Serological Detection of Ebola Virus Exposures in Native Non-human Primates of Southern Nigeria
- DOI
- 10.2991/j.jegh.2018.05.001How to use a DOI?
- Keywords
- Filoviridae; monkey; wildlife; zoonosis
- Abstract
Ebola viruses (family: Filoviridae) are the cause of Ebola virus disease (EVD), a highly fatal illness characterised by haemorrhagic fever syndrome in both humans and non-human primates (NHPs). West Africa was the epicentre of the 2013–2015 EVD epidemic which caused the death of over 11,000 people, including eight casualties in southern Nigeria. Antibodies to filoviruses have been detected among NHPs in some countries, but there is no documented evidence of exposures to filoviruses among NHPs in Nigeria. From August 2015 to February 2017, a total of 142 serum samples were obtained from individual captive and wild animals, belonging to 11 NHP species, in southern Nigeria, and screened for species-specific antibodies to filoviruses belonging to the species; Zaire ebolavirus [Ebola virus (EBOV)], Sudan ebolavirus [Sudan virus (SUDV)], and Marburg marburgvirus [Ravn virus (RAVV)]–using a modified filovirus species-specific ELISA technique. Of the sera tested, 2.1% (3/142) were positive for antibodies to EBOV. The entire 142 sera were negative for SUDV or RAVV. These findings point to the existence of natural exposures of NHPs in southern Nigeria to EBOV. There is need to discourage, the uncontrolled hunting of NHPs in Nigeria for public health safety.
- Copyright
- © 2018 Atlantis Press International B.V.
- Open Access
- This is an open access article under the CC BY-NC license (http://creativecommons.org/licences/by-nc/4.0/).
1. INTRODUCTION
The Ebola virus disease (EVD) epidemic which occurred in West Africa between 2013 and 2015, and was declared a public health event of international concern, left critical lessons for disease surveillance and emergency preparedness [1]. Therefore, surveillance of wildlife (including non-human primates) for exposure to the virus and other major filoviruses at selected locations in the sub-region has become a priority activity. The family Filoviridae, order Mononegavirales, comprises viruses with single-stranded, negative-sense, non-segmented RNA genomes [2]. The most important genera in the family Filoviridae are Ebolavirus and Marburgvirus–both are endemic to Africa. Ebola viruses are the causative agent of EVD, a highly fatal illness characterised by haemorrhagic fever syndrome in both humans and NHPs [3].
There are five distinct virus species in the genus Ebolavirus; Zaire ebolavirus [Ebola virus (EBOV)], Sudan ebolavirus [Sudan virus (SUDV)], Taï Forest ebolavirus [Taï Forest virus (TAFV)], Reston ebolavirus [Reston virus (RESTV)], and Bundibugyo ebolavirus [Bundibugyo virus (BDBV)] [2]. Outbreaks of EVD caused by EBOV, SUDV or BDBV had case fatalities of up to 90% in human populations [4], while RESTV caused clinical disease in non-human primates but not in man [3].The only species in the genus Marburgvirus is Marburg marburgvirus and two viruses have been described, namely Marburg virus (MARV) and Ravn virus (RAVV) [2]. Marburgvirus disease outbreaks have not been reported in West Africa but where they have occurred elsewhere in Africa, high mortality rates were recorded [5].
The 2013–2015 EVD epidemic which occurred in West Africa caused huge losses to local, national, regional and global economies [6]. Guinea, Liberia, and Sierra Leone (the most affected countries) lost 2.2 billion USD of GDP in 2015, threatening macroeconomic stability and food security [7]. Yet, over 11,000 human lives were lost including those of 513 healthcare workers. Overall, 3.6 billion USD was spent on fighting the epidemic during the 2-year period [7,8]. In Nigeria, the first human case of EVD recorded was in July 2015 as an offshoot of the 2013–2015 epidemics [9]. At the end of the 3-month EVD epidemic in Nigeria, 20 human cases and eight deaths were recorded, and the numbers would have been higher but for the timely intervention of local health workers, at a huge cost [9,10].
Tomori and others [11] reported an EBOV/Marburg virus seroprevalence of 1.8% and 1.7% respectively, in human serum samples from Nigeria. Their report is the only peer-reviewed evidence of the occurrence of human exposures to filoviruses in the country prior to July 2015. However, antibodies to these viruses have been detected in sera of human and NHPs, even in regions such as Ethiopia, Madagascar, Chad, Kenya, Zimbabwe [12] and Cameroon [13], where the clinical disease has not been previously observed. This has raised speculations about the actual geographical range of the disease in wildlife [12,13]. Presently, there is no documented evidence of filoviruses in NHP populations in Nigeria, but antibodies to the virus have been detected in fruit bats caught within West African rainforests [14]. Bats are the presumed natural reservoirs of Ebola viruses, marburgviruses and several other zoonotic viruses [15]. Global gap analysis of infectious agents in wild primates revealed that West Africa was among the regions in the world which remained undersampled [16].
The present study was designed to investigate possible exposures of NHPs in southern Nigeria to some priority filoviruses, using species-specific recombinant and purified protein-based Enzyme-Linked Immunosorbent Assays (ELISA) adapted to EBOV, SUDV, and RAVV.
2. MATERIAL AND METHODS
2.1. Study Sites and Animal Sampling
Non-human primates enlisted for serological screening were sampled from the Zoological garden, University of Ibadan, Oyo State (7.4434°N, 3.8956°E); the Biological garden, University of Ilorin, Kwara State (8.4817°N, 4.6382°E); the Agodi gardens, Ibadan, Oyo State (7.4069°N, 3.8994°E); the Osun Osogbo sacred groove, Osun State (7.7592°N, 4.5569°E), and Centre for Education, Research and Conservation of Primates and Nature (CERCOPAN) township primate facility, Calabar, Cross River State (4.9819°N, 8.3433°E) (Fig. 1). The specimens were collected from August 2015 to February 2017. A total of 142 serum samples were obtained from captive and wild individual animals, belonging to 11 NHP species, in five locations within southwest and southeast Nigeria. The 11 NHP species were: Cercocebus sabaeus, Cercocebus torquatus, Cercopithecus erythrotis, Cercopithecus mona, Cercopithecus nictitans, Cercopithecus preussi, Cercopithecus sclateri, Cercopithecus tantalus, Erythrocebus patas, Papio anubis, and Pan troglodytes. Table 1 shows the distribution of sampled animals among the various study sites. Specimens from domestic (pet) monkeys in Oyo State, whose owners consented to the sampling of their animals, were also included in the study. Attempts were made to sample as many NHPs as permitted by the host facilities/communities. All sampling locations were within southwest Nigeria, except CERCOPAN which is located in the southeast region of the country–close to the border with Cameroon.
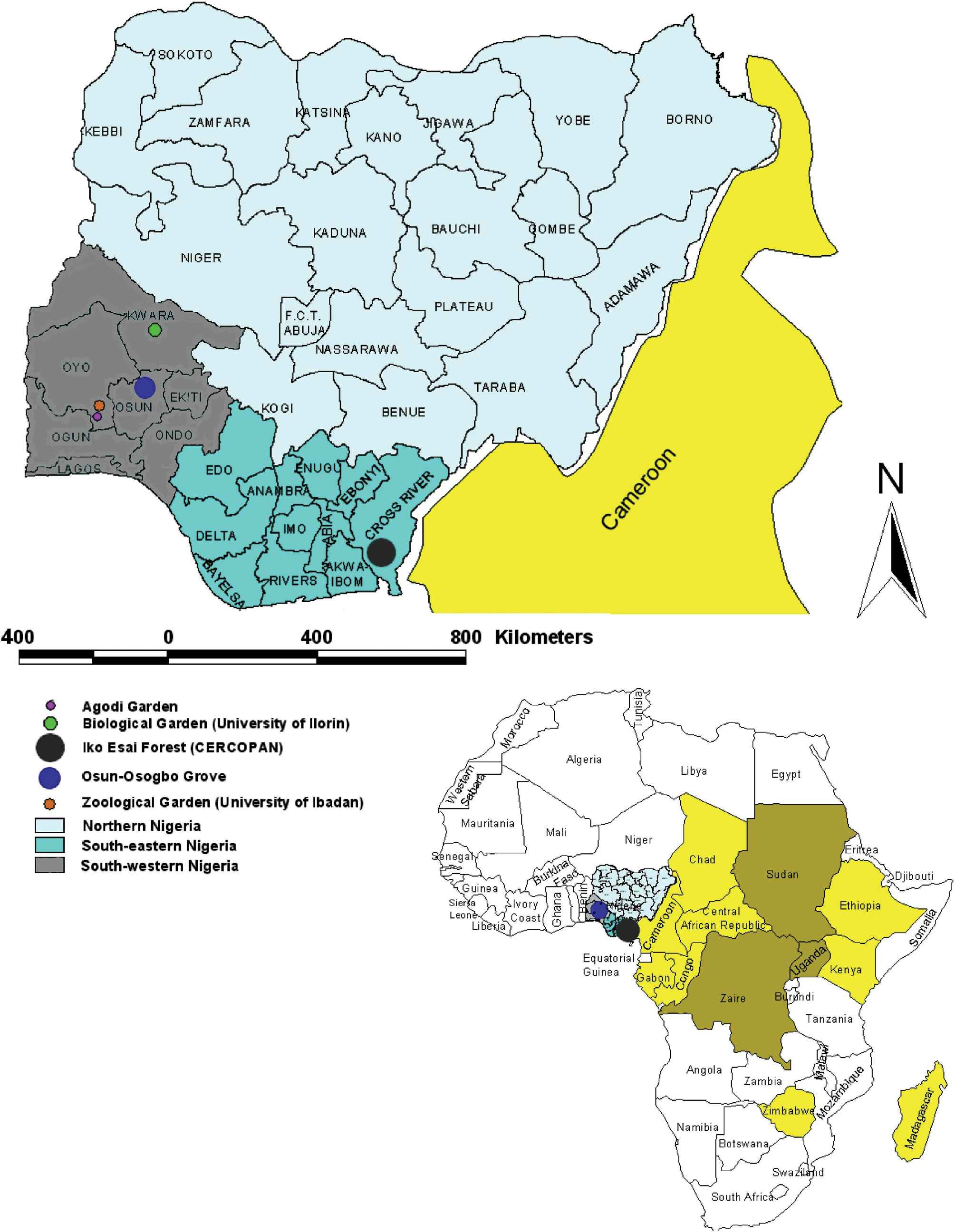
Ebola serology Study sites in southern Nigeria with insert showing extent of the virus in Africa. This figure shows the study sites in southern Nigeria with insert showing locations within Africa and in relation to Ebola virus Epicenters in Central Africa and other countries where the virus antibodies were detected in humans and/or nonhuman primates.
| Study site | Location | Type of enclosure/holding | No. of NHP in facility | No. of NHP sampled | Sampled proportion | Species of NHP# |
|---|---|---|---|---|---|---|
| Zoological garden, University of Ibadan, Oyo State | Southwest Nigeria | Captive | 30 | 27 | 90.0% | C nictitans C sabaeus C torquatus E patas M sphinx* P anubis P troglodytes |
| Biological garden, University of Ilorin, Kwara State | Southwest Nigeria | Captive | 18 | 8 | 44.4% | C sabaeus E patas P anubis* P troglodytes* |
| Agodi gardens, Ibadan, Oyo State | Southwest Nigeria | Captive | 4 | 4 | 100.0% | P anubis E patas C sabaeus |
| Osun Osogbo sacred groove, Osun State | Southwest Nigeria | Free-ranging | 60α | 4 | 6.7% | C mona |
| Pet monkeys within Ibadan, Oyo State | Southwest Nigeria | Captive | NA | 5 | NA | E patas |
| CERCOPAN primate sanctuary, Cross river State | Southeast Nigeria | Captive | 150 | 94 | 62.7% | C erythrotis C mona C nictitans C preussi C sclateri C tantalus C torquatus |
| Total | 142 |
Estimates based on curator records; NA, not available (not applicable); NHP, non-human primates;
Species of NHP available in each location: Cercocebus sabaeus, Cercocebus torquatus, Cercopithecuserythrotis, Cercopithecusmona, Cercopithecusnictitans, Cercopithecuspreussi, Cercopithecussclateri, Cercopithecustantalus, Erythrocebus patas, Papio anubis, Pan troglodytes and Mandrillus sphinx;
Species available but not sampled due to sampling restrictions by host facility or ethical reasons.
Distribution of sampled non-human primates among study sites in southern Nigeria.
Caged NHPs in zoos were darted at close range with a blowpipe loaded with the anaesthetic (ketamine hydrochloride) administered at 10 mg/kg body weight of the subject. Tame subjects were injected by hand. Locally fabricated, self-triggering traps (approximate size = 2 m × 1 m × 1 m, made of aluminium wire netting attached to a wooden frame), with guillotine-type trap door were used to trap free-ranging monkeys. Prior to trapping, wild monkeys were habituated for two weeks by daily placement of suitable food items around the trapping sites. Once sedation was achieved, phlebotomy was performed via cephalic or tibial venipuncture. Five millilitres (5 ml) of blood was collected, 1 ml into heparinized tubes; the remaining into sterile plain tubes for serum separation. Samples were transported on ice packs to the Centre for Control and Prevention of Zoonoses (CCPZ) laboratory at the University of Ibadan and stored at −20°C until shipped to the Biomedical Primate Research Centre (BPRC), Rijswijk, The Netherlands–for virological testing. Ethical approval for capture and sampling of the monkeys was obtained from the University of Ibadan, Animal Care and Use Research Ethics Committee (Ethical Approval reference: UI-ACUREC/App/2015/055).
Immobilization of animals at CERCOPAN was done by separating the animals in satellite or squeeze cages and injecting by hand. Darting equipment was not necessary since squeeze cages were available for use. Drugs used at CERCOPAN were detomidine or medetomidine at a dose of 0.05–0.1 mg/kg body of the subject mixed with ketamine at a dose of 5–10 mg/kg. The serum samples obtained were stored (−20°C) at the CERCOPAN Veterinary laboratory, Calabar, and sent to the BPRC within two months of collection.
2.2. Filovirus Antibody Testing
Virus antibody tests were carried out in the BSL-3 virus research laboratory of the Biomedical Primate Research Centre (BPRC), Rijswijk, The Netherlands. Indirect ELISA (i-ELISA) was performed as earlier described [17], but with recent modifications [18–23]. In summary, filovirus species-specific recombinant proteins and purified antigens from EBOV, SUDV, and RAVV were the antibody targets in the assay [19,20]. Antibodies to filovirus, if present in the NHP sera, bound the filovirus species-specific targets–which were subsequently detected with protein-G- and protein-A conjugated to an enzyme. Antibodies were indirectly identified when the substrate was added and a color change occurred. Protein-G/protein-A conjugate was used instead of the standard anti-NHP secondary antibody because anti-NHP conjugates are mainly produced for research purpose-bred animals like chimps, macaques, and baboons. In lower primates (like marmosets and tamarins) standard anti-NHP conjugate does not work 100% thereby creating false negative results.
2.2.1. Indirect ELISA
A species-specific, recombinant antigen-based, ELISA protocol was used to target antibodies to EBOV, SUDV or RAVV in NHP sera. This approach was different from the conventional whole virus-targeted ELISA with its characteristic cross-reactivity across Ebola viruses [21]. The i-ELISA was derived from a broad range of filovirus antigens exclusively used for coating ELISA plates.
The filovirus species-specific proteins used to coat the ELISA plates were:
- (i)
A mixture of “EBOV GP which was purified from Human Embryonic Kidney 293 cell culture and obtained from Immune Technology Corporation (catalogue number: IT-014-003p)” and “Ultra-centrifuged EBOV lysate (EBOV IgG lysate) which was inactivated by gamma irradiation, sucrose purified and extracted in an IgG column”–both targeted at antibodies to EBOV.
- (ii)
SUDV GP (type Gulu) which was purified from baculovirus-infected insect cells and obtained from Sino Biologicals Incorporated (catalogue number: 40094-V08BH2).
- (iii)
Ultra-centrifuged RAVV lysate (RAVV IgG lysate) which was inactivated by gamma irradiation, sucrose purified and extracted in an IgG column.
These coated plates were individually used to detect IgM and IgG antibodies specific to EBOV, SUDV, and RAVV virus glycoprotein respectively. In other words, antigens specific for the respective filoviruses were exclusively coated on ELISA plates, to bind species-specific antibodies, and without the likelihood of cross-reactivity.
The positive control sera used were:
- (i)
Anti-sera specific to EBOV GP from Immune Technology Corporation [Catalogue number: IT-014-003/Anti-GP (Ebola/Zaire)].
- (ii)
Anti-sera specific to SUDV GP1 (type Gulu) from Sino Biologicals Incorporated (Catalogue number: 40094-R301-100). Human EVD convalescent plasma (SUDV) was also used since plasma or serum has a wider range of antibodies than a monoclonal antibody.
- (iii)
Human Marburg virus disease convalescent plasma–UE vial anti-human Marburg virus (20/6/92).
The negative controls used were:
- (i)
Rabbit polyclonal antibody.
- (ii)
Heat-inactivated (30 mins at 56°C), pooled macaque serum from BPRC colony.
This emerging approach to filoviruses surveillance in West Africa is considered more effective and efficient for improving our knowledge of the epizootiology of those virus species and types circulating in such resource-limited environments.
Filovirus species-specific protein solution (1.0 mg virus/ml in Tris-NaC1-EDTA Buffer, and 0.25% Triton X-100), was added to each well of flat bottom polystyrene ELISA plates (675061, 96 well, Greiner Bio-One, Germany), at a concentration of 2 µg/ml in phosphate-buffered saline (PBS), and incubated overnight at room temperature (RT). The coated plates were washed (5×) with 0.01 M PBS, 0.1% Tween 20) and blocked for 1 h at RT with a mixture comprising 1.0% casein (SC5890, Sigma-Aldrich, St. Louis, MO, USA) in 0.01 M PBS. A further washing (5x) was done, followed by addition of 100 µl of each serum sample (in duplicates), previously heat inactivated for 30 min at 56°C and diluted 1:100 in PBS, 1% casein, 0.1% cell lysate of uninfected cells, and 0.1% Tween 20 to the wells followed by incubation for 1 h at 20°C. Wells were then washed (5×) and a conjugate solution comprising 1/1000 diluted protein G (539305, Calbiochem, San Diego, USA) and 1/1000 protein A (P7488 Sigma Aldrich Chemie NV, Zwijndrecht, The Netherlands) was added followed by incubation for 1 h at RT. Plates were washed again and the substrate, Blue Phosphatase substrate (50–88-05/-6, KPL, Gaithersburg MD, USA), was added to the wells (100 µl/well) for colour development. The reaction was stopped with 2 N NaOH, and the plates were read at 595 nm wavelength on a Bio-Rad model iMARK™ microplate absorbance reader (Bio-Rad Laboratories, The Netherlands).
Blank values were subtracted from all optical density (OD) values, by the pre-programmed microplate reader. OD values greater than 4 times the mean of the negative controls were considered positive while values less than 2 times the mean of the negative controls were considered negative. All values in-between were considered as equivocal responses. Further confirmatory tests such as plaque reduction neutralisation tests (PRNT) could not be done due to BSL4 requirements for such tests.
3. RESULTS
3.1. Natural Exposure of NHPs of Southern Nigeria to Filovirus
Among the 142 serum samples from individual animals belonging to 11 NHP species–subjected to serological testing–three (2.1%) showed a positive reaction to EBOV antigen (Table 2; Table 3; Fig. 2), while none reacted positively to the SUDV or RAVV antigens. The positive reactors were sera from three individual animals each belonging to the species Cercopithecus erythrotis, Cercopithecus nictitans, and Cercopithecus sclateri. Ambiguous reactions to EBOV antigens were found in sera from three individual animals, each belonging to the species Papio anubis, Cercopithecus mona, Cercopithecus sclateri; and three individual animals belonging to Cercocebus torquatus. The entire three positive, and five out of the six equivocal sera were among those obtained from monkeys confiscated from poachers by CERCOPAN and housed in the primate sanctuary in Calabar, SE Nigeria. Only the animal belonging to P. anubis was from south-west Nigeria.
| Genus | Species | Common name | No. testeda (No. positiveb) | No. from SWN | No. from SEN |
|---|---|---|---|---|---|
| Cercocebus | sabaeus | Green monkey | 15(0) | 15 | – |
| torquatus | Collared mangabey | 34(0) | 2 | 32 | |
| Cercopithecus | erythrotis | Red-eared guenon | 3(1) | – | 3 |
| mona | Mona monkey | 19(0) | 5 | 14 | |
| nictitans | Putty-nosed monkey | 24(1) | 1 | 23 | |
| preussi | Preuss’s monkey | 1(0) | – | 1 | |
| sclateri | Sclater’s guenon | 7(1) | – | 7 | |
| tantalus | Tantalus monkey | 14(0) | – | 14 | |
| Erythrocebus | patas | Patas monkey | 14(0) | 14 | – |
| Papio | anubis | Anubis/Olive baboon | 10(0) | 10 | – |
| Pan | troglodytes | Common chimpanzee | 1(0) | 1 | – |
| Total | 142(3) | 48 | 94 |
NHP, non-human primates; SWN, Southwest Nigeria; SEN, Southeast Nigeria.;
Number of different animals.;
All positive cases were from SEN.
Seroprevalence of Ebola virus antibodies in 11 species of non-human primates from southern Nigeria.
| Serum Id* | OD** | Results*** | Species |
|---|---|---|---|
| PC1 | 1.23 | +ve Control 1 | – |
| PC2 | 1.21 | +ve Control 2 | – |
| NC1 | 0.15 | −ve Control 1 | – |
| NC2 | 0.10 | −ve Control 2 | – |
| S01 | 0.00 | −ve | Cercocebus torquatus |
| S02 | −0.04 | −ve | Cercocebus torquatus |
| S03 | 0.20 | −ve | Cercocebus torquatus |
| S04 | 0.11 | −ve | Cercocebus torquatus |
| S05 | 0.00 | −ve | Cercocebus torquatus |
| S06 | 0.10 | −ve | Cercocebus torquatus |
| S07 | 0.08 | −ve | Cercocebus torquatus |
| S08 | 0.04 | −ve | Cercocebus torquatus |
| S09 | 0.21 | −ve | Cercocebus torquatus |
| S10 | 0.09 | −ve | Cercocebus torquatus |
| S11 | 0.13 | −ve | Cercocebus torquatus |
| S12 | 0.27 | Equivocal | Cercocebus torquatus |
| S13 | 0.11 | −ve | Cercocebus torquatus |
| S14 | 0.07 | −ve | Cercocebus torquatus |
| S15 | 0.18 | −ve | Cercocebus torquatus |
| S16 | 0.14 | −ve | Cercocebus torquatus |
| S17 | 0.07 | −ve | Cercocebus torquatus |
| S18 | 0.06 | −ve | Cercocebus torquatus |
| S19 | 0.20 | −ve | Cercocebus torquatus |
| S20 | 0.12 | −ve | Cercocebus torquatus |
| S21 | 0.14 | −ve | Cercocebus torquatus |
| S22 | 0.14 | −ve | Cercocebus torquatus |
| S23 | 0.11 | −ve | Cercocebus torquatus |
| S24 | 0.06 | −ve | Cercocebus torquatus |
| S25 | 0.16 | −ve | Cercocebus torquatus |
| S26 | 0.26 | Equivocal | Cercocebus torquatus |
| S27 | 0.06 | −ve | Cercocebus torquatus |
| S28 | 0.11 | −ve | Cercocebus torquatus |
| S29 | 0.20 | −ve | Cercocebus torquatus |
| S30 | 0.25 | Equivocal | Cercocebus torquatus |
| S31 | 0.06 | −ve | Cercocebus torquatus |
| S32 | 0.18 | −ve | Cercocebus torquatus |
| S33 | 0.22 | −ve | Cercocebus torquatus |
| S34 | 0.05 | −ve | Cercocebus torquatus |
| S35 | 0.02 | −ve | Cercopithecu preussi |
| S36 | 0.50 | +ve | Cercopithecus erythrotis |
| S37 | 0.04 | −ve | Cercopithecus erythrotis |
| S38 | 0.08 | −ve | Cercopithecus erythrotis |
| S39 | 0.20 | −ve | Cercopithecus mona |
| S40 | 0.28 | Equivocal | Cercopithecus mona |
| S41 | 0.04 | −ve | Cercopithecus mona |
| S42 | 0.02 | −ve | Cercopithecus mona |
| S43 | 0.11 | −ve | Cercopithecus mona |
| S44 | 0.23 | −ve | Cercopithecus mona |
| S45 | 0.19 | −ve | Cercopithecus mona |
| S46 | 0.18 | −ve | Cercopithecus mona |
| S47 | 0.08 | −ve | Cercopithecus mona |
| S48 | 0.15 | −ve | Cercopithecus mona |
| S49 | 0.09 | −ve | Cercopithecus mona |
| S50 | 0.21 | −ve | Cercopithecus mona |
| S51 | 0.02 | −ve | Cercopithecus mona |
| S52 | −0.04 | −ve | Cercopithecus mona |
| S53 | −0.06 | −ve | Cercopithecus mona |
| S54 | −0.06 | −ve | Cercopithecus mona |
| S55 | 0.07 | −ve | Cercopithecus mona |
| S56 | 0.09 | −ve | Cercopithecus mona |
| S57 | −0.04 | −ve | Cercopithecus mona |
| S58 | −0.05 | −ve | Cercopithecus nictitans |
| S59 | 0.10 | −ve | Cercopithecus nictitans |
| S60 | 0.20 | −ve | Cercopithecus nictitans |
| S61 | 0.60 | +ve | Cercopithecus nictitans |
| S62 | 0.05 | −ve | Cercopithecus nictitans |
| S63 | 0.02 | −ve | Cercopithecus nictitans |
| S64 | 0.04 | −ve | Cercopithecus nictitans |
| S65 | 0.03 | −ve | Cercopithecus nictitans |
| S66 | 0.13 | −ve | Cercopithecus nictitans |
| S67 | 0.08 | −ve | Cercopithecus nictitans |
| S68 | 0.00 | −ve | Cercopithecus nictitans |
| S69 | −0.01 | −ve | Cercopithecus nictitans |
| S70 | 0.02 | −ve | Cercopithecus nictitans |
| S71 | 0.05 | −ve | Cercopithecus nictitans |
| S72 | 0.04 | −ve | Cercopithecus nictitans |
| S73 | 0.05 | −ve | Cercopithecus nictitans |
| S74 | 0.02 | −ve | Cercopithecus nictitans |
| S75 | 0.08 | −ve | Cercopithecus nictitans |
| S76 | 0.18 | −ve | Cercopithecus nictitans |
| S77 | 0.01 | −ve | Cercopithecus nictitans |
| S78 | 0.11 | −ve | Cercopithecus nictitans |
| S79 | 0.04 | −ve | Cercopithecus nictitans |
| S80 | 0.00 | −ve | Cercopithecus nictitans |
| S81 | −0.01 | −ve | Cercopithecus nictitans |
| S82 | 0.00 | −ve | Cercopithecus sclateri |
| S83 | 0.19 | −ve | Cercopithecus sclateri |
| S84 | 0.29 | Equivocal | Cercopithecus sclateri |
| S85 | 0.11 | −ve | Cercopithecus sclateri |
| S86 | 0.15 | −ve | Cercopithecus sclateri |
| S87 | 0.52 | +ve | Cercopithecus sclateri |
| S88 | 0.12 | −ve | Cercopithecus sclateri |
| S89 | 0.08 | −ve | Cercopithecus tantalus |
| S90 | 0.19 | −ve | Cercopithecus tantalus |
| S91 | 0.16 | −ve | Cercopithecus tantalus |
| S92 | 0.06 | −ve | Cercopithecus tantalus |
| S93 | 0.17 | −ve | Cercopithecus tantalus |
| S94 | 0.02 | −ve | Cercopithecus tantalus |
| S95 | 0.12 | −ve | Cercopithecus tantalus |
| S96 | 0.03 | −ve | Chlorocebus sebaeus |
| S97 | −0.01 | −ve | Chlorocebus sebaeus |
| S98 | −0.01 | −ve | Chlorocebus sebaeus |
| S99 | −0.03 | −ve | Chlorocebus sebaeus |
| S100 | −0.05 | −ve | Chlorocebus sebaeus |
| S101 | −0.05 | −ve | Chlorocebus sebaeus |
| S102 | −0.04 | −ve | Chlorocebus sebaeus |
| S103 | −0.06 | −ve | Chlorocebus sebaeus |
| S104 | −0.04 | −ve | Chlorocebus sebaeus |
| S105 | −0.02 | −ve | Chlorocebus sebaeus |
| S106 | −0.05 | −ve | Chlorocebus sebaeus |
| S107 | −0.06 | −ve | Chlorocebus sebaeus |
| S108 | −0.04 | −ve | Chlorocebus sebaeus |
| S109 | −0.03 | −ve | Chlorocebus sebaeus |
| S110 | −0.09 | −ve | Chlorocebus sebaeus |
| S111 | 0.02 | −ve | Erythrocebus patas |
| S112 | −0.01 | −ve | Erythrocebus patas |
| S113 | −0.03 | −ve | Erythrocebus patas |
| S114 | −0.06 | −ve | Erythrocebus patas |
| S115 | −0.02 | −ve | Erythrocebus patas |
| S116 | −0.06 | −ve | Erythrocebus patas |
| S117 | −0.07 | −ve | Erythrocebus patas |
| S118 | −0.06 | −ve | Erythrocebus patas |
| S119 | −0.02 | −ve | Erythrocebus patas |
| S120 | −0.01 | −ve | Erythrocebus patas |
| S121 | −0.05 | −ve | Erythrocebus patas |
| S122 | −0.04 | −ve | Erythrocebus patas |
| S123 | −0.05 | −ve | Erythrocebus patas |
| S124 | −0.01 | −ve | Erythrocebus patas |
| S125 | −0.03 | −ve | Pan troglodytes |
| S126 | −0.03 | −ve | Papio anubis |
| S127 | −0.05 | −ve | Papio anubis |
| S128 | −0.05 | −ve | Papio anubis |
| S129 | −0.05 | −ve | Papio anubis |
| S130 | −0.05 | −ve | Papio anubis |
| S131 | −0.04 | −ve | Papio anubis |
| S132 | 0.25 | Equivocal | Papio anubis |
| S133 | −0.04 | −ve | Papio anubis |
| S134 | −0.05 | −ve | Papio anubis |
| S135 | 0.05 | −ve | Papio anubis |
| S136 | 0.01 | −ve | Cercopithecus tantalus |
| S137 | 0.01 | −ve | Cercopithecus tantalus |
| S138 | −0.01 | −ve | Cercopithecus tantalus |
| S139 | 0.05 | −ve | Cercopithecus tantalus |
| S140 | 0.03 | −ve | Cercopithecus tantalus |
| S141 | 0.07 | −ve | Cercopithecus tantalus |
| S142 | −0.01 | −ve | Cercopithecus tantalus |
PC1 & PC2 are positive controls; NC1 & NC2 are negative controls; S01-S142 are non-human primate serum samples;
OD values presented are mean values of readings obtained from duplicate tests on each sample; Blank values were subtracted by the pre-programmed microplate reader from all OD values;
OD values greater than 4 times the mean of the negative controls were considered positive; values less than 2 times the mean of the negative controls were considered negative; all values in-between were considered equivocal.
Interpretation of OD values of i-ELISA targeted at EBOV antibodies in non-human primate serum samples from southern Nigeria.
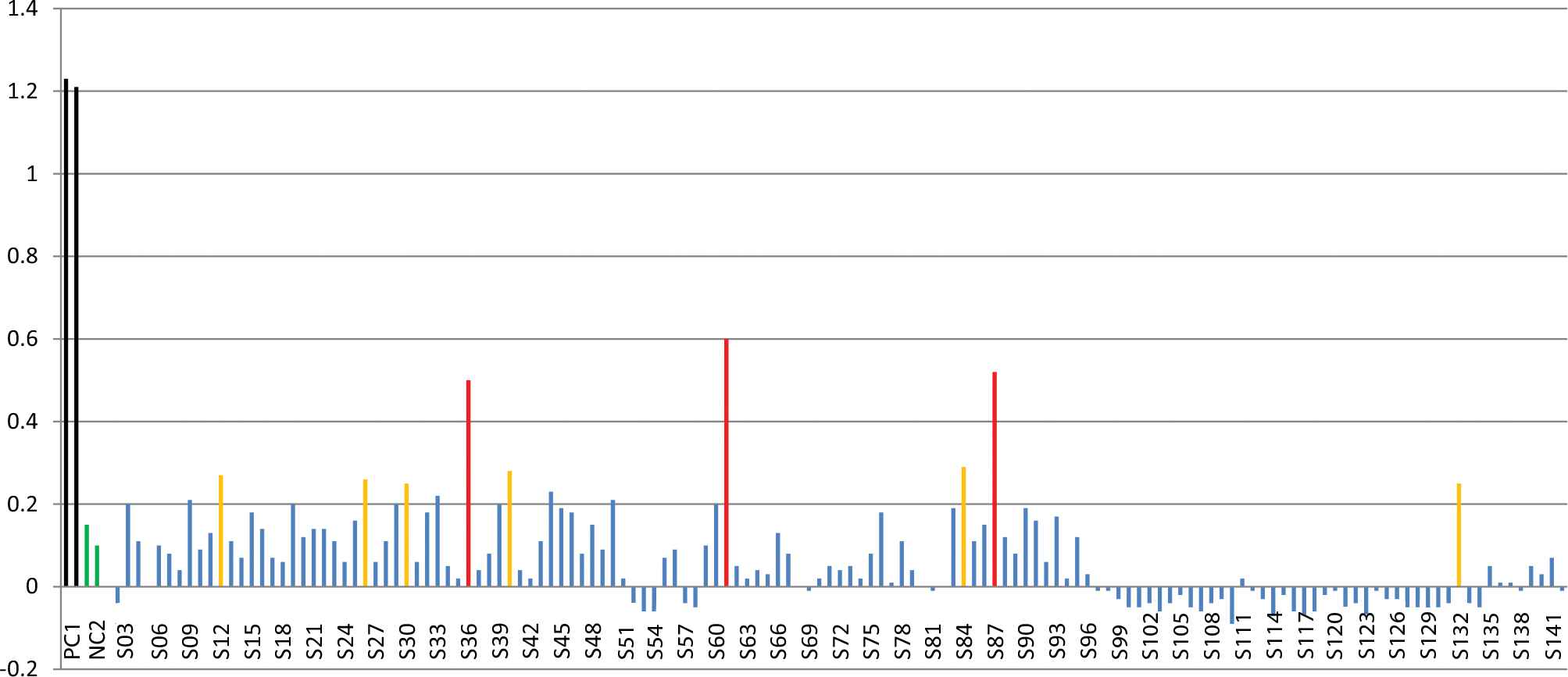
Graphical representation of OD values of i-ELISA designed to detect EBOV antigens in monkey serum samples from southern Nigeria. This figure displays the optical density values for 142 monkey serum samples (including the controls) as vertical bars. The positive and negative controls are represented with black and green bars respectively while positive, negative and equivocal results are represented with red, blue and orange bars respectively.
4. DISCUSSION
The present investigation was carried out in view of the 2013–2015 EVD epidemic in West Africa and its continuous public health implications in the sub-region. We determined exposure status of NHPs to three major filoviruses on selected locations in southern Nigeria. The exposure status of animals belonging to 11 native species of NHP to EBOV, SUDV, and RAVV was investigated at five locations in the rainforests of south-western and south-eastern parts of Nigeria that have touristic and recreational uses, or that are important to NHP conservation. The findings suggest natural exposure of native NHPs in southern Nigeria to EBOV, but not to SUDV or RAVV.
To the best of our knowledge, this study is the first to document serological findings suggestive of filovirus exposures in animal samples from Nigeria. The presence of EBOV antibodies in native monkeys could mean that the virus was present in the Nigerian wildlife before the recent EVD outbreaks 2014 in humans in Nigeria; the source of which was a human index case imported into Lagos metropolis in the south-western part of Nigeria from Monrovia, the capital of Liberia [9]. Cross River State, where positive cases (including five out of the six equivocal results) in monkeys were recorded in this study, has a contiguous international boundary with Cameroon where EBOV has been serologically detected in Chimpanzees [13]. In fact, the expansive Cross River National Park shares a long border with Takamanda forest reserve and Korup National park both in Cameroon [24]. The observation that the entire positive sera were among those obtained from monkeys confiscated from poachers by CERCOPAN corroborate with the circulation of EBOV in Cameroon (which is adjacent to Calabar, Cross River State) with the possibility of natural spill-over into Cross River NHP populations. Therefore, the eastern region of Nigeria should be a choice region for any future extensive study of EBOV transmission dynamics in Nigerian and in West African wildlife.
The fact that IgM antibodies may take 2–6 days to develop in the body fluids of an exposed animal or human and IgG antibodies may remain for some 3–10 years once developed [18,19] implies every likelihood that the NHPs could have been exposed to the virus over a very broad time range. In their study, Tomori and others [11] reported seropositivity Ebola virus and marburgviruses in northern Nigeria and not in the rainforest zone located in the south of the country where we have found the present positive cases. It is therefore of interest to expand our sero-survey of NHP to the human population living in south-eastern Nigeria, the living area of the EBOV-exposed NHPs, with special attention to occupationally exposed individuals and residents in neighbouring communities.
In addition, since bats are presumed reservoirs of EBOV as well as other potentially fatal viral zoonotic pathogens [15], the present EBOV exposures detected in monkeys in southern Nigeria may possibly have resulted from a spill-over of the infection from bats found in the area. Sero-epizootiological and molecular investigation of bats in the region for filovirus infection would give additional information towards a better understanding of the potential source of the virus exposure in the monkeys. Uncontrolled ‘bushmeat’ hunting and close interaction between humans and NHP have been going on in the region. This poses an avenue of exposure of humans to potentially highly pathogenic microbes from wildlife [25–27].
The relatively few sampled animals may not fully represent the extent of exposure of monkeys in the region to Filoviruses. Detailed sensitivity and specificity tests (such as Virus Neutralisation and plaque reduction neutralisation assays) were not performed in this study, neither was the detection limit of the assay i-ELISA determined. However, the use of recombinant proteins instead of whole viruses to coat the ELISA plates reduced the possibility of cross-reactivity between the viruses [21]. Also, an ‘in-house quality control’ repeated tests (with same ELISA protocol) on the positive samples and some of the negative samples also gave results similar to those previously obtained in the tests (as presented the Fig. 2)–the likelihood of false positives was therefore minimal. Therefore, this report may serve as a template for future strategic and more systematic surveillance of EBOV in wildlife animals in southern Nigeria. Standardisation of anti-EBOV antibody detection ELISA protocol for routine use in NHPs–such as recently done for pigs [23]–is highly recommended. We also recommend proactive studies and surveillance for a better understanding of the geographical range and drivers of EBOV exposure and risk of public health events in the tropical rainforests of West Africa. A follow-up RT-PCR analysis of positive samples would be critical to ascertain active infection status or not in the monkeys at the time of our investigation. In particular, a more systematic and longitudinal survey of NHPs and bat viral pathogen load, on a national scale, is advisable. At the same time, it is essential to intensify action against the uncontrolled hunting of monkeys in Nigeria.
Sero-surveillance–the screening for pathogen-associated antigens or antibodies in serum samples from a population in this way–has been described as a useful tool for rapid investigation of viral pathogens circulating in resource-limited environments [18,28]. The presence of species-specific antibodies to EBOV in NHPs in Nigeria is of public health importance, and a pointer to an expanding area of endemicity (enzooticity), similar to what may be implied from the reported finding of antibodies to the virus in humans and NHP sera from Ebola hot spots, as well as in regions that had never recorded either human or animal EVD cases [13,29]. Although such reports have triggered debates on the actual geographical range of the viruses and led to questions of methods used to carry out surveillance for the disease [12,30], ours and similar findings should be considered as a basis for early warning and preparedness on a logical framework for response at the source. For example, based on the list of WHO-approved effective EVD vaccines following 2013–2015 epidemics and the high virulence of the virus, the pre-exposure vaccination of occupationally exposed individuals, including employees of research institutes such as the CERCOPAN primate sanctuary would be a logical public health policy in West Africa.
5. CONCLUSION
This study provides serological evidence of probable exposure of NHPs to natural infection with EBOV in the conserved rainforests of southern Nigeria as revealed by filovirus species-specific ELISA results. While this is of public health importance and is the first reported evidence of naturally-occurring EBOV infections in NHPs in Nigeria, the potential role of these animals in the ecology and epizootiology of filoviruses in Nigeria needs further investigation. Until the true prevalence of EBOV infection among the monkeys in Nigeria is conclusively verified, there is a critical need to discourage the uncontrolled hunting of monkeys in the country, not only for conservation of NHPs but also to safeguard public health.
CONFLICT OF INTEREST
None.
REFERENCES
Cite this article
TY - JOUR AU - B.N. Ogunro AU - B.O. Olugasa AU - E.J. Verschoor AU - A.O. Olarinmoye AU - I. Theyse AU - H. Niphuis PY - 2018 DA - 2018/12/31 TI - Serological Detection of Ebola Virus Exposures in Native Non-human Primates of Southern Nigeria JO - Journal of Epidemiology and Global Health SP - 162 EP - 170 VL - 8 IS - 3-4 SN - 2210-6014 UR - https://doi.org/10.2991/j.jegh.2018.05.001 DO - 10.2991/j.jegh.2018.05.001 ID - Ogunro2018 ER -
