Mass Gathering Medicine (Hajj Pilgrimage in Saudi Arabia): The Outcome of Cardiopulmonary Resuscitation during Hajj
- DOI
- 10.2991/jegh.k.190218.001How to use a DOI?
- Keywords
- Cardiac arrest; cardiopulmonary resuscitation; Hajj; mass gathering; Utstein-style
- Abstract
The annual Hajj (pilgrimage) to the Islamic holy shrines at the city of Makkah in the Kingdom of Saudi Arabia is one of the largest yearly recurring mass gatherings worldwide. We aim to evaluate the outcome of outside and inside the hospital cardiopulmonary resuscitation to resuscitate cardiopulmonary arrest among pilgrims. In a prospective cohort study of cardiac arrest patients during Hajj period (January 2004–December 2007 and January 2010–December 2011), 426 patients were resuscitated. The mean age was 64.0 ± 12.0 years. A total of 252 (52.2%) patients had an outside the hospital cardiac arrest, whereas 174 (40.8%) patients had an inside the hospital cardiac arrest. The survival rate of outside the hospital was 5%, whereas inside the hospital was 30%. The overall survival rate was 15.5%. During Hajj, cardiopulmonary resuscitation inside the hospital was associated with better clinical outcomes than outside the hospital. Patients with cardiac arrest outside of the hospital are much less likely to survive due to the lack of immediately trained help and the delay of arrival of aid due to overcrowding. Sudden cardiac arrest leading to death could be minimized if cardiopulmonary resuscitation and defibrillation are delivered before the arrival of emergency medical services.
- Copyright
- © 2019 Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
A mass gathering is defined as a large number of people who are attending a certain event that is focused on specific places for a finite time. Consequently, Mass Gathering Medicine has emerged as a new medical field that focuses on the health risks and hazards of mass gatherings [1]. The annual Hajj (pilgrimage) to the Islamic holy shrines organized at the city of Makkah in the kingdom of Saudi Arabia is considered one of the largest yearly recurring mass gatherings worldwide. The officially published number of pilgrims is approximately 3–4 million, originating from 184 countries representing all continents of the world [2]. The annual number of pilgrims had increased substantially during the last years from 58,584 in 1920 to 3,161,573 in 2012 [2].
Each year, pilgrims gather for Hajj between the 8th and 13th day of the 12th month of the Islamic lunar calendar (Dhul-Hijjah). The Hajj manifested its health challenges since pilgrims come from different parts of the world and represent a mixture of socio-demographic characteristics and health backgrounds, which could subject the pilgrims to various health risks, which makes them prone to many infectious diseases, injuries, and even death while attending such a huge event [3]. Hajj is known to be a spiritually, physically, mentally, and emotionally demanding experience. Thorough medical checkups 1 or 2 months before going for Hajj is highly recommended, particularly for pilgrims who are known to have chronic illnesses, mainly cardiovascular disease. Most patients affected by heart failure, recent myocardial infarction, serious arrhythmias, unstable angina, uncontrolled hypertension, or had recent cardiac surgery should not be considered fit for attending and performing Hajj [4–8].
Recent official published data outlined that cardiovascular disease has become the leading cause of death among pilgrims during Hajj [5]. Another fact is that many pilgrims had cardiac arrests outside of hospitals available at the Hajj holy shrines, at their accommodations or nearby premises, and although adequate healthcare and emergency medical service units were allocated nearby, there was a delay or inability to provide resuscitation in an appropriate time [6].
Yousuf et al. [6] studied the medical problems among Hajj pilgrims that were admitted to King Abdul Aziz Hospital in 1995 in Medina and identified ischemic heart disease, diabetes mellitus, and respiratory infection (pneumonia) as the most commonly reported illnesses during Hajj. In the past number of years, cardiovascular diseases started to manifest as the leading cause of mortality during Hajj and of intensive care unit (ICU) admission. In 2004, a study analyzed hospital admissions during Hajj with regard to pilgrims’ geographical origin, and it identified myocardial infarction as the major cause of ICU admission of seven hospitals located in the holy shrines (four in Mena and three in Arafat), followed by pneumonia, bronchial asthma, chronic obstructive pulmonary disorder (COPD), and pulmonary edema. Cardiovascular causes such as myocardial infarction and left ventricular failure occurred with the highest frequencies (about 60%) of the ICU admissions [7].
The Ministry of Health in the Kingdom of Saudi Arabia officially declared deaths as a result of cardiovascular diseases as the highest recorded during Hajj season 2005 [8]. In addition, Madani [9] published that cardiovascular illnesses caused about 64% of all admission to the ICUs during Hajj of the Islamic year 1424 (2004) in which the most common diagnosis was myocardial infarction and 10.7% mortality (68.6% older than 40 years). Al Shimemeri [5] found that about half of the officially recorded deaths resulted from myocardial infarction alone and that 57.9% of all admissions to the ICUs were due to cardiovascular illnesses (31.5%) and hypertension (26.4%) [5]. A review article published in 2006 [10] examined the pattern of transfer of care from the emergency rooms of the holy shrines, Makkah and Medina hospitals to the ICUs during the Hajj of 2002 and found that cardiovascular diseases were the most reported causes of death (45.8%) and that hypertension was responsible for 2.7% of the deaths.
Cardiopulmonary resuscitation (CPR) is a crucial part of basic life support and a potential life saver associated with survival prevention of sudden death [8]. It was implemented in the clinical practice for more than 50 years during which it had several modifications. Nevertheless, the clinical outcomes reported, particularly the rate of survival to discharge, has not significantly improved since the year 2005 [9].
Therefore, the current clinical resuscitation research of focuses mainly on influencing the factors affecting the CPR outcomes and increasing the resuscitation effectiveness [10]. Cardiac etiology, shockable rhythms, CPR duration ≤ 15 min, and total adrenaline dose ≤ 5 mg were suggested as predictors of a favorable outcome, whereas traumatic etiology, previous terminal illness, or multiple organ failures were predictors of an unfavorable outcome [11].
In the city of Medina, most of the pilgrims are accommodated around the prophet’s mosque in hotels and buildings. Al Ansar Hospital, the nearest hospital to the prophet’s mosque (about 1 km away), is the first and nearest hospital to receive the medical emergencies, including cardiac arrest cases. However, despite the proximity to the place of the event, patients usually reach the hospital late because of overcrowding, which necessitated the development of strategies and protocols to deal with these conditions including CPR.
In this study, we aim to evaluate the outcome of CPR done to pilgrims in Medina city during Hajj, either inside Al Ansar Hospital or brought from outside, and to analyze the difference between outside and inside the hospital arrest and compare the results with other published reports.
2. MATERIALS AND METHODS
A prospective cohort study of the outcome of 426 pilgrim patients seen and treated at Al Ansar Hospital in Medina, Saudi Arabia during Hajj period (2 months from 15th of Zul-Qaida to 15th of Muharram, lunar months) from 1424 to 1427 H and 1430 to 1431 H corresponding to January 2004–December 2007 and January 2010–December 2011 was done. The study was approved by the research ethical committee at Al Ansar General Hospital, Medina, Saudi Arabia. A digital database file was structured for the study protocol and data designated only to pilgrims arresting during the specified Hajj period. All the digital files were saved on a hard drive for analysis.
The computerized database file for each patient included the personal data (age, sex, and nationality), the clinical data (co-morbid diseases, especially cardiac diseases), and the study data which was specified as: the location where the arrest happened; witnessed arrest versus unwitnessed arrest; monitored versus unmonitored; the actual time from arrest to the initiation of CPR; the initial recorded rhythm [ventricular tachycardia (VT), ventricular fibrillation (VF), or asystole]; a direct current shock delivered or not; intubation was done or not; the actual time needed to restore spontaneous circulation; the length of spontaneous circulation persistence (<20 min, >20 min but <24 h, or >24 h); vasopressor drugs administered or not; the actual duration of CPR; and the actual level of consciousness following CPR (immediate return to consciousness, coma < 24 h, coma > 24 h).
The criteria used in the study were from the Utstein Template and followed the recommendations of the International liaison committee on resuscitation. All patients were managed according to the guidelines of the advanced cardiac life support (ACLS) recommended by the American Heart Association. Associated factors for survival were evaluated using logistic regression analysis, and the collected data were analyzed by the SPSS program release 22 (IBM Corp., Armonk, NY, USA).
3. RESULTS
A total of 426 pilgrims who were diagnosed to have had cardiac arrest were included in the study. Of this, 287 (67.4%) were males and 139 (32.6%) were females, (ratio 2.1:1). The mean age was 64.0 ± 12.0 years.
The main risk factors in the study population were: age >50 years in 309 (72.5%) patients, cardiovascular diseases in 148 (34.74%) patients, diabetes mellitus in 91 (21.36%) patients, COPD in 26 (6.1%) patients, chronic liver disease in 25 (5.87%) patients, and trauma in 22 (5.2%) patients.
The majority of pilgrims were from Asian countries (mainly Indonesia, Pakistan, Iran, Bangladesh, India, Saudi Arabia), followed by African countries (mainly Egypt, Sudan, Nigeria, Algeria, South Africa), and Europe (mainly Turkey, Russia, Albania, France) (Figure 1).
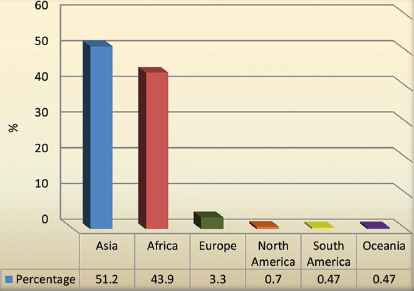
Geographic distribution of the study population
3.1. Outside the Hospital Cardiac Arrest
A total of 252 (52.2%) patients had an outside the hospital cardiac arrest. Of them, 163 (64.7%) were received in asystole and 89 (35.3%) in pulseless electrical activity (PEA). The mean duration of CPR time was 22.5 min (range, 15–30 min). All were mechanically ventilated and started on inotropic support. None of the cases immediately regained consciousness, and all of them were admitted to the ICU. Immediate survival rate was 23%. Survival after 24 h was 16%. Survival to discharge was 5%.
3.2. Inside the Hospital Cardiac Arrest
A total of 174 patients had an inside the hospital cardiac arrest. Of them, 35 (20.1%) were received in asystole, 85 (48.9%) in PEA, 36 (20.9%) in VT, and 16 (9.2%) in VF. The time of initiation of CPR was 32.5 s (range, 25–40 s). The mean duration of CPR was 12.5 min (range, 5–20 min). Around 70% of them regained consciousness immediately, and none of them required inotropic support. The immediate survival rate was 60%. Survival after 24 h was 43%. Survival to discharge was 30% (Tables 1 and 2; Figure 2).
| Cardiac arrest outside the hospital | |||||||
| Data & outcome | 1424 (2004) | 1425 (2005) | 1426 (2006) | 1427 (2007) | 1430 (2010) | 1431 (2011) | n (%) |
| Cases (N) | 43 | 49 | 39 | 38 | 36 | 47 | 252 |
| Immediate survival | 10 | 13 | 7 | 7 | 12 | 10 | 59 (23) |
| Alive for >24 h | 10 | 7 | 7 | 4 | 5 | 6 | 39 (16) |
| Survived to discharge | 1 | 2 | 3 | 2 | 2 | 1 | 14 (5) |
| Cardiac arrest inside the hospital | |||||||
| Cases (N) | 31 | 50 | 20 | 23 | 22 | 29 | 174 |
| Immediate survival | 25 | 20 | 12 | 20 | 12 | 18 | 105 (60) |
| Alive for >24 h | 12 | 15 | 12 | 18 | 6 | 12 | 75 (43) |
| Survived to discharge | 7 | 11 | 8 | 10 | 6 | 9 | 52 (30) |
Cardiac arrest inside and outside the hospital
| Data and outcome | Outside the hospital | Inside the hospital | Combined |
|---|---|---|---|
| Cases studied (N) | 252 | 174 | 426 |
| Immediate survival rate | 59 (23) | 105 (60) | 164 (39) |
| Hours alive after 24 h | 39 (16) | 75 (43) | 114 (27) |
| Discharged from the hospital | 14 (5) | 52 (30) | 66 (15.5) |
Data are presented as n (%).
Combined results of 6 years
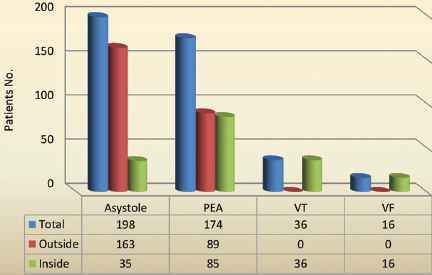
The initially monitored rhythm recorded at presentation of outside and inside the hospital pilgrims. PEA, pulseless electrical activities; VF, ventricular fibrillation; VT, ventricular tachycardia
Univariate logistic regression analysis outlined that the following factors were associated with survival following completion of CPR: cardiac arrest inside the hospital compared with arrest outside the hospital [odds ratio (OR) = 2.7, 93% confidence interval (CI) = 1.24–5.30, p = 0.01] and asystole as the initial cardiac rhythm at presentation (OR = 0.46, 94% CI = 0.23–0.89, p = 0.03).
Multivariate logistic regression analysis outlined that cardiac arrest within the hospital was associated with survival at the end of CPR (OR = 2.51, 95% CI = 1.06–5.99, p = 0.04).
Univariate logistic regression analysis outlined that the following factors were associated with survival at the discharge time from the hospital: cardiac arrest inside the hospital (OR = 8.3, 95% CI = 1.09–65.63, p = 0.04) and the duration of CPR (OR = 0.92, 95% CI = 0.86–0.95, p = 0.001).
Multivariate logistic regression analysis outlined that cardiac arrest inside the hospital was associated with survival at the discharge time from the hospital (OR = 8.68, 95% CI = 1.01–74.6, p = 0.05) and the duration of CPR (OR = 0.92, 95% CI = 0.87–0.98, p = 0.01).
4. DISCUSSION
Our involvement at Al Ansar Hospital in the medical service during many Hajj seasons led to the observation that the majority of the pilgrims are older than 50 years and have multiple co-morbid illnesses with a history of heart disease, hypertension, diabetes, or chronic lung diseases. These debilitating diseases along with unaccustomed physical exertion, new environment, and at times, noncompliance to prescribed medications put them at increased risk of deterioration even up to a cardiac arrest.
In our study, the majority of pilgrims brought from outside the hospital were elderly who have a history of significant coronary artery disease or chronic lung diseases. The main predictors of successful resuscitation included asystole, the CPR duration, and cardiac arrest within the hospital, while parameters such as cardiac rhythm, co-morbid diseases, and airway management had no significant influence on the survival. In patients who had a witnessed arrest, the majority of them had VF/VT or respiratory arrest secondary to COPD and severe asthma leading to PEA.
Out of the patients of inside the hospital cardiac arrests, 20% had arrested in the emergency room, 40% had arrested in the ICU, and 40% had arrested in the medical wards. Patients who arrested inside the hospital were recognized immediately and responded promptly. Nonsurvivors included those with significant co-morbid diseases.
The prompt initiation of CPR could double the chance of survival of a victim [12–23]. Therefore, a regulation was issued in 2010 stating that all health service personnel working in Al Ansar Hospital and participating in Hajj medical service should have a valid CPR certificate as a job prerequisite, and by 2011, all heath service personnel were CPR certified. Our results in regard to immediate survival rate, alive after 24 h, and discharge from the hospital were comparable to the international reported figures (Table 3).
| Outcome | Ebell et al. [22] 9838 cases | McGrath [24] | DeBard [25] 1073 cases | BRESUS study [26] 3795 cases | Our study 426 cases |
|---|---|---|---|---|---|
| Immediate survival rate | — | — | — | 39 | 164 (38.5) |
| Alive after 24 h | — | 38 | 39 | 28 | 114 (27) |
| Discharge from the hospital | Average survival 3–27 | 15 | 17 | 17 | 66 (15.5) |
Data are presented as % or n (%).
Comparison between our study and internationally published studies
The survival rate of all emergency medical services (EMS) treated outside the hospital cardiac arrest ranges from 3% to 16%. For VF arrest, the survival rate varies from 7.7% to 39.9% [27]. Our observation is that overcrowding is a major limitation to provide the service, delaying both arrival time of health providers to the location of the event and transporting victims to the hospital. We observed that first EMS response in our study was given at the arrival of the ambulance, so time is lost between the event and arrival of the ambulance. This issue was addressed by training the employees working at the pilgrim populated places for performing the basic life support and providing automated external defibrillators (AEDs) at various locations.
Automated external defibrillator is a portable electronic machine which autonomously analyzes life-threatening cardiac arrhythmias of VF and VT in arrested victims and by defibrillation (stopping the arrhythmia) allows the heart to re-establish an effective rhythm [28]. In October 2011, The Saudi Arabia Ministry of Health installed 88 AED Plus units in the holy city of Makkah to resuscitate pilgrims who experience sudden cardiac arrest while participating in the Hajj. As a result of the consensus that large numbers of sudden cardiac arrest patients are referred to Al Ansar Hospital, especially during Hajj, an AED Plus unit was assigned to each room in the emergency department, ICU, operating theater, and medical and surgical wards. It led to a significant improvement in the results of in-hospital resuscitation as proved by our study results.
General public education of the basics of CPR, encouraging early recognition of sudden cardiac arrest victims by witnesses, and avoidance of delay in EMS arrival, which may be due to the distance or heavy traffic, are crucial factors influencing the outcome of resuscitation. To overcome the delay in EMS arrival, telephone-assisted CPR by the bystander emerged as a valuable option that increased the outcome of survival significantly [24]. In 2013, a recommendation from the Hajj medical committee lead to installation of 22 AEDs in the prophet’s mosque (the most crowded location during Hajj) in Medina, with the availability of both wired and wireless telephones beside each unit, and organizing CPR training for many civil and security employee of the prophet’s mosque.
Known cardiac patients planning to attend and perform Hajj should carefully plan their medical care prior to leaving their countries, and they should be aware that Hajj rituals are very strenuous to the degree that any physical overstress could precipitate ischemia. Acquisition of sufficient supplies of medications, compliance with doses and timing of intake, avoidance of crowded places, the performance of the rituals in organized and tranquilized manner, and the rapid reporting of any health occurrence to the closest health center is advised.
Given our statistics and involvement in the unique situation of Hajj mass gathering every year, we recommend that pilgrims having chronic illnesses should be well prepared before coming to Hajj. A complete cardiopulmonary evaluation, adequate medication supply, and education on the alarming symptoms like chest pain, breathing problems, and dizziness should be done. Furthermore, they should know their limitations in physical exertions depending on formal tests. In addition, we request the help of Hajj medical missions from different countries to have their group leaders trained in recognizing the pre-arrest symptomatology and prompt referral at that stage.
We strongly recommend reinforcement of basic life support (BLS) training and more liberal availability and use of AEDs for arrested patients by the bystanders including security officers in the prophet’s mosque and management personnel in the hotels. It will enhance immediate response to arrests until the formal EMS arrives with an ambulance and will have a significant impact on the survival and outcome of these patients. All grand hotels around the prophet’s mosque should have ambulances, AEDs, and trained employees to perform CPR.
All allocated healthcare providers (physicians, nurses, and technicians) working in dispensaries around the prophet’s mosque should be BLS and ACLS certified. All emergency department allocated healthcare providers (physicians, nurses, and technicians) should be well aware of not only resuscitation but post-resuscitative care also. Beside pilgrims, we recommend a comprehensive community-oriented training program for BLS and CPR for the residents of Medina city, including college students and security forces.
5. CONCLUSION
We conclude that during Hajj, CPR inside the hospital was associated with a more favorable clinical outcomes as compared with outside hospital arrest. Patients arresting outside of the hospital are much less likely to survive due to the lack of immediately trained help and the delay of arrival of aid due to overcrowding. Sudden cardiac arrest leading to death could be minimized if CPR and defibrillation are delivered before EMS arrive.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
REFERENCES
Cite this article
TY - JOUR AU - Bader Hamza Shirah AU - Fareed Abdulmuhsen Al Nozha AU - Syed Husham Zafar AU - Hussain Mohammed Kalumian PY - 2019 DA - 2019/03/27 TI - Mass Gathering Medicine (Hajj Pilgrimage in Saudi Arabia): The Outcome of Cardiopulmonary Resuscitation during Hajj JO - Journal of Epidemiology and Global Health SP - 71 EP - 75 VL - 9 IS - 1 SN - 2210-6014 UR - https://doi.org/10.2991/jegh.k.190218.001 DO - 10.2991/jegh.k.190218.001 ID - Shirah2019 ER -
