Delayed Posttraumatic Tension Pneumocephalus: A Rare Case Report and Review of the Literature
- DOI
- 10.2991/dsahmj.k.200316.001How to use a DOI?
- Keywords
- Tension pneumocephalus; traumatic pneumocephalus; cerebrospinal fluid leak; craniotomy; rhinorrhea; head trauma; frontal bone; frontal sinus; dura
- Abstract
Pneumocephalus (PNC) is defined as a pathological air collection inside the skull in the epidural, subdural, subarachnoid, intraventricular, or intraparenchymal compartments. The rate at which the air accumulates inside the cranium could be acute (<72 h) or delayed (≥72 h). Tension PNC (TP) occurs when the air collection exerts an abnormally high pressure on the brain, compared with the pressure outside the cranium, resulting in a mass effect and neurological symptoms. PNC, also called pneumocranium, can be spontaneous or acquired. Trauma remains the most common cause of acquired PNC. A 34-year-old gentleman presented with a short duration history of sudden severe headache, vomiting, and clear fluid leak from the left nostril. He had history of trauma, which occurred 3 months ago. Computed Axial Tomography (CAT) scan revealed intra-axial and extra-axial PNC plus an old depressed fracture of the left side of the frontal bone. Eventually, he was scheduled for surgical bifrontal craniotomy, repair of posterior sinus fracture, and recanalization of frontal sinus. Delayed TP is a rarely occurring pathology, and in rare cases it can occur many weeks after trauma. It is a life-threatening neurosurgical emergency that needs to be managed on urgent basis. Based on the literature review and the success achieved in this case, early surgical management is the optimal treatment for TP.
- Copyright
- © 2020 Dr. Sulaiman Al Habib Medical Group. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Pneumocephalus (PNC) is defined as a pathological air collection inside the cranium—particularly in the epidural, subdural, subarachnoid, intraventricular, or intraparenchymal compartment. Another term, “pneumocranium,” was also used by some authors to describe the same pathology.
Most cases of PNC are acquired, for example, they can be caused by trauma to the cranium or the face, adjacent air sinus infections, neurosurgical or otological interventions, and neoplasms.
By contrast, “spontaneous” PNC has been very rarely reported [1,2]. The rate at which the air accumulates inside the cranium could be acute (<72 h) or delayed (≥72 h) [3]. PNC has two clinical entities: simple and Tension PNC (TP). The latter is defined as intracranial air collection that exerts an abnormally high pressure on the brain parenchyma, compared with the pressure outside the cranium, resulting in a mass effect detected by images of Computed Axial Tomography (CAT) scan or Magnetic Resonance Imaging (MRI) during investigation. This will eventually lead to the appearance of significant neurological deficit if not treated promptly. By contrast, simple PNC is usually asymptomatic and requires no intervention [4–6].
2. CASE DESCRIPTION
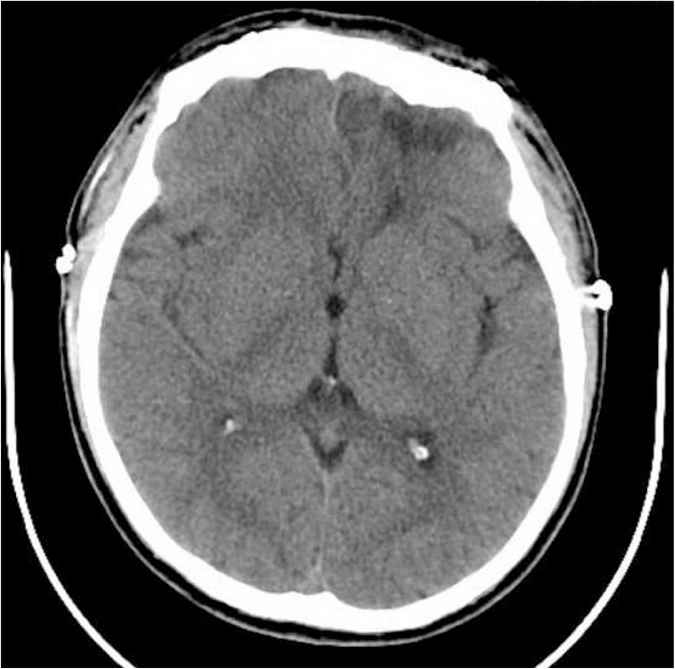
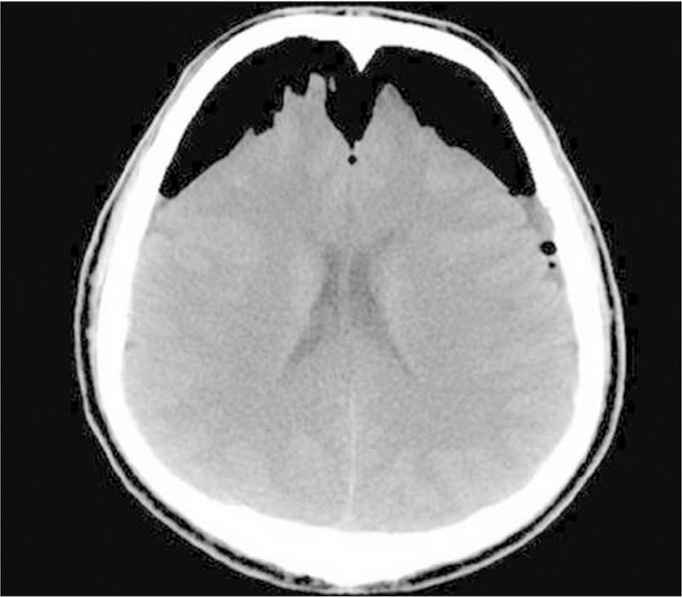
A 34-year-old gentleman presented to the emergency room complaining of sudden severe headache that started on the same day of his presentation. The headache was associated with frequent vomiting and clear fluid leakage from the left nostril. He had history of head trauma 3 months ago in another country, but did not require any surgical intervention as he claimed. Upon examination, he had normal vital signs. Results of his head examination revealed an old mild depression at the forehead region. His Glasgow Coma Scale (GCS) score was 15/15. Fortunately, his neurological examination was completely normal including the examination results of motor, sensory, cerebellar, and cranial nerves. His initial blood investigations were completely within the normal range. CAT scan was performed urgently and revealed a large area of encephalomalacia in the left frontal lobe filled with air, which communicated with the related frontal horn of the left lateral ventricle (Figure 1). A small defect was also seen in the posteroinferior aspect of the left frontal sinus, associated with multiple foci of PNC seen along the convexity of the brain, in the basal cisterns, and lateral and third ventricles as well. The CAT scan also showed an old depressed fracture of the left side of the frontal bone (depressed by 7.4 mm). Moreover, the volume of air in the intracranium cavity was estimated by the reporting neuroradiologist to be approximately 45 mL of air based on the patient’s CAT scan. The patient was urgently evaluated by the neurosurgical team and was taken on the same night for surgical repair. Accordingly, he underwent bifrontal craniotomy, repair of posterior sinus fracture, and recanalization of the frontal sinus. Postoperatively, he had an uneventful smooth recovery with rapid resolution of his headache. A repeat CAT scan of the brain was obtained and showed complete resolution of the PNC with small air foci noted in the right frontal horn of the lateral ventricle (Figure 2). On the 11th postoperative day, the patient was discharged home symptom-free.

Encephalomalacia in the left frontal lobe filled with air that communicates with the frontal horn of the left lateral ventricle.
Complete resolution of the pneumocephalus with small air foci noted in the right frontal horn of the lateral ventricle.
3. DISCUSSION
Pneumocephalus may result from craniofacial trauma, otorhinolaryngological surgery, or neurosurgical operations. In rare cases, it may arise from neoplasms, central nervous system infections, congenital skull bone defects, or barotrauma [7].
The pathophysiology behind PNC has been rationalized to be the result of one of two postulated theories, one of which is the “ball valve mechanism”—the increase in intracranial pressure in the presence of a dural defect in which tissues could make a one-way valve resulting in air trapping inside the cranium. The other theory is the “inverted soda bottle mechanism.” Cerebrospinal Fluid (CSF) leak accompanied by a defect in the meninges results in a decrease in intracranial pressure, allowing air to enter the cranium to equalize the pressure [1,8].
Intracranial postoperative infection had been reported previously in one case involving a gunshot victim approximately 16 weeks after the first craniotomy [6]. It was postulated to be caused by gas-producing organism based on the clinical scenario of the case.
The incidence of PNC remains unknown, simply because it is often missed and reported less frequently. More deliberate use of CAT scans and MRI has helped in identifying more of these cases.
Tension PNC usually occurs acutely in trauma victims or postoperatively. By contrast, delayed TP is rarely reported. It can present days or weeks after the insult. In one extreme case, Kon et al. [9] reported a patient with TP in 2003 who had presented 7 years after initial craniotomy.
Pillai et al. [5] conducted a comprehensive review of all reported cases of traumatic TP in the literature and identified 20 of such cases. In their review, there were 17 males and three females. The most common etiology by far was trauma. Similar to our case, Pillai et al. [5] reported that frontal bone/sinus fracture is the most common injury associated with traumatic TP. Nineteen cases were picked up by CAT scans and one by MRI. The most common presenting symptomatology was decreased level of consciousness. Of note, the overall mortality in their review was 2/20 (10%).
Although PNC does not usually have a clear presentation, headache is the most frequently reported symptom. Other manifestations include CSF rhinorrhea, otorrhea, meningismus, seizures, vomiting, cranial nerve palsies, weakness, or paralysis [1,8]. Interestingly, some patients experienced hearing sounds in their head. This phenomenon is called “bruit hydro-aérique,” as it resembles the splash succession sounds upon postural change. Sivasubramaniam et al. [10] reported that 73% of patients with postoperative pneumocephaly had experienced intracranial sounds.
The volume of air necessary to produce tension, that is, “mass effect,” is a source of debate. Although it was believed to be up to 75 mL of air, this has not been proven.
The combination of clinical features and radiological findings, on CAT scan, is mandatory to support the diagnosis of TP. Intracranial air may accumulate at any site, that is, at epidural, subdural, subarachnoid, ventricular, or intracerebral sites. Interestingly, if it collects at the subdural site and extends downward to the interhemispheric fissure, it shows a unique appearance on CAT scan referred to radiologically as “Mount Fuji sign” [6,11,12] (Figure 3).
“Mount Fuji Sign” with tension pneumocephalus. Adapted with permission from Gokmen et al. [12].
The best imaging modality to diagnose PNC is CAT scan. It is readily available and quite sensitive. It can detect as little as 0.5 mL of air compared with at least 2 mL that can be detected by plain skull imaging, which is an outdated option with which to investigate head trauma [5,13].
Magnetic resonance imaging can also be used to detect intracranial air in trauma victims; however, it is expensive and unavailable in some centers, particularly in the rural setting.
Pneumocephalus management depends on the volume of air within the cranium and the clinical neurological presentation. Therefore, cases need to be assessed individually by the neurosurgical team. Urgent surgical decompression is necessary for TP or major clinical neurological deficit as the condition maybe fatal. Those serious cases are at great risk of circulatory collapse and herniation if not addressed urgently, whereas cases with small volume of air or minor neurological symptoms can be managed conservatively. The initial nonoperative supportive measures for all cases should include antibiotic prophylaxis, high flow oxygen supplementation, head supine or Trendelenburg positioning, antipyretics, and analgesia.
Multiple surgical options are available for the management of PNC including craniotomy, endoscopy, burr holes, needle aspiration, and ventriculostomy placement [8,14].
4. CONCLUSION
Posttraumatic TP is a rare condition that is commonly associated with cranial base and facial injuries and, as our case has shown, can occur many weeks after the initial trauma or craniotomy. TP is a life-threatening neurosurgical emergency that requires urgent intervention to decompress the increasing intracranial pressure. Based on the literature review and the success of this case, surgical management is the optimal treatment for TP. Moreover, considering TP pathophysiology, patients should have long-term follow up after being discharged from the hospital.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
MAA contributed in study data curation and writing of original draft. TAA contributed in study supervision, review and editing of the manuscript.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Tawfiq Abdulmohsen Almezeiny AU - Mody Abdulrahman Almarshad PY - 2020 DA - 2020/03/19 TI - Delayed Posttraumatic Tension Pneumocephalus: A Rare Case Report and Review of the Literature JO - Dr. Sulaiman Al Habib Medical Journal SP - 1 EP - 3 VL - 2 IS - 1 SN - 2590-3349 UR - https://doi.org/10.2991/dsahmj.k.200316.001 DO - 10.2991/dsahmj.k.200316.001 ID - Almezeiny2020 ER -
