Unusually High Global End Diastolic Index Associated with Optimal Cardiac Index in Two Critically Ill Patients
- DOI
- 10.2991/icres.k.210406.002How to use a DOI?
- Keywords
- Cardiopulmonary physiological disorders; hemodynamic monitoring; pulse indicator continuous cardiac output (PiCCO); global end diastolic index (GEDI)
- Abstract
The optimal management of hemodynamic disorders among critically ill patients requires an accurate assessment of hemodynamic status. Global End Diastolic Index (GEDI) is taken for a more reliable indicator of preload in critically ill patients than central venous pressure and doctors tend to arrange it among the normal ranges (680–800 ml/m2). Here we report a case with a relatively extremely high GEDI that initially erroneously led to a fluid restrictive treatment. An 83-year-old man was admitted to the intensive care unit (ICU) for dyspnea and severe hypoxemia following inefficient antibiotics treatment of bilateral pneumonia in emergency room. Failed with non-invasive positive pressure ventilation (NPPV), he was intubated and Pulse Indicator Continuous Cardiac Output (PiCCO) system was installed. Result shows extremely high GEDI 1620 ml/m2, therefore continuous renal replacement therapy was initiated for negative fluid balance. When GEDI was reduced below 1300 ml/m2, cardiac index (CI) decreased simultaneously. According to the Frank–Starling curve, GEDI of 1300 ml/m2 was seemed as being associated with a maximal CI for the patient. Next chest roentgenogram and abdomen computer tomography (CT) scan showed three aneurysms which were responsible for the extremely high GEDI values due to special calculated methods in Newman model of the PiCCO principle. In such cases, ventricular function curve will be useful and recommended to assess the individually most appropriate GEDI.
- Chinese Abstract
危重患者血流动力学紊乱的精准管理需要对血流动力学状态进行精确评估。与中心静脉压相比,全心舒张末期容积指数(Global End Diastolic Index,GEDI)被认为是评估危重患者前负荷更可靠的指标,临床医生常将其正常范围设为680-800 ml/m2。本文报道一例GEDI极高,并在初始治疗进行了错误地限制性液体治疗的病例。该病例是一位83岁老年男性,因双肺肺炎在急诊室进行抗生素治疗无效,后因呼吸困难、低氧血症收入ICU。给与无创正压通气(NPPV)治疗失败后,改为有创机械通气,并通过PiCCO系统监测血流动力学状态。PiCCO监测结果显示GEDI非常高,为1620 ml/m2,因此给予CRRT治疗,纠正液体负平衡。当GEDI低于1300 ml/m2时,同时伴有心脏指数(cardiac index,CI)的降低。根据Frank-Starling曲线,GEDI为1300 ml/m2时CI最大。胸部x线片和腹部CT结果显示机体存在3个动脉瘤,这是导致GEDI值极高的原因,该值是PiCCO系统基于Newman模型的计算方法,在这种情况下,建议采用心室功能曲线获得准确的GEDI值。
- Copyright
- © 2021 First Affiliated Hospital of Zhengzhou University. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
The optimal management of critically ill patients with cardiopulmonary disorders requires an accurate assessment of hemodynamic status. As an advanced technique of hemodynamic monitoring, the Pulse Indicator Continuous Cardiac Output (PiCCO) system offers accurate assessments of hemodynamic status constantly and dynamically, provides aid in the determination of immediate and subsequent therapies and correlates well with pulmonary arterial catheter [1–4]. In particularly, Global End Diastolic Index (GEDI), a volumetric parameter, is a more reliable indicator of preload in critically ill patients than the filling pressure of Central Venous Pressure (CVP) [5,6]. However, clinicians may be prone to treat patients according to absolute values of GEDI, i.e., to set targets to the normal range of 680–800 ml/m2. Here we report two patients with unusually high GEDI that misled to fluid restrictive treatments initially. This case is indicative that treatment should not only based on PiCCO parameters; comprehensive medical condition should be considered on managing hemodynamic status.
An 85-year-old female with preexisting atrial fibrillation and pulmonary fibrosis was transferred to the ICU for an episode of acute lung edema induced by heavy exercise. On ICU admission, she was intubated, and mechanical ventilation was initiated with a Positive End Expiratory Pressure (PEEP) of 5 cm H2O. A double-lumen central venous catheter was inserted into the right internal jugular vein, and a CVP of 18 mmHg was identified. A 5-Fr thermistor-tipped catheter (Pulsiocath PV2015L20, PiCCO plus, Pulsion Medical Systems, Munich, Germany) was placed into the femoral artery for extended hemodynamic monitoring. For the first set measurements, GEDI was 1120 ml/m2, and Extravascular Lung Water Index (ELWI) was 16 ml/kg (normal range: 3–7 ml/kg), in addition, the patient had edema in both lower extremities and was ausculted as wet rales in both lower lungs. After negative fluid balance using furosemide for the first 2 days, GEDI decreased to 950 ml/m2 with CI unchanged and PaO2/FiO2 ratio (P/F) improved meanwhile. However, continued diuresis not only decreased GEDI to 850 ml/m2, but also decreased CI from 3.4 to 2.6 L/min/m2. Norepinephrine was then pumped (0.2 µg/kg/min) to maintain Mean Arterial Pressure (MAP) above 70 mmHg. Transthoracic echocardiography (TTE) revealed a normal left ventricular systolic function with an ejection fraction 60% and a huge right atrium (72 × 54 mm), a huge right ventricle (40 mm) and an enlarged left atrium (50 × 75mm), as showed in Figure 1. The TTE also revealed severe mitral and tricuspid regurgitation with an estimated pulmonary arterial systolic pressure of 64 mmHg. Since passive leg raising test showed fluid responsiveness, 1000 ml Sodium Lactate infusions increased GEDI to 950 ml/m2, with CI increased and norepinephrine withdrawn. GEDI of about 950 ml/m2 was considered being associated with an optional CI. She was given a large dose of alprostadil, and finally extubated successfully on day 5. Figure 2 showed a modified Frank–Starling curve from GEDI and CI values over four consecutive days with unchanged airway pressures (In the first 2 days, we increased PEEP to treat pulmonary edema, on the 3rd day, with the decline in patient’s blood pressure and CI, we consider that excessive use of diuretics lead to hypovolemia, so in the next time, we did not change PEEP).
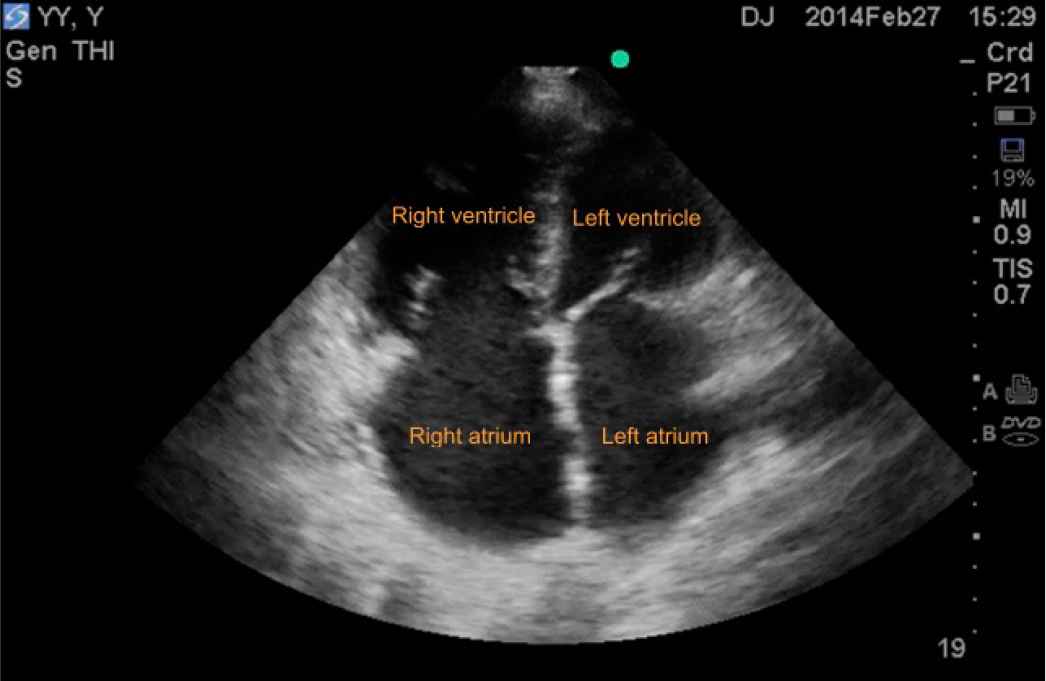
TTE showed enlarged right atrium, right ventricle and left atrium.
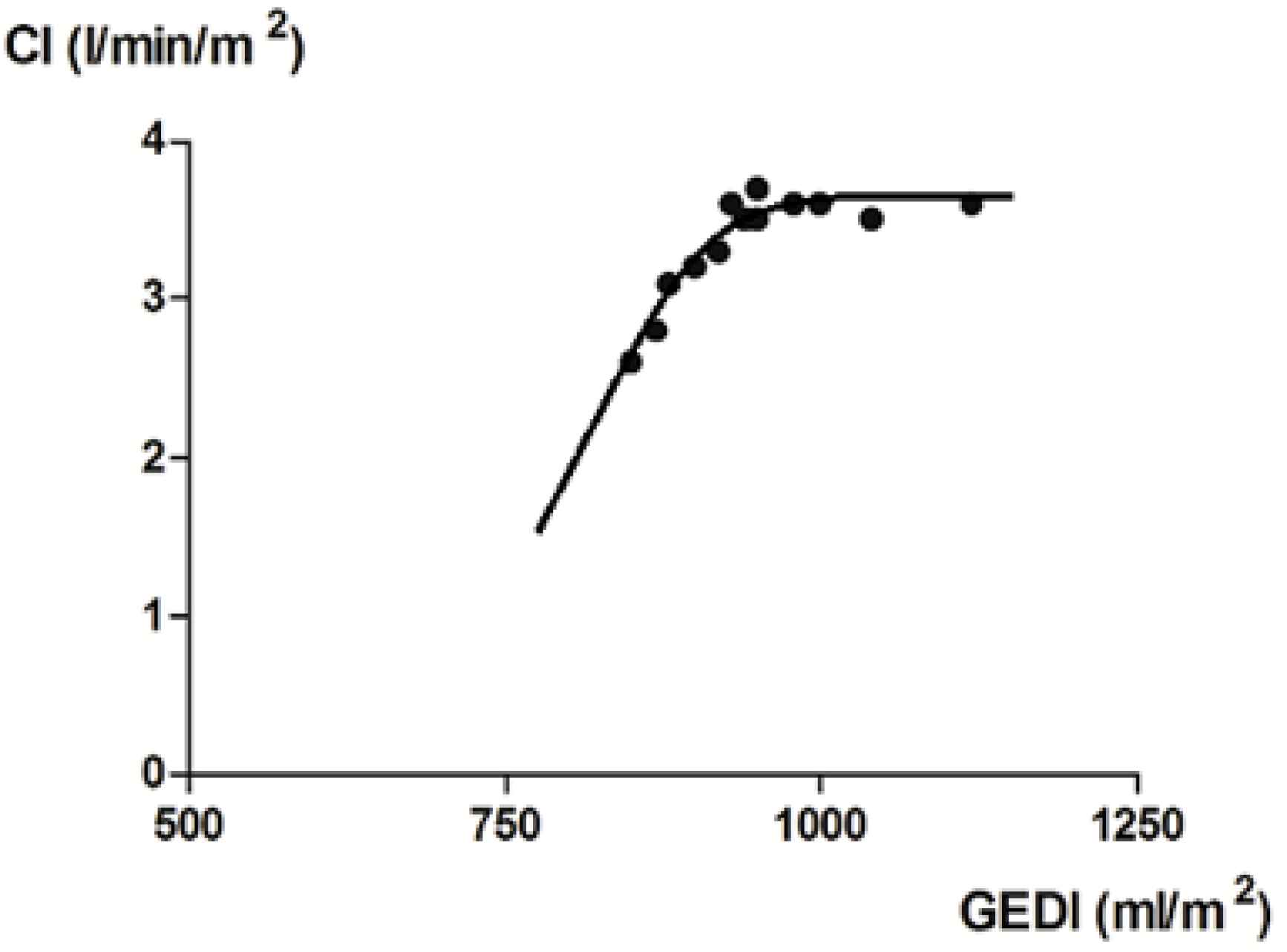
Relationship between GEDI and CI as constructed from values over four consecutive days with unchanged airway pressures.
A 83-year-old man with history of hypertension, coronary heart disease, and chronic renal insufficiency was admitted to the ICU for dyspnea and hypoxemia following a 4-day antibiotics for bilateral pneumonia in the emergency room. A central venous catheter was placed, imipenem was given and non-invasive positive pressure ventilation was initiated, which failed 1 h later and was substituted by invasive ventilation (FiO2 80%, PEEP 10 cm H2O). Because of hypotension (MAP 90 mmHg maintained with norepinephrine 0.4 µg/kg/min), high CVP (15 mmHg) and a level of brain natriuretic peptide of 4650 pg/ml (normal range: 0–100 pg/ml), advanced hemodynamic monitoring with the PiCCO system was installed. The first set of measurements (mean of three) were as follows: CI 2.4 L/min/m2, GEDI 1620 ml/m2, ELWI 16 ml/kg. Fluid overload and heart failure were presumed, so the inotropic support of dobutamine (5 µg/kg/min) was pumped and patient was treated with fluid restriction and Continuous Renal Replacement Therapy (CRRT) for negative balance. After a negative fluid balance of 4500 ml in 2 days, his blood pressure was stabilized with norepinephrine dosage decreased to 0.1 µg/kg/min. Another set of measurements showed extremely high GEDI 1310 ml/m2, CRRT was continued with a negative fluid balance of 2000 ml, which not only decreased GEDI to 1100 ml/m2, but also decreased of CI from 3 to 2.2 L/min/m2 with the dosage of norepinephrine increased to 0.4 µg/kg/min. Ultrasonography revealed three aneurysms (thoracic aortic aneurysm, 50 × 50 mm; abdominal aortic aneurysm, 40 × 50 mm; Iliac aneurysm 20 × 30 mm), which were confirmed by chest roentgenogram (Figure 3) and abdomen CT scan. Fluid was given to keep the GEDI of 1300 ml/m2, which was considered being associated with an optimal CI (Figure 4). About 24 h later, the patient was hemodynamic stable with dobutamine and norepinephrine stopped and oxygenation significantly improved. Extubation was on the schedule. Unfortunately, he suffered and died from catheter-related blood stream infection of Staphylococcus aureus.
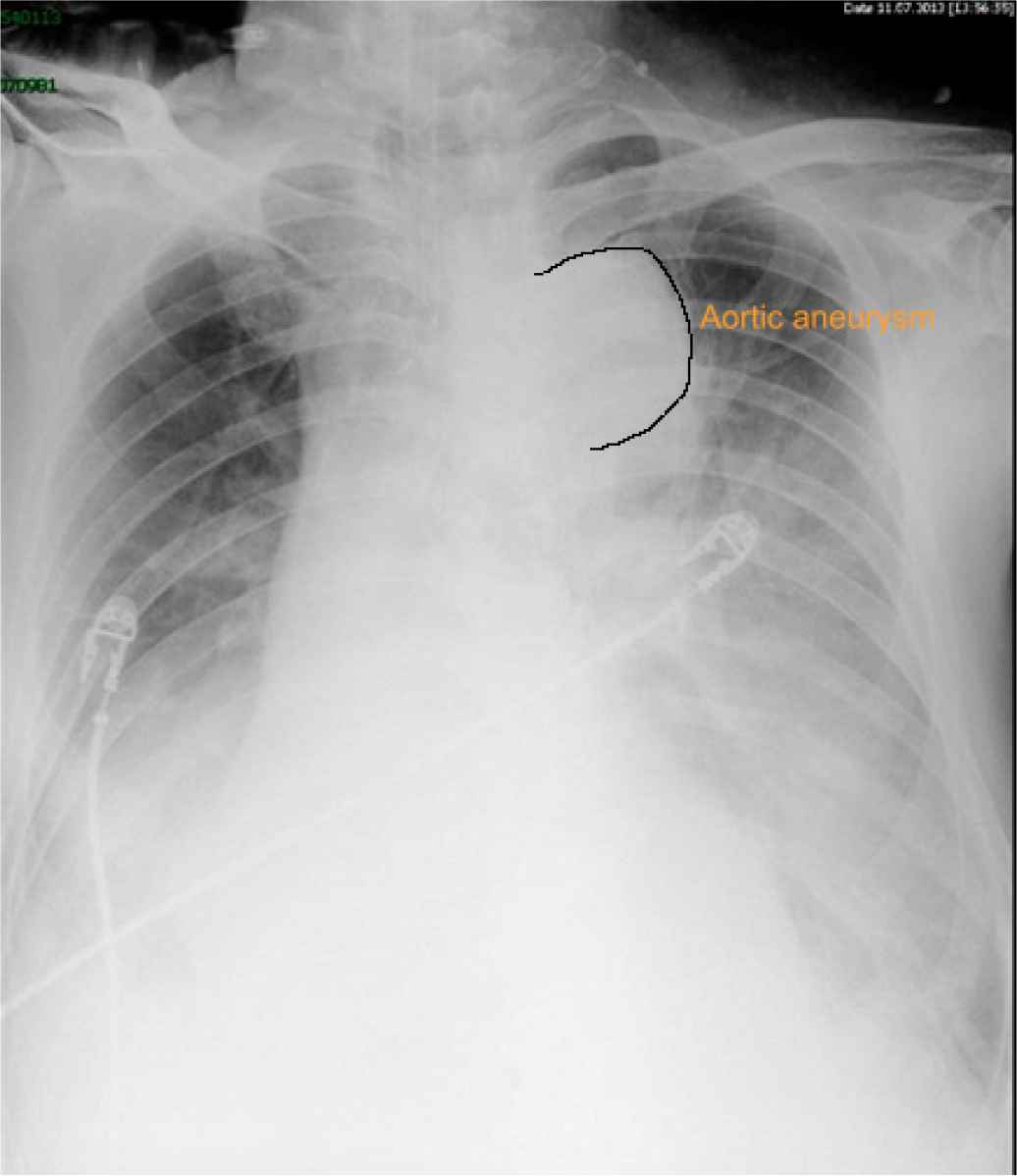
Chest roentgenogram showed thoracic aortic aneurysm (50 × 50 mm).
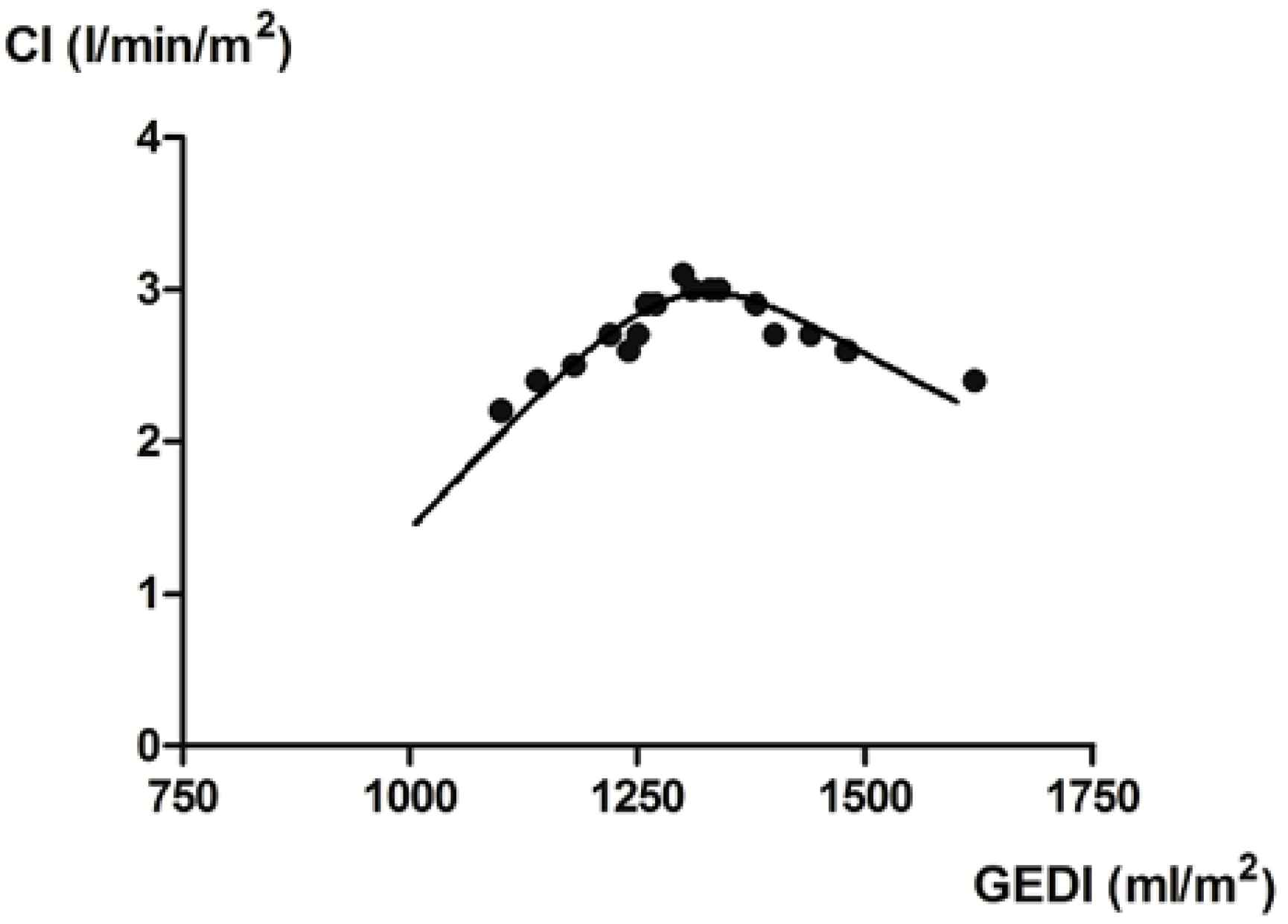
Relationship between GEDI and CI as constructed from values over four consecutive days with unchanged dobutamine dosage.
In recent years, reference values for GEDI were proposed and the notion of a fixed reference range applicable to all subjects was challenged [7–9]. Huber et al. [10] found that injection of saline into a femoral vena cava instead of a jugular or subclavian access results in higher GEDI values. A meta-analysis including 64 studies recognized significantly higher mean GEDI in septic patients compared with patients undergoing major surgeries, and concluded the need to adapt therapeutic targets for different patient populations [7].
Of note, with PiCCO, GEDI positively correlates with Intra-Thoracic Blood Volume (ITBV). Any factor causing increased ITBV will lead to increased GEDI. In our two patients with unusually high GEDI to maintain proper CI, one had huge cardiac chambers and the other had three large aortic aneurysms, including one thoracic aneurysm. These persisting anatomically changes are the reasons why they have optimal GEDI higher than their counterparts without those changes do. Another aspect worth noting is that since cold saline was injected into the central vein and blood temperature was detected by PiCCO catheter placed in the femoral artery in our patients, the abdominal aortic aneurysm and iliac aneurysm in the second patient should also had an impact on the GEDI. Akohov et al. [11] noticed that a larger aortic volume directly translates to a higher global end diastolic volume measurement. Therefore, instead of blindly targeting at the reference range for regular patients, GEDI should be titrated based on the Frank–Starling curve, especially for patients with an enlarged heart or a large aneurysm.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
Xiaoqing Wu prepared (review & editing) the manuscript. Desheng Chen and Chen Li collected the data and modified the manuscript. Jun Duan supervised the project.
REFERENCES
Cite this article
TY - JOUR AU - Xiaoqing Wu AU - Desheng Chen AU - Chen Li AU - Jun Duan PY - 2021 DA - 2021/04/10 TI - Unusually High Global End Diastolic Index Associated with Optimal Cardiac Index in Two Critically Ill Patients JO - Intensive Care Research SP - 31 EP - 33 VL - 1 IS - 1-2 SN - 2666-9862 UR - https://doi.org/10.2991/icres.k.210406.002 DO - 10.2991/icres.k.210406.002 ID - Wu2021 ER -
