Quality Improvement Project to Reduce Unnecessary Chest X-ray in a Tertiary Center
 , Reham Babiker, Abdelmoneim Mahgoub
, Reham Babiker, Abdelmoneim Mahgoub- DOI
- 10.2991/dsahmj.k.200702.001How to use a DOI?
- Keywords
- Acute bronchiolitis; pediatric; chest x-ray; radiography; consistent
- Abstract
The proper diagnostic approach for acute bronchiolitis is one of the significant controversial aspects among clinicians in the pediatric field. The radiographic evaluation of the classic presentation has a limited role and may expose patients to unnecessary procedures. Despite the presence of evidence-based guidelines, unnecessary radiography is still well documented worldwide. Therefore, our aim was primarily to evaluate the frequency of chest x-ray abnormalities in acute bronchiolitis and under what circumstances changes are accurately expected. The secondary aim was to decrease the use of unnecessary chest x-rays in acute bronchiolitis. For this, a retrospective study was conducted on 150 patients who were younger than 2 years of age and admitted for acute bronchiolitis. Patients with underlying comorbidities were excluded from the study. The results showed nonspecific alternation of chest radiography consistent with the disease behavior in 83.3% of the cases. There was no significant correlation between the clinical variables and the severity of radiological findings in our study. The study demonstrated that 59.3% of chest x-rays were not indicated and the majority of the overall requests were for high-grade fever. We conclude that there is no proven value of routine radiography in the usual presentation. In agreement with previous research, we recommend that requests should be made for particular indications as per existing guidelines. Ongoing education and re-auditing of practice continue to expand this body of evidence.
- Copyright
- © 2020 Dr. Sulaiman Al Habib Medical Group. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Acute bronchiolitis is one of the most common respiratory diseases encountered in pediatric clinical practice [1]. Worldwide, it accounts for 2–3% of infant hospitalizations per year, which represent a significant burden for the healthcare system [2]. Viruses are the leading causative organism, in particular, the Respiratory Syncytial Virus (RSV) [3]. Lower respiratory tract bronchioles are the principal affected cells with consequent inflammation, excessive secretions, and mucosal edema. The clinical presentations range from a mild self-limited illness to severely troubled breathing requiring medical care [4].
The increasing use of imaging has become a significant problem on the basis of the cost and unnecessary radiation [5]. Avoidance of possible complications or missing pneumonia is the main reason behind indiscriminate radiography. The routine usage of chest imaging may expose patients to unnecessary treatment such as antibiotic administration or prolonged hospital stay [6].
Several studies demonstrated that the majority of chest radiographies are relatively nonspecific with a variable degree of findings that are consistent with the disease presentation including bilateral infiltration, hyperinflation, or peribronchial cuffing [7]. To the extent of our knowledge, no studies have determined the proportion of abnormal chest x-rays in children admitted with acute bronchiolitis in Saudi Arabia. Besides, few studies in the literature have reported the risk factors of abnormal radiography [8,9]. Determining the frequency of pathological chest radiography and understanding the risk factors could help clinicians to reduce the number of chest x-rays, and thus limit unnecessary radiation [10].
Therefore, the primary goal of this study was to determine the proportion of significant chest x-rays abnormalities and to define the clinical predictors of these abnormalities in young children admitted with an acute bronchiolitis to a pediatric unit at a tertiary hospital. Secondary outcomes included a decrease in the use of unnecessary chest x-rays in acute bronchiolitis.
2. MATERIALS AND METHODS
The study was conducted in the pediatric department at Arryan Hospital/Dr. Sulaiman Al-Habib Medical Group (HMG; Riyadh, Saudi Arabia). HMG is a private tertiary center, Joint Commission International-accredited hospital. The study was approved by the HMG Institutional Review Board (Approval No: RC19.02.28).
This is a retrospective study that aims to evaluate the frequency of the chest x-ray abnormalities in acute bronchiolitis besides defining the possible predicting factors. A decrease in the use of unnecessary chest x-rays is the secondary aim of this research. The inclusion criteria were both genders up to 24 months and those admitted through the emergency department with the diagnosis of acute bronchiolitis. The diagnosis is a decision based on the clinical presentation of the patients, which includes coryza symptoms, cough, low-grade fever, and shortness of breath [11]. Our exclusion criteria were children older than 2 years, those with recurrent wheezy chest, children with signs and symptoms of pneumonia, premature babies, and those with comorbidities such as chronic lung disease or congenital heart disease.
The chest x-rays were performed in the anterior–posterior view. Data were collected from an electronic hospital record system called VIDA (volunteers for intercultural and definitive adventures) and categorized on Microsoft Office Excel sheet 2010 (Microsoft Corporation, Redmond, WA, USA). The parameters include the age, sex, and the predictors/factors of chest x-ray abnormalities, which include temperature, respiratory rate, oxygen saturation, C-reactive Proteins (CRP), neutrophil counts, nasopharyngeal RSV aspirate, and Pediatric Intensive Care Unit (PICU) admission.
The results of chest x-rays were divided according to the interpretation of the radiologist into two groups: group I consistent with acute bronchiolitis and group II inconsistent with acute bronchiolitis. Statistical analysis was performed using SPSS version 19 (SPSS Inc., Chicago, IL, USA). Data are presented as descriptive statistics (mean ± standard deviation for continuous data, n [%] for categorical data). Student t-test and Chi-square test were performed for the comparison of continuous and categorical data, respectively. Multivariate logistic regression analysis was incorporated to predict the risk factors for chest x-rays abnormalities. Statistical significance was measured with p < 0.05.
Finally, to decrease the use of unnecessary chest x-rays, the indication of imaging was retrieved from patient’s records and compared to the American Academy of Pediatrics (AAP) and National Institute of Health and Care Excellence (NICE) recommendations, which include signs of respiratory distress accompanied by high fever ≥39°C, age younger than 3 months, focal lung crackles, worsening of clinical presentation, or the need for intensive care unit admission [12,13].
3. RESULTS
3.1. Characteristics of Study Participants
We initially assessed the electronic records of 171 patients admitted with acute bronchiolitis at HMG. Among these, 21 patients were excluded. A total of 150 patients met the necessary inclusion criteria and were recruited for the study (Figure 1).
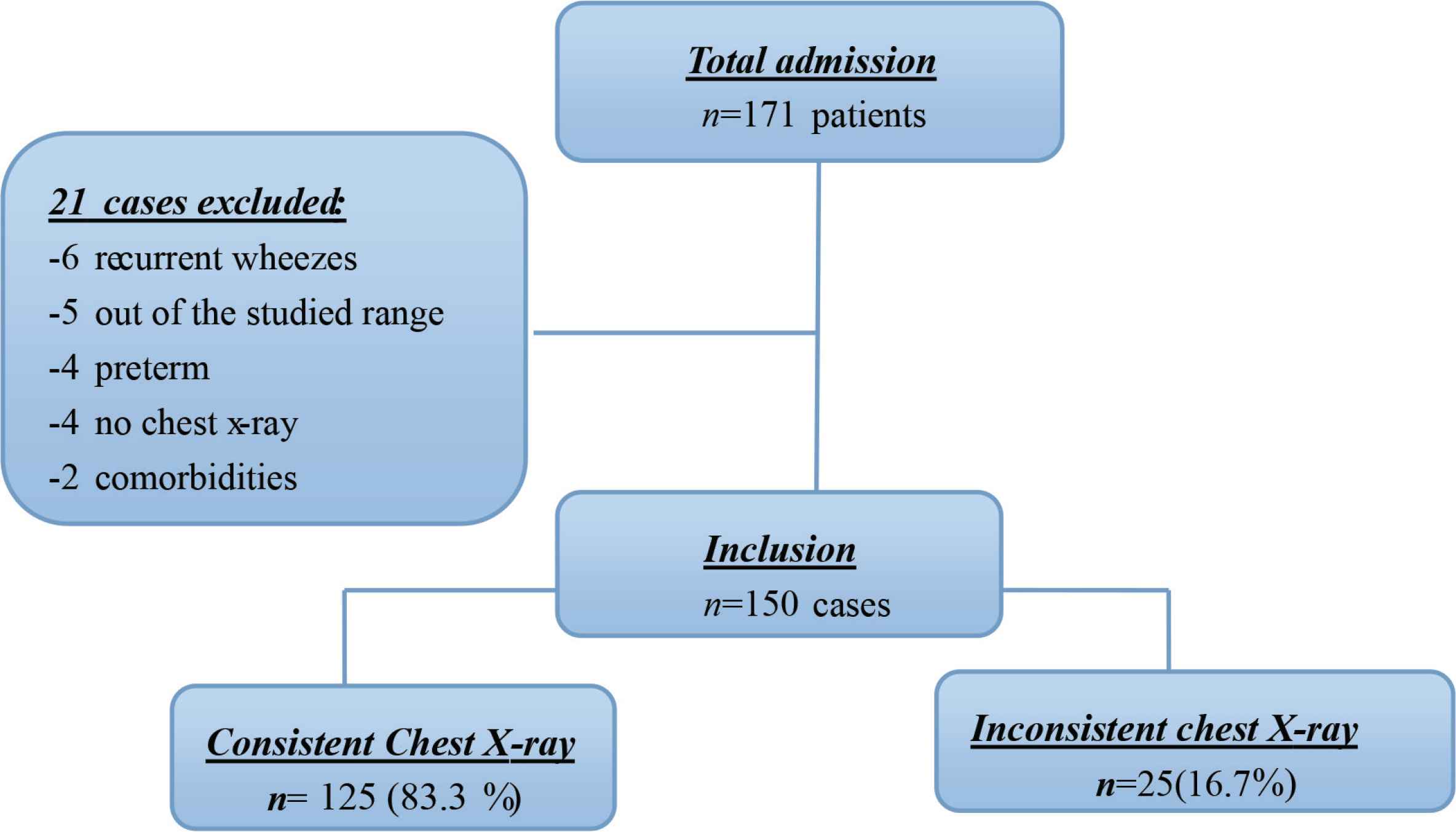
Flowchart study population enrollment.
The age of the study groups ranged between 1 month and 24 months, with a mean of 10.03 ± 4.92 months. The gender frequency was 55% (83/150) for males and 45% (67/150) for females. Demographic and clinical characteristics of children with normal and abnormal chest radiographies are illustrated in Table 1.
| Variables | Consistent | Nonconsistent | p |
|---|---|---|---|
| Age | 10.23 ± 5.10 | 9.04 ± 3.78 | 0.27, nsa |
| Sex | |||
| Male | 70 | 13 | 0.98, nsb |
| Female | 55 | 12 | |
| Fever | 37.68 ± 0.94 | 38.29 ± 1.25 | 0.57, nsa |
| RR | 45.31 ± 4 | 47 ± 7.1 | 0.14, nsa |
| SpO2 | 94.6 ± 2.5 | 92.05 ± 2.2 | 0.15, nsa |
| Neutrophil | 5.53 ± 6.33 | 6.61 ± 6.46 | 0.96, nsa |
| CRP | 12.08 ± 12.73 | 16.24 ± 20.8 | 0.21, nsa |
| RSV | 50 | 8 | 0.22, nsb |
| PICU | 9 | 2 | 0.96, nsb |
Independent t-test was used to calculate p-values (p< 0.05).
Chi-square test/Fisher’s exact test was used as appropriate.
ns, nonsignificant; RR, respiratory rate; SpO2, oxygen saturation.
Demographics and health characteristics of the study population
3.2. Classification of Chest Radiographic Findings
The chest x-ray scans were divided according to radiological findings. Consistent chest radiographs included bilateral infiltrations, hyperinflations, peribronchial cuffing, and atelectasis. Nonconsistent radiographic findings included isolated pulmonary infiltration, lobar pneumonia, consolidations, or effusion. The radiological pattern of the single chest x-ray is miscellaneous and diverse; however, according to the most consistent radiological findings, the distribution of the patients is illustrated in Table 2.
| Radiological pattern | Chest x-ray finding | Frequency (n) |
|---|---|---|
| Consistent chest x-ray | Bilateral infiltration | 88 |
| Hyperinflation | 7 | |
| Peribronchial cuffing | 24 | |
| Atelectasis | 6 | |
| Nonconsistent chest x-ray | Consolidation | 6 |
| Isolated infiltrations | 19 |
Chest x-ray findings
3.3. Clinical Predictors of Chest Radiographic Abnormalities in Study Participants
Multivariate logistic regression was used to determine the possible clinical predictors of chest x-ray abnormalities among the studied factors. The results revealed no variables with statistical significance (Table 3).
| Variable | Parameter estimate | SE | p |
|---|---|---|---|
| Age | –0.006 | 0.067 | 0.9 |
| RR | –0.053 | 0.05 | 0.3 |
| SpO2 | 0.116 | 0.172 | 0.5 |
| CRP | –0.26 | 0.027 | 0.3 |
RR, respiratory rate; SE, standard error; SpO2, oxygen saturation.
Clinical predictors of abnormal chest x-ray results
3.4. Indication of Chest X-rays in Young Children
The data showed that 61 (40.7%) of the chest x-rays taken were indicated according to AAP/NICE guidelines. The rest of chest x-rays performed 89 (59.3%) were not indicated. The frequency of the chest x-ray finding based on clinical indication is illustrated in Figure 2 and Table 4.
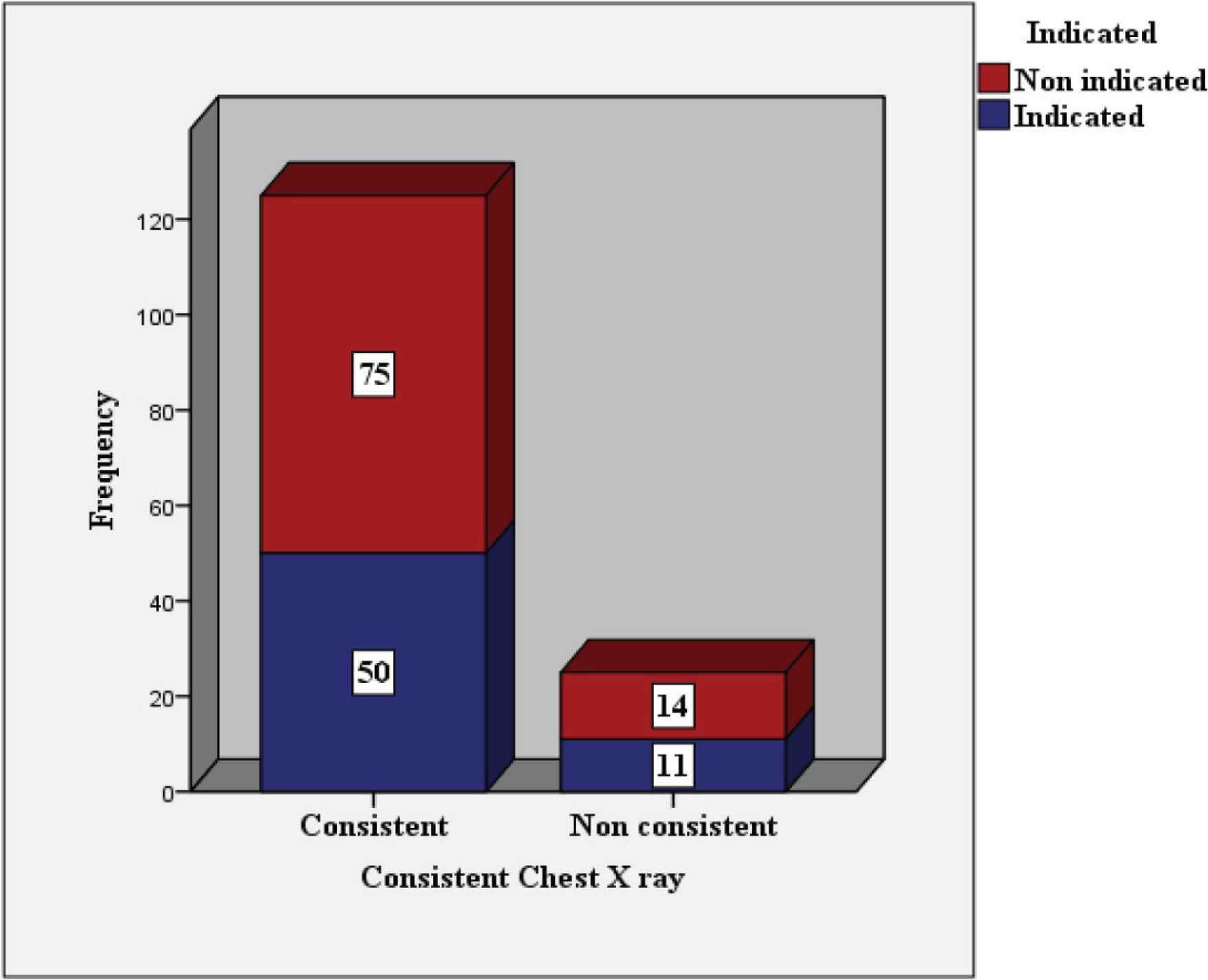
Chest x-ray findings based on clinical indications.
| Variables | Consistent | Nonconsistent |
|---|---|---|
| Fever ≥39°C | 24 | 5 |
| <3 months | 12 | 3 |
| Focal lung crackles | 8 | 2 |
| Worsening/need for intensive care units | 7 | 3 |
Proportion of clinical indicators based on chest x-ray findings
4. DISCUSSION
It is not surprising that the management of acute bronchiolitis varied considerably in the same facility. To our knowledge, this is the first study to explore imaging utilization in our center.
The study demonstrated that radiological findings in patients with the typical presentation of bronchiolitis are usually consistent with the disease behavior (83.3%). These findings include bilateral infiltration, peribronchial cuffing, or hyperinflation. This is in accordance with the findings of Castillo et al. [14], who demonstrated that 89.2% of 128 infants assessed had nonspecific alteration of chest findings consistent with the bronchiolitis. Similarly, Christakis et al. [15] retrospectively reviewed thousands of patients in 30 different hospitals in the United States and concluded that the vast majority was without significant radiological findings. It is worth mentioning that no obvious correlation, such as the need for immediate intensive care unit admissions, was found between chest x-rays and disease severity. In the same way, Dawson et al. [16] concluded that there was no statistical significance between clinical severity and chest film findings when they assessed 153 patients. In contrast to our result, Gonçalves et al. [17] found that patients with abnormal chest x-ray results had severe disease course with a higher risk of invasive ventilation.
In order to evaluate what features should prompt the clinician to request radiographs, we investigated different clinical variables for the prediction of chest x-ray abnormalities. These include the infant’s age, sex, temperature, respiratory rate, oxygen saturation, absolute neutrophil counts, CRP, and nasopharyngeal RSV aspirate. Furthermore, the decision on PICU admission according to the hospital scoring system, pediatric early warning signs, was also investigated. First, no demographic difference was observed in our data. Similarly, the clinical variables were not statistically significant among the study population, especially when patients were not hypoxic (SpO2 > 90%). Furthermore, test results including RSV, CRP, and neutrophil results were not significant to predict the radiographic abnormalities in our study. Instead, the clinician is advised to reserve imaging for those indicated and to consider clinical follow-up as an alternative. Correspondingly, García et al. [18] concluded that there was no relation between the clinical variables and chest x-ray changes. In the same way, Ecochard-Dugelay et al. [19] screened 401 patients and suggested that clinical variables are not predictive for radiographic abnormalities.
Finally, as part of a quality improvement project, we audited the indications of chest x-rays that had been requested and compared them to recommendations of the AAP and NICE guidelines. The study demonstrates that 59.3% of the chest x-rays were not indicated. High-grade fever (≥39°C) and age <3 months were the most frequent reasons behind chest imaging. Out of non-indicated radiography, 84.2% had radiographic findings consistent with acute bronchiolitis. These results concur with international guidelines that recommend discriminate chest radiography of patients.
Development of local policies, frequent re-auditing, and educational sessions can lead to a reduction in the number of unnecessary chest x-rays and enhance compliance with national and international guidelines.
Nonetheless, there are some limitations that should be noted and considered for further research. Because of its retrospective nature, the study depended on the availability of clear well-documented notes. The inaccuracy of information may lead to the underestimation of chest radiography indications. Thus, prospective studies on larger samples are advisable.
5. CONCLUSION
The majority of chest radiographs (83.3%) were benign in previously well children presenting with typical bronchiolitis picture. Clinical variables are of little prognostic value. Indiscriminate chest radiography is not recommended. The study advises strict adherence to the guidelines to decrease unnecessary radiography. Ongoing education and re-auditing of practice continue to expand this body of evidence.
CONFLICTS OF INTEREST
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
AUTHORS’ CONTRIBUTION
MA, RB and AM contributed in conceptualization, designing and writing which includes review and editing the manuscript. RB contributed in data collection. MA contributed in formal analysis and writing the original draft. AM supervised the project. However, all the authors review the manuscript and approve the final draft of the manuscript.
FUNDING
The author received no financial support for the research, authorship and publication of this article.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - M. Abdoun AU - Reham Babiker AU - Abdelmoneim Mahgoub PY - 2020 DA - 2020/07/05 TI - Quality Improvement Project to Reduce Unnecessary Chest X-ray in a Tertiary Center JO - Dr. Sulaiman Al Habib Medical Journal SP - 186 EP - 189 VL - 2 IS - 4 SN - 2590-3349 UR - https://doi.org/10.2991/dsahmj.k.200702.001 DO - 10.2991/dsahmj.k.200702.001 ID - Abdoun2020 ER -
