Epidemiology of Meningitis in Oman—Implications for Future Surveillance
- DOI
- 10.2991/j.jegh.2018.02.001How to use a DOI?
- Keywords
- Haemophilus influenzae; Lumbar puncture; Meningitis; Neisseria meningitides; Oman; Streptococcus pneumoniae; Surveillance
- Abstract
Objectives:
This study aimed to understand the epidemiology of meningitis cases admitted to hospitals in Oman and to identify any changing microbial patterns from the introduction of the new vaccines.
Methods:
A retrospective analysis of all cases of meningitis reported through a national surveillance system. Meningitis is a notifiable disease.
Results:
Of a total of 581 cases of meningitis from the period between January 1, 2005 and December 31, 2013, 15% (88) were confirmed to be bacterial in origin and 7.2% (42/581) viral. In 50.9% (296) of patients with suspected pyogenic meningitis, no specific bacterial pathogen were identified, and in 26% of cases (151) a cerebrospinal fluid study could not be undertaken. Among 88 cases with confirmed bacterial pathogens the organisms identified were Streptococcus pneumoniae (65.9%), Neisseria meningitides (18.2%), Haemophilus influenzae (6.8%), and other organisms (9.1%). The peak incidence was in children <2 years of age (39.4%). It showed notable decline in H. influenzae cases as well as pneumococcal meningitis cases, possibly indicative of the successful immunization program.
Conclusion:
A drop in H. Influenzae and pneumococcal meningitis cases was possibly the effect of the introduction of vaccines. It shows the need for improving diagnostic accuracy, laboratory capacities, and quality of surveillance reporting.
- Copyright
- © 2018 Atlantis Press International B.V.
- Open Access
- This is an open access article under the CC BY-NC license (http://creativecommons.org/licences/by-nc/4.0/).
1. INTRODUCTION
Currently, bacterial meningitis continues to take lives and is prevalent worldwide. Although there has been a remarkable reduction in case fatality rates resulting from the introduction of antibiotics, their use against bacterial meningitis has reduced case fatality rates to no more than 25% [1]. Bacterial meningitis continues to be a leading cause of emergency admission to hospitals despite numerous improvements in vaccine development and use [2,3]. Microbiology laboratories play an important role, not only in the primary identification of the causative organism and its antibiotic susceptibility pattern, but also in providing valuable information regarding the common incriminating pathogens in that area, and which drugs to start empiric treatment with [4].
Acute bacterial meningitis, a disease that necessitates immediate diagnosis and aggressive treatment, is termed as a medical emergency. In the majority of cases, treatment for bacterial meningitis has to be given before laboratory results confirm the specific etiological organism. The decision to opt for antimicrobial treatment is based on the most prevalent pathogen known to a specific region as well as the age of the patient and their antibiotic susceptibility [5,6].
Pneumococcal meningitis is the principal cause of bacterial meningitis compared with meningitis caused by either Neisseria meningitides or Haemophilus influenzae [7]. Pneumococcal meningitis breaks out periodically and in epidemics in many parts of the globe and the disease has a high-case fatality rate. Group B streptococci, Escherichia coli, Listeria monocytogenes, and other organisms acquired through the birth canal compose the majority of the bacterial causes of neonatal meningitis. Neonatal meningitis could also be blamed on infant exposure to Klebsiella–Enterobacter–Serratia group found in environments infants may be exposed to Ministry of Health (MoH) Oman [1], Simonsen et al. [8], Kaufman and Fairchild [9].
Viral meningitis is comparatively commonplace but rarely an extreme clinical syndrome and is characterized by an abrupt onset of fever with meningeal signs and symptoms. Similar to pneumococcal meningitis, viral meningitis breaks out periodically worldwide or in epidemics; however, case fatality rates are generally low. Infections, mostly in those contracted by children, may have the potential for a long-term chronic condition, but this is seldom severe and a full recovery is expected [1]. Furthermore, active infection hardly ever lasts more than 10 days [10]. In settings where the policy of prereferral antibiotics for meningitis is practiced it is possible that it may cause a negative result for cerebrospinal fluid (CSF) and blood culture resulting in some bacterial meningitis being misclassified as viral [1].
Prior to the introduction of the H. influenzae type b (Hib) vaccine in routine infant immunization programs, Hib meningitis was well known as a common source of childhood meningitis in many areas [11]. The vaccine is increasing in its availability globally and its use is proliferating; notably in the past 20 years, the epidemiology of meningitis has undergone substantial changes [11–15]. The introduction of the conjugate Hib vaccine (in October 2001) in the Expanded Programme of Immunization (EPI) in Oman and the more recent introduction of the pneumococcal conjugate vaccine (PCV-7 in November 2008, PCV-10 in November 2010, and PCV-13 in December 2011) must have influenced the epidemiology of the disease in Oman [16].
This study was conducted to describe the epidemiology of meningitis cases admitted to hospitals in Oman and reported through a surveillance system. We also attempted to explore the changing microbial pattern in relation to the introduction of Hib and pneumococcal vaccines and to compare the results of previous similar studies from Oman.
2. MATERIALS AND METHODS
We have completed a retrospective analysis of all cases of meningitis reported through a surveillance system to the Department of Communicable Diseases Surveillance and Control, Ministry of Health, Oman from January 1, 2005 to December 31, 2013. Communicable disease surveillance in Oman covers all health institutions in the country and it is mandatory to notify all communicable diseases prioritized for notification, and meningitis (bacterial and viral) is listed in this prioritized group. The surveillance is decentralized, and because monitoring systems are in place we expect the cases reported through surveillance to be representative of incident cases for the period in the country. These reports formed the records from which data required for the study was extracted into a database. All the cases were examined for basic patient demographic data including age, sex, country of origin, history of travel, meningitis vaccination status, underlying conditions, microbiologic etiology, and clinical outcome. The following clinical and microbiologic case definitions of meningitis were used in this study: (1) a diagnosis of clinical meningitis was made if reporting was based only upon clinical assessment with features including fever and more than one of the following: severe headache, neck stiffness and pain, nausea and vomiting, altered mental status, and photophobia. In children <2 years of age, diagnosis was made if a case had both a sudden onset of fever ≥38.5°C, and irritability or bulging fontanels; (2) confirmed bacterial meningitis was defined by a Gram-positive stain of CSF, by antemortem or postmortem culture isolation of a relevant microorganism from CSF or blood, or by discovery of bacterial antigens in CSF; (3) meningitis was presumed to be bacterial in origin (suspected bacterial meningitis) based upon clinical presentation and if one or more of the following features were seen in CSF examination: turbidity, neutrophilic pleocytosis [>500 white blood cells (WBCs)/mm3], or a low glucose level (<50 mg/dL) without a Gram-positive stain; (4) suspected viral meningitis was presumptively diagnosed on clinical grounds and by the exclusion of bacterial meningitis, and the presence of one or more of the following: normal CSF glucose or mild increase (50 mg/dL) in CSF protein, moderate increase in CSF WBCs (<500/mm3) and lymphocyte predominance (50%), or an epidemiologic link to a confirmed case; and (5) confirmed viral meningitis was defined as a suspected case with laboratory confirmation [e.g., virus culture isolation or positive CSF polymerase chain reaction (PCR)].
Infections caused by Mycobacterium tuberculosis were excluded from the study. The data that were obtained from the communicable diseases surveillance system notification database in a Microsoft Excel (Microsoft office professional plus 2010, Microsoft corporation) and SPSS Version 20 (SPSS Inc) format. The data were cleaned and analyzed using an Excel spreadsheet and SPSS version 20. No personal identifiers were present in the data and hence there were no issues with regard to patient confidentiality or ethical issues involved in the study. The permission to collect, use, and publish this data was granted by the Ministry of Health because this was surveillance data which is intended for such purposes.
3. RESULTS
During the 9-year review period, 581 cases were reported as suspect or confirmed meningitis and an overall summary is given in Table 1. The study population consisted of 75% (437) Omanis and rest were expatriates. A total of 228 (39%) were females and 353 were (61%) males. Analysis of age distribution showed that 413 (71%) were children <13 years of age. Among the children, 55% were under 2 years of age (Figure 1) and 54 were neonates. In total, 101 (17%) cases were reported from tertiary level hospitals whereas the rest were from secondary level hospitals. One hundred and fifty-one cases (26%) were not subjected to CSF examination mostly due to nonconsenting by parents and this is mostly from one place (Figure 1). The time and place distribution of the cases are given in Table 1. Of the 384 (66%) cases that were reported as bacterial meningitis, 88 (15%) were confirmed with organisms identified and 296 (51%) were reported as suspected bacterial meningitis and treated accordingly. In the review period, 42 cases of suspected viral meningitis and four cases of fungal meningitis (all in immunocompromised patients) were also reported. During 2013, viral studies were initiated and two cases were confirmed enterovirus meningitis.
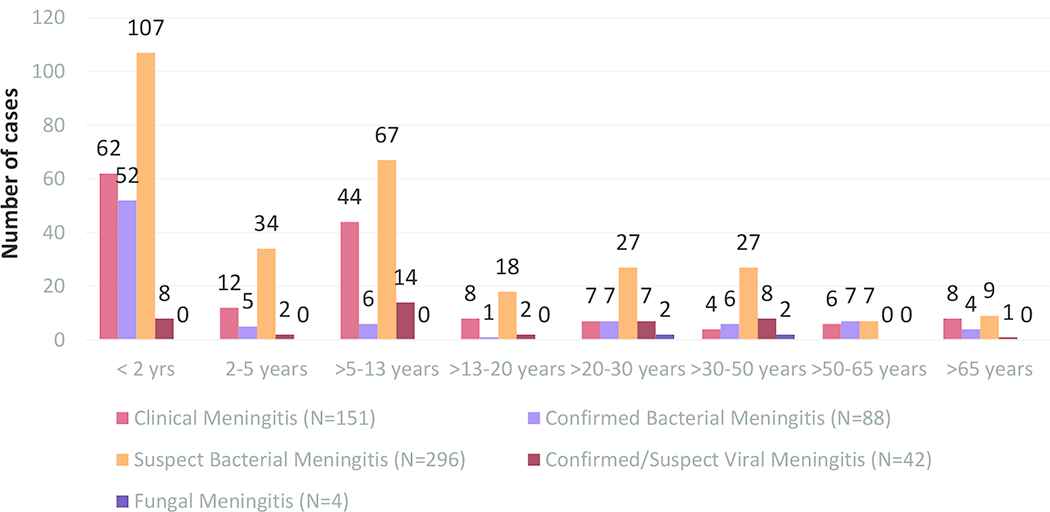
Classification of meningitis cases based on age groups (n = 581)
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | Total | |
|---|---|---|---|---|---|---|---|---|---|---|
| Meningitis surveillance performance trends (diagnostic confirmation) No. of cases | ||||||||||
| Suspected meningitis | 58 | 25 | 36 | 41 | 21 | 28 | 36 | 19 | 32 | 296 |
| Confirmed meningitis (lab result available) | 16 | 18 | 22 | 18 | 10 | 11 | 14 | 15 | 10 | 134 |
| Bacterial | 11 | 11 | 13 | 18 | 7 | 7 | 10 | 2 | 9 | 88 |
| Viral | 4 | 6 | 8 | 0 | 2 | 3 | 4 | 12 | 3 | 42 |
| Fungal | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 4 |
| Clinical meningitis (No. CSF study) | 2 | 19 | 15 | 23 | 7 | 24 | 15 | 12 | 34 | 151 |
| Total (n = 581) | 76 | 62 | 73 | 82 | 38 | 63 | 65 | 46 | 76 | 581 |
| Meningitis surveillance performance trends (region wise notifications) Number of cases | ||||||||||
| Muscat | 15 | 13 | 15 | 15 | 7 | 6 | 4 | 11 | 5 | 91 |
| South Batinah | 3 | 6 | 5 | 2 | 2 | 8 | 9 | 6 | 14 | 55 |
| North Batinah | 28 | 24 | 26 | 37 | 14 | 31 | 22 | 9 | 36 | 227 |
| Dhahira | 5 | 1 | 3 | 2 | 1 | 2 | 3 | 2 | 2 | 21 |
| Dhakliyah | 6 | 2 | 4 | 6 | 5 | 0 | 1 | 0 | 3 | 27 |
| North Sharqiyah | 7 | 7 | 10 | 7 | 3 | 2 | 6 | 6 | 12 | 60 |
| South Sharqiyah | 1 | 2 | 6 | 6 | 3 | 4 | 3 | 4 | 1 | 30 |
| Musandam | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Buraimi | 0 | 0 | 0 | 0 | 0 | 2 | 2 | 2 | 0 | 6 |
| Dhofar | 10 | 6 | 4 | 7 | 3 | 8 | 15 | 6 | 3 | 62 |
| Total (n = 581) | 76 | 62 | 73 | 82 | 38 | 63 | 65 | 46 | 76 | 581 |
CSF, cerebrospinal fluid.
Summary of meningitis surveillance process during the review period
The organisms that were identified from CSF in the surveillance data are shown with annual trends and age distribution in Figures 2 and 3. It is to be noted that only a few cases of H. influenzae meningitis was reported during the period. At the same time there is a clear decline in pneumococcal meningitis reports in the latter years of the review period. Although there was reduction in the proportion of confirmed pneumococcal cases among positive cultures during the study period the trend was not statistically significant.
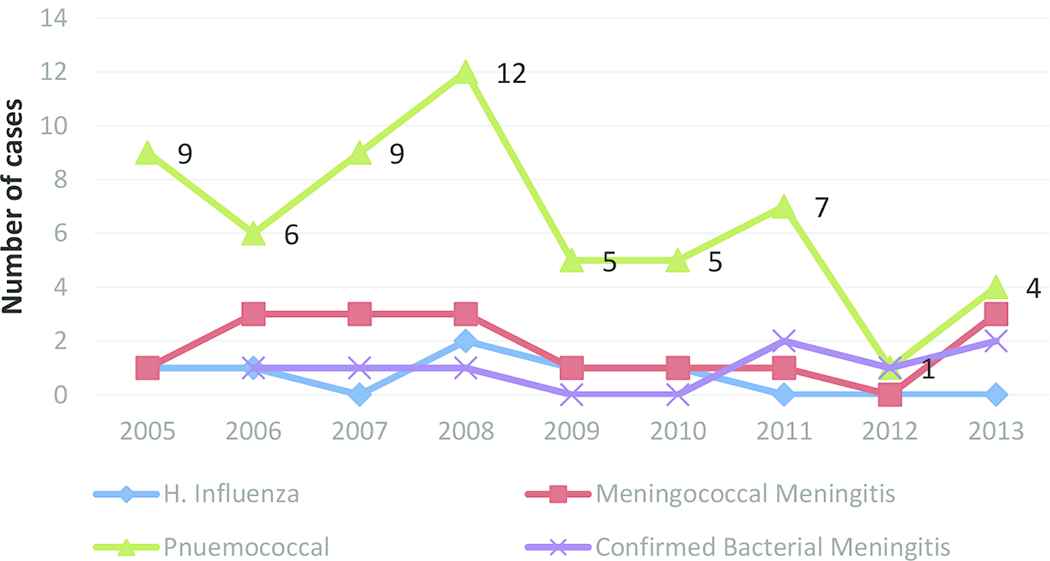
Trend in organisms 2005–2013 (n = 88)
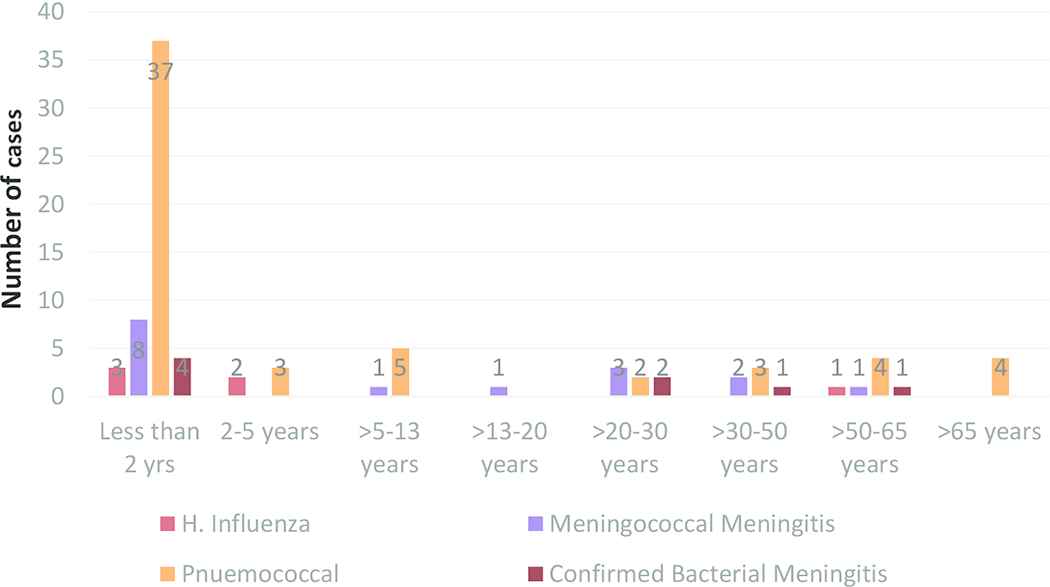
Organisms identified based on age groups (n = 88)
4. DISCUSSION
This retrospective review of meningitis cases reported through a passive surveillance process has shown that a significant proportion of the cases notified were reported to be of bacterial etiology. Based on our case definitions, 296 cases were classified as suspect bacterial meningitis and 88 cases were reported with organisms identified. Viral etiology was attributed based on clinical and CSF findings alone as facilities for viral studies were not established during this period.
A majority (71%) of the cases reported occurred in children <13 years of age and a major proportion among them were younger than 2 years of age. Acute bacterial meningitis is one of the most common infections in children contributing much to morbidity and mortality [5,17,18]. Hib, Streptococcus pneumoniae and N. meningitides were the most common organisms identified among the reported cases and this is concurrent with the pattern that is seen in most published studies [19]. Hib cases were confined to infants and it was noted that no cases were reported since 2009. Similarly, there is also a reducing trend seen in pneumococcal meningitis. In a retrospective review of 41 cases that described the epidemiology of invasive pneumococcal disease (IPD) in Omani children <5 years of age admitted in 2006 in tertiary care facilities of the Muscat Governorate, the annual incidence of IPD was 26.1 per 100,000 in children <2 years of age and 18.6 per 100,000 in children <5 years of age. This can be considered as an indication of the incidence of IPD in the time prior to the introduction of the pneumococcal conjugate vaccine (PCV). Among the IPD cases in the above-mentioned study, 22 (54%) isolates were resistant to at least one antibiotic and 15 (37%) of the cases had a comorbid condition that they were aware of Al Awaidy et al. [20]. The changes with respect to incidence of Hib and pneumococcal disease may be attributed to the introduction of Hib and pneumococcal vaccines in the EPI schedule in Oman from 2001 and 2008, respectively. The epidemiology of meningitis has changed significantly in most parts of the world wherever appropriate vaccines were introduced into immunization schedules [5,16,19,21–28].
In our study, meningococcal cases were mainly reported from older age groups. Invasive meningococcal disease, in meningitis or bacteremia form, has a case fatality rate of 8–15% despite antibiotics and this disease also poses the risk of long term neurological deficits. High risk populations for disease include infants, adolescents, those with asplenia or complement deficiencies, and potentially those with human immunodeficiency virus (HIV) [19,28–30]. Sporadic cases were reported in Oman during the review period of this study. Meningococcal vaccines are not included in the childhood vaccination program. However, in Oman, meningococcal polysaccharide (serogroup ACYW135) vaccine is given to people traveling to Saudi Arabia for pilgrimage and to travelers to countries of the meningitis belt. The use of conjugate meningococcal vaccines has changed the course of the epidemiology of meningitis globally, regardless of economy; high- and low-income countries have both benefitted from vaccination. Outbreaks at university campuses of serogroup B disease have garnered additional attention to the recent creation of a novel serogroup B vaccine now approved in various countries [29,30]. This also suggests the need for upgrading laboratory facilities for subtyping.
Viral meningitis cases were reported in increasing numbers during the period of review. As facilities for viral studies of CSF became established in 2013, enterovirus meningitis was reported. Non-polio enteroviruses are reported to be the most common cause of viral meningitis in the United States, although only a small number of those infected with enteroviruses will develop meningitis [31].
Out of 384 cases of bacterial meningitis, 296 were found to have a negative CSF gram stain/culture. This group of patients poses a diagnostic challenge. They are treated empirically and remain without identified etiology. Increasing diagnostic capabilities such as the introduction of PCR including arboviral can improve diagnostic yield in patients with meningitis and a negative CSF gram stain [32,33]. We noted a considerably lower rate of diagnostic lumbar punctures (LPs) in our study, two-thirds of the cases without LP were children younger than 13 years of age. This sheds light on the idea that many severely ill children were treated lacking an accurate diagnostic test for meningitis. Such lower rates were found to be reported in settings where few resources were available and the patient to physician ratio is comparatively high, and this may make it unfeasible for eligible and consenting patients to undergo LPs. However, resource limitation does not seem to be a contributor for lower rates of LP in Oman. Unrecognized and not formally diagnosed bacterial meningitis is connected to lower rates of medical care use and overall childhood hospitalization, higher rates of childhood fatalities from unclear causes, and pointedly lower reported rates of meningitis in children [11,34]. A study that specifically explored the factors that influence parental decision to refuse LPs in GCC countries showed that approximately 44% of parents are afraid of the idea of their child having an LP and did not consent to the procedure. Some of the factors for refusing an LP were that they knew someone who had subsequent complications from LP [odds ratio (OR) = 8.7], that they felt it unnecessary (OR = 7.9), or that it caused complications (OR = 12.5). Furthermore, of the consenting parents, those who knew about the severe complications caused by meningitis comprised a much greater percentage than those who were less aware [35]. These findings suggest the need to plan appropriate counseling strategies to reduce the refusal rates for LPs.
As stated before the data for this study were obtained from the robust passive surveillance system for communicable diseases in Oman and can be considered as representing the incidence in Oman. However, being a retrospective analysis of disease notifications reported through a passive surveillance system, has its inherent limitations. It lacks clinical details as well as outcomes. It is also subject to possible underreporting. Lack of specific diagnostic tests, such as those of molecular diagnostics, could have resulted in underestimating the true proportion of both bacterial and viral meningitis. Therefore there is a need to develop laboratory practices further for bacterial detection and identification, and this would also help to fortify regulations and articulate improved antibiotic policies. This additional step, along with better a reporting system, would improve the quality of meningitis surveillance in Oman. It is also important to note that improvements in a surveillance system for meningitis should consider narrowing it on the evolving epidemiology of meningitis consequent to the introduction of new vaccines, the changing patterns of disease-causing bacterial serotypes, and on antibiotic resistance and its influence on treatment [5].
5. CONCLUSION
The total number of meningitis cases of H. influenzae being reported through surveillance systems has shown a decline in this study period as well as based on comparison with published reports of previous years. This decline may be attributed to the introduction of the Hib vaccine in Oman since October 2001. The number of meningitis cases caused by other pathogens such as S. pneumoniae and N. meningitides were also suggestive of a declining trend. Along with the need for improved diagnostic facilities the study emphasizes the improvements needed in surveillance for tracking effectively the epidemiology of meningitis in the country.
CONFLICTS OF INTEREST
None declared.
REFERENCES
Cite this article
TY - JOUR AU - Padmamohan J. Kurup AU - Seif Al-Abri AU - Salim Al-Mahrooqi AU - Amina Al-Jardani AU - Shyam Bawikar AU - Bader Al-Rawahi AU - Idris Al-Abaidani PY - 2018 DA - 2018/12/31 TI - Epidemiology of Meningitis in Oman—Implications for Future Surveillance JO - Journal of Epidemiology and Global Health SP - 231 EP - 235 VL - 8 IS - 3-4 SN - 2210-6014 UR - https://doi.org/10.2991/j.jegh.2018.02.001 DO - 10.2991/j.jegh.2018.02.001 ID - Kurup2018 ER -
