.9%).
| Year of inclusion | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | |
| Number of women at the time of HPV test | 27 | 75 | 114 | 113 | 94 | 231 | 300 | 392 | 307 | 225 | 285 |
| Number of responders at survey | 6 | 9 | 29 | 26 | 18 | 53 | 67 | 89 | 70 | 55 | 69 |
| Response rate (%) | 22.2 | 12.0 | 25.4 | 23.0 | 19.1 | 22.9 | 22.3 | 22.7 | 22.8 | 24.4 | 24.2 |
Response rate to the questionnaire sent to women according to the year of inclusion.
The socio-behavioral characteristics of the women who answered the questionnaire are summarized in Table 3. The median ages at first menstruation and first sexual intercourse were 12.8 and 16.5, respectively. No association was found between the infection status (HR HPV and HPV 16, 18 and/or 45) and the age at first menstruation or at first intercourse. The average age at first pregnancy was 20 years for responders who had had a baby before the HPV test (n = 50).
| Characteristics | Overall Sample | HR HPV+ | HPV 16/18/45+ | |||
|---|---|---|---|---|---|---|
| Numbers of responses | Mean (range) or n (%) | Numbers | Mean (range) or n (%) | Numbers | Mean (range) or n (%) | |
| Age at first menstruation (years) | 488 | 12.8 (9–19) | 199 | 12.8 (9–19) | 84 | 12.7 (9–17) |
| Age at first sexual intercourse (years) | 488 | 16.5 (12–22) | 200 | 16.5 (12–22) | 84 | 16.3 (13–22) |
| Age at first pregnancy (years) | 50a | 20.2 (16–23) | 202 | 21.7 (16–23) | 82 | 19 (16–22) |
| Age at the time of HPV test (years) | 491 | 21.1 (15.1–23.9) | 202 | 20.7 (13–23) | 86 | 21.3 (15.4–23.9) |
| Time between first intercourse and HPV test (years) | 488 | 4.5 (0–9.63) | 200 | 4.8 (0.5–9.6) | 85 | 5.0 (0.5–9.6) |
| Smoking at the time of HPV test | 465 | 249 (53.5%) | 199 | 122 (61.3%) | 83 | 53 (63.8%) |
| Use of oral contraception at the time of HPV test | 465 | 259 (55.6%) | 202 | 126 (62.3%) | 86 | 56 (65.1%) |
HR, high risk; HPV, human papillomavirus.
16 missing.
Socio-behavioral characteristics among women who responded to the questionnaire in 2010 (n = 491).
In the bivariate analysis, among women who reported taking oral contraceptives at the time of the HPV test (55.6%), the risk of infection with HR HPV and HPV 16/18/45 increased significantly (OR = 1.78, 95% CI, 1.08–2.94 and OR = 1.57, 95% CI, 1.08–2.27, respectively) compared with women using other methods of contraception. Moreover, 249 responders (53.5%) were smokers at the time of the HPV test, and smoking increased the risk of HR HPV infection (OR = 1.83, 95% CI, 1.27–2.65) and HPV 16/18/45 infection (OR = 1.78, 95% CI, 1.09–2.91). The average age at which women consulted the gynecologist and tested for HPV was 21 years, with a median of 4.5 years between the first intercourse and the first consultation in gynecology. Women who consulted less than 4 years before their first sexual intercourse had a lower risk of being infected by HR HPV (OR = 0.65, 95% CI, 0.45–0.94) and HPV 16, 18 and/or 45 (OR = 0.58, 95% CI, 0.35–0.96).
The multivariate model identified two factors that were independently associated with HR HPV and HPV 16, 18 and/or 45 infections: smoking and use of oral contraceptives (Table 4). Two factors were independently associated with HR HPV infection such as the age >19 years (OR = 2.87, 95% CI, 1.40–5.83) and having a baby at the time of the HPV test that showed a protective effect (OR = 0.48, 95% CI, 0.24–0.95).
| Characteristics | HR HPV positive | HPV 16, 18 and/or 45 positive | ||||
|---|---|---|---|---|---|---|
| N (%) | OR (95% CI) | p-Value | N (%) | OR (95% CI) | p-Value | |
| Age at the time of HPV test (years) | 0.0005 | 0.06 | ||||
| [15–19] | 16 (20.8) | 1 [Reference] | 9 (12.9) | 1 [Reference] | ||
| [19–21] | 61 (42.1) | 2.87 (1.40–5.83) | 24 (22.2) | 1.54 (0.62–3.84) | ||
| [21–23] | 79 (47.0) | 3.83 (1.91–8.84) | 39 (30.4) | 2.82(1.19–6.63) | ||
| [23–24] | 46 (45.5) | 4.19 (1.98–8.84) | 14 (20.3) | 1.98 (0.75–5.20) | ||
| Smoking habit at the time of HPV test | 0.002 | 0.013 | ||||
| No | 77 (35.6) | 1 [Reference] | 33 (17.8) | 1 [Reference] | ||
| Yes | 122 (48.9) | 2.03 (1.36–3.05) | 53 (27.9) | 2.02 (1.17–3.49) | ||
| Contraception at the time of HPV test | 0.012 | 0.016 | ||||
| Pill | 126 (45.8) | 1.62 (1.09–2.43) | 56 (27.5) | 1.90 (1.10–3.28) | ||
| Other method | 74 (34.2) | 1 [Reference] | 30 (17.5) | 1 [Reference] | ||
| Having one baby at the time of HPV test | 0.032 | 0.60 | ||||
| No | 179 (42.1) | 1 [Reference] | 73 (22.8) | 1 [Reference] | ||
| Yes | 15 (30.0) | 0.48 (0.24–0.95) | 9 (20.4) | 0.83 (0.35–1.96) | ||
| Age at first menstruation (years) | 0.23 | 0.23 | ||||
| <12 | 41 (47.1) | 1.37 (0.86–2.19) | 19 (29.2) | 1.54 (0.85–2.82) | ||
| ⩾12 | 158 (39.4) | 1 [Reference] | 65 (21.1) | 1 [Reference] | ||
CI: confidence interval.
Stepwise model.
Adjusted on age at first sexual intercourse (years) and duration between age at first sexual intercourse and age at HPV test (years).
Goodness of fit based on Hosmer–Lemeshow p = 0.36 for exposure to HR HPV and p = 0.54 for exposure to HPV 16, 18 and/or 45.
Multivariate analysis of factors associated with HR HPV and HPV16, 18 and/or 45 infections among 491 sexually active females aged 15 to <24 years.
Due to privacy legislation, only the number of sexual partners at the time of the questionnaire was available. Interestingly, women who had ⩾4 sexual lifetime partners at the survey time presented the highest rate of positivity for HR HPV when included in the study for HPV testing (p < 0.0001).
4. Discussion
This is the largest French epidemiological study that focused on sexually active women aged 15 to 23 years taking into account socio-behavioral characteristics and risk factors of HPV infection. In this cohort, the overall prevalence of HR HPV was 44.6%, with 19% (95% CI, 17.3–20.7%) infected with current vaccine types 16 and/or 18. In Danish women the prevalence of HR HPV as well as HPV 16/18/45 reached similar rates to those reported here [19]. A Swedish study reported an even higher prevalence of HR HPV infection of 61.6% in a group of sexually active women aged 15–23 with a tendency to increase from 16 to 21 years of age [20]. The high prevalence of HPV in this cohort also agrees with two recent studies that included unvaccinated young women participating in the Chlamydia trachomatis screening program in England [12] and in the Netherlands [21]. Italian studies reported rates ranging from 10% to 15% for HPV 16 and 18 among sexually active women of 18–24 years of age [22,23]. In contrast Dunne et al. showed a lower HR HPV prevalence ranging from 18% to 28% among American sexually active females aged 14–24 years [24]. Monsonego et al. found a HR HPV prevalence of 23.5% in women aged <25 years attending private gynecology practices in Paris, France [18,25], a prevalence very similar to that observed in German women attending a gynecologist in private practice [26]. Manhart et al., who included both sexually active women and women having signed a virginity pledge, found a rate of only 7.8% [27]. Whether national and regional differences in age and type specific patterns of HPV prevalence may be partly attributed to the protocol used for specimen collection and HPV assay, the overall high prevalence of HR HPV as well as HPV 16/18/45 found in this series of young females could also be explained by the hospital-based recruitment of a high-risk population as shown by a high percentage of abnormal cytology (31.2%) which is in agreement with a previous observation in another series of young women [28]. The rate of HPV 16/18/45 in HSIL (59.1%) is similar to that reported by Coupé et al. [29]. Surprisingly, in the present report, the prevalence of the HPV was stable while it peaks at 22–24 years in a population of Dutch women with a significant decrease with age thereafter [29].
Teenagers who consult in STD planning or a hospital have likely a higher frequency of risk factors and a higher HPV 16 prevalence compared with primary care patients [30]. The Danish study pointed out that women aged 15–22 years could also have a greater interest in health, or a higher rate of risky behavior [19]. Nevertheless, this cohort did not differ from the general French population in terms of age at first menstruation (12.8 vs. 12.6) or age at first sexual intercourse (16.5 vs. 17), but the age at first pregnancy appeared to be lower (20.2 vs. 29.4) [31], which could be explained by socio-demographic reasons such as income or level of education. However, due to ethical reasons, it was not allowed to collect these two personal data that could not have been analyzed in the multivariate model.
These results also identified well-known risk factors such as smoking habits and oral contraception for both HR HPV and HPV 16/18/45 infection. The International Agency for Research on Cancer HPV Prevalence Surveys noted an increasing risk of HPV infection with smoking intensity, after allowing for the lifetime number of sexual partners [32]. Similarly, in a cohort of 8508 women from Costa Rica, a positive association was found between smoking and HPV infection, but only for HPV 16 [33]. The association between smoking and HPV infection has also been confirmed in other studies among females aged 13–21 and 18–20 years [34,35], whereas others did not report any association [36,37]. The higher risk of being infected by HPV among women taking an oral contraceptive could be indicative of high-risk sexual behaviors. However, it is difficult to separate the effects of the contraceptive pill use from those of sexual activity, and several investigations have found no association [38,39]. Recently, a meta-analysis confirmed that first coitus at a young age (⩽15), increased number of pregnancies, increased number of sexual partners, use of contraceptives, smoking and chewing tobacco habits, and early age at marriage were significant risk factors for HPV infection [40]. These results stress that females aged 19–23 who were current smokers and taking an oral contraceptive might need closer HR HPV follow-up than the general population. Even risk factors for exposure to HPV infection were investigated retrospectively in this study, sometimes up to 13 years later for women enrolled in 1997, the information collected from the questionnaire, such as age at first menstruation, first intercourse or first child are major events in a woman’s life and should not be subject to memory bias, whereas data concerning smoking and oral contraception use could be affected by memory bias.
Several international studies have confirmed that a high number of lifetime sexual partners increased the risk of infection with one or more HPV types over time [12,13,18,25,26,41]. Unfortunately, due to ethical reasons, data on the number of sexual partners at the time of the HPV test were unobtainable, and this variable could not be studied.
Until 2013, French recommendations limited vaccination to young women who had never had any sexual activity or who were within 1 year of their first sexual encounter. It is best to get the HPV vaccine before becoming sexually active and coming in contact with HPV. However, the vaccine is recommended in many countries for women who are already sexually active because they are unlikely to be infected by both HPV 16/18. Interestingly, this study showed that HPV 16/18 and/or 45 were present in 19% of the sexually active young women. Thus, if HPV 45 is not taken into consideration, it could be estimated that the implementation of the vaccination against HPV 16 and 18 could prevent HPV 16/18 infection in more than 80% of this cohort. In the general population, the prevalence of the vaccine HPV types is likely much lower than among the hospital-based cohort, suggesting that the young population studied would benefit much more from prophylactic vaccination, regardless of their sexual activity status. Indeed, the efficacy of the quadrivalent vaccine for women who were seropositive for HPV and DNA-negative at the time of enrollment was at least 66.9% [42].
Several modeling studies have shown that vaccination programs including 12-year-old girls and catch-up vaccination for adolescents and young adult women with no time restrictions after the first sexual intercourse result in faster decreases in HPV-related disorders [43–45]. These results were observed at the level of the population in Australia, where, after the start of the HPV vaccination program, there was an acceleration in the public health impact of vaccination and an increase of the short-term benefits [46].
This study provides the first estimate of prevalent HPV 16/18/45 infection among a large French cohort of young females aged 15–23 years. Furthermore, the same risk factors were identified for HR HPV and HPV 16, 18 and/or 45 infections, such as smoking and the use of oral contraceptives. Overall, the HR HPV prevalence was high (44.6%), with the highest prevalence noted among females aged 20–23 years, underlining the importance of following up women who are HR HPV-positive and who have not been vaccinated. However, the prevalence of HPV vaccine types was relatively low suggesting that it could be possible to expand the target group for catch-up vaccination by including women who are already sexually active for more than one year. Given the lower than expected coverage rate of HPV vaccine in France, vaccination advisory boards have provided recently new recommendations.
Conflict of interest
DR is an occasional speaker for Sanofi-Pasteur MSD.
Acknowledgments
We thank all the staff of the gynecology department. We particularly thank Fiona Ecarnot for editorial assistance. The ProbeSet tests were kindly provided by Qiagen (Gaithersburg, MD, USA). The study was funded by the Ligue Contre le Cancer (comité du Doubs, CCIR-GE).
References
Cite this article
TY - JOUR AU - Ariane Baudu AU - Jean-Luc Prétet AU - Didier Riethmuller AU - Morgane Chotard AU - Christiane Mougin AU - Mariette Mercier PY - 2014 DA - 2014/01/23 TI - Prevalence and risk factors of human papillomavirus infection types 16/18/45 in a cohort of French females aged 15–23 years JO - Journal of Epidemiology and Global Health SP - 35 EP - 43 VL - 4 IS - 1 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2013.11.003 DO - 10.1016/j.jegh.2013.11.003 ID - Baudu2014 ER -
