Aggressive renal sympathetic denervation approach to treating resistant hypertension: A fresh start?
- DOI
- 10.1016/j.artres.2016.10.143How to use a DOI?
- Keywords
- Resistant hypertension; Renal sympathetic denervation; Blood pressure
- Abstract
A multivariable analysis identified predictors of systolic blood pressure change in SYMPLICITY HTN-3 trial. Additional analyses examined the influence of medication changes, results in selected subgroups and procedural factors. Greater reductions in office and ambulatory systolic blood pressure, and heart rate were observed with a higher number of ablations and energy delivery in a four-quadrant pattern. Based on this information, we selected a white patient with baseline office systolic blood pressure >180 mmHg, using aldosterone antagonist, non-using vasodilators, and performed an aggressive RSD approach.
Male patient, 40 years old, white, referred by the attending physician to our service due to a complaint of dyspnea, dizziness, and headache. Resistant hypertensive patient, already being tested various therapeutic regimens. The procedure did not show any vascular complications and the patient was discharged after 24 h hospitalization, clinically stable, walking without difficulty, and presenting mean office blood pressure levels during the 24 h post procedure in 130/82 mmHg. After 6 months of follow-up, the office blood pressure was 140/89 mmHg, and the 24-h ABPM values were: mean = 132/83 mmHg, awake = 135/86 mmHg, and sleeping = 126/75 mmHg, and did not present any symptoms.
- Copyright
- © 2016 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Introduction
The recent results of the SYMPLICITY HTN-3 trial have challenged preclinical science, clinical anecdote, and the consistency observed across early phase trials. Although the trial demonstrated the safety of renal sympathetic denervation (RSD), among 535 patients identified with treatment resistant hypertension the difference in 6-month blood pressure decline between renal sympathetic denervation RSD and sham-treatment groups was not significantly different for office or ambulatory measures.1 Based on the results of multivariable analysis to identify predictors of systolic blood pressure change, and analysis of pre-specified and post hoc subgroups to identify potential confounding factors that may have affected the trial results, three areas of investigation were pursued: changes in antihypertensive medications, outcomes in selected subgroups, and detailed assessment of procedural data that may have impacted the delivery of effective RSD. Nevertheless, the EnligHTN I study provides evidence that the multi-electrode ablation system constitutes a safe method of RSD in patients with drug resistant hypertension and is accompanied by an early and sustained reduction of office, ambulatory and home blood pressure at 24 months after the procedure. However, none of the potential predictive demographic variables assessed were associated with response to RSD at long term follow-up.2
Kandzari et al. evaluated patients with resistant hypertension were randomized 2:1 to RSD (n = 364) or sham (n = 171). The primary endpoint was the difference in office systolic blood pressure change at 6 months. Multivariable analysis identified predictors of systolic blood pressure change. Additional analyses examined the influence of medication changes, results in selected subgroups and procedural factors. Between randomization and the 6-month endpoint, 39% of patients underwent medication changes. Predictors of office SBP reduction at 6 months were baseline office systolic blood pressure ≥180 mmHg, aldosterone antagonist use, and non-use of vasodilators; a number of ablations were a predictor in the RSD group. Non-African-American patients receiving RSD had a significantly greater change in office SBP than those receiving sham; −15.2 + 23.5 vs. −8.6 + 24.8 mmHg, respectively (P = 0.012). Greater reductions in office and ambulatory systolic blood pressure, and heart rate were observed with a higher number of ablations and energy delivery in a four-quadrant pattern.3
Based on this information, we selected a white patient with baseline office systolic blood pressure >180 mmHg, using aldosterone antagonist, non-using vasodilators, and performed an aggressive RSD approach.
Case presentation
Male patient, 40 years old, white, referred by the attending physician to our service due to a complaint of dyspnea, dizziness, and headache. Resistant hypertensive patient, already being tested various therapeutic regimens. Not tolerate clonidine. In use, currently: Nebivolol 5 mg once a day, chlorthalidone 25 mg once a day, amlodipine 10 mg once a day, Valsartan 320 mg once a day, spironolactone 50 mg once a day, and furosemide 40 mg twice a day.
Physical exam: mean blood pressure = 194/120 mmHg, heart rate 78 bpm, sinus thythm.
Complementary tests
The computerized tomography presented normal aorta and kidney. Eco-Doppler renal arteries from 2015 showed normal anatomy, normal flow rates (up to 100 cm/s), without stenosis, the renal-aorta index <3.5 cm (normal). Echocardiogram from 2015 showed ventricular end diastolic volume = 5.4 cm, left atrium = 3.1 cm, interventricular septum thickness at the end of diastole = 0.8 cm, left ventricular mass indexed (kg/m2) – 104.3 g/m2, left ventricular ejection fraction measured by Simpson’s method (LVEF) 69%. The myocardial scintigraphy 2015 showed no ischemia, LVEF = 44%, without necrosis. The polysomnography from 2015 showed 10.8/h (mild), some desaturation periods, decreased sleep efficiency. Creatinine value was 0.8 mg/dL, consequently the estimated glomerular filtration rate was 112 mL/min/1.73 m2 (CKD-EPI CREATININE, 2009), with albumin: creatinine = 8 mg/g (Table 1).
| 24-h ABPM | Mean, mmHg | Awake, mmHg | Sleeping, mmHg |
|---|---|---|---|
| 2013 | 166/91 | 166/91 | 137/103 |
| 2014 | 164/113 | 164/117 | 112/81 |
| 2015 | 147/125 | 147/127 | 137/116 |
24-h ambulatory blood pressure measurements (ABPM) during the follow-up.
The patient signed the informed consent and the ethics committee approved the execution of the case. The procedure was performed in the catheterization laboratory with direct visualization using fluoroscopy and radiopaque contrast. The patient remained under unconscious sedation and catheterization of the right femoral artery by the standard Seldinger technique was performed using an 8-Fr valved short sheath, after sub cutaneous injection of local anesthetic. Subsequently, an RDC catheter was introduced into this sheath by the standard “over the wire” technique. Unfractionated heparin was administered intravenously, targeting an activated coagulation time (ACT) between 250 and 350 s. This sheath was advanced to the level of the renal arteries, and the ostia were located with nonselective aortography. The introducer was then positioned to anchor at the ostium of each renal artery. The patient underwent to RSD using the system EnligHTN™ (St. Jude Medical, St. Paul, Minnesota, USA) inserted through the RDC catheter, as shown in Fig. 1. The number of ablation spots per artery was 27 in the left renal artery and 36 in the right renal artery (Fig. 2). The procedure was performed without any complications, and the patient remained clinically stable and awoke properly from sedation. Intravenous protamine was infused at the end of the procedure, and manual compression of the femoral artery was performed with a mean time of 15 min, followed by the compressive dressing. The procedure did not show any vascular complications and the patient was discharged after 24 h hospitalization, clinically stable, walking without difficulty, and using just aspirin 100 mg once a day, valsartan 320 mg once a day, chlorthalidone 25 mg once a day Nebivolol 5 mg once a day, presenting mean office blood pressure levels during the 24 h post procedure in 130/82 mmHg. After 6 months of follow-up, the office blood pressure was 140/89 mmHg, and the 24-h ABPM values were: mean = 132/83 mmHg, awake = 135/86 mmHg, and sleeping = 126/75 mmHg, and did not present any symptoms.
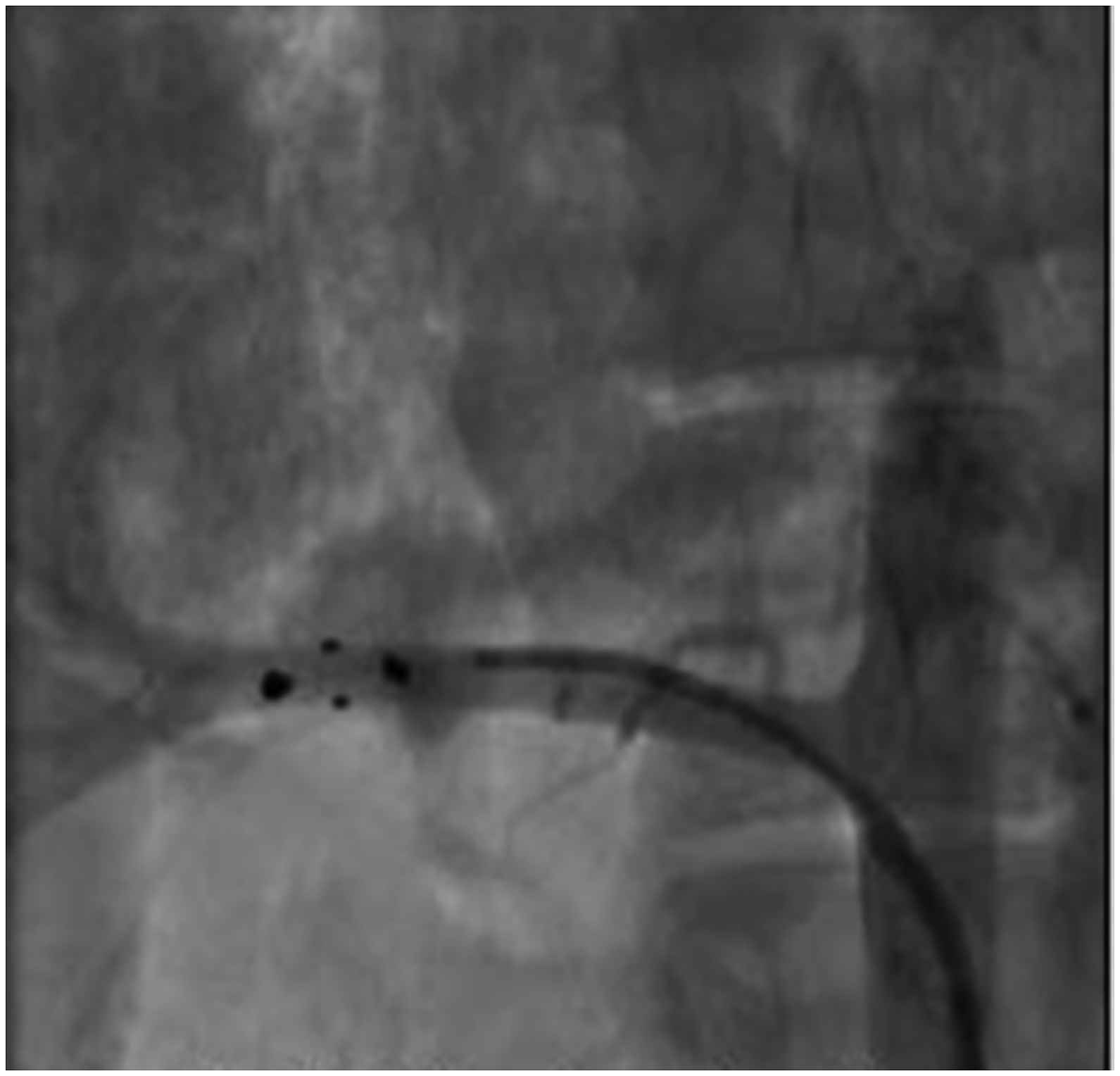
The ablation catheter EnligHTN™ inserted through the RDC sheath and placed in the distal part of the right renal artery.
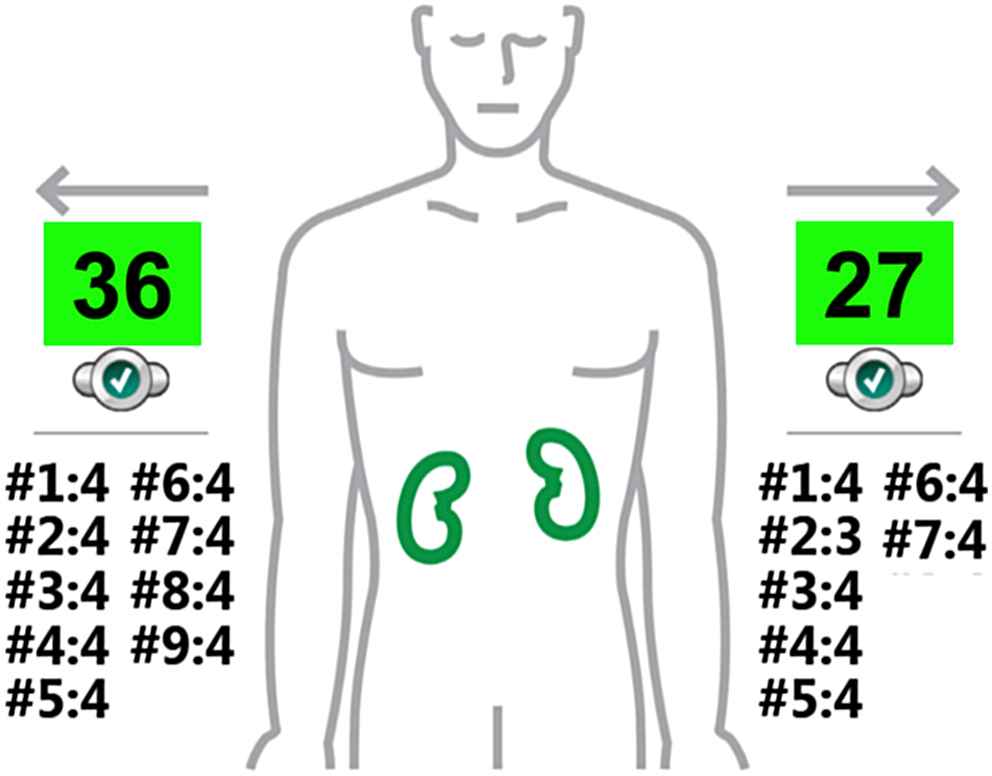
Number of ablation spots performed in the right and left renal arteries using the EnligHTN™ system.
Conclusion
This patient, selected according to predictors of success postulated by the SYMPLICITY HTN-3 associated to an aggressive RSD approach, presented a marked reduction in office blood pressure and 24-h ABPM.
References
Cite this article
TY - JOUR AU - Márcio Galindo Kiuchi AU - Luis Marcelo Rodrigues Paz AU - Shaojie Chen PY - 2016 DA - 2016/11/01 TI - Aggressive renal sympathetic denervation approach to treating resistant hypertension: A fresh start? JO - Artery Research SP - 42 EP - 44 VL - 16 IS - C SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2016.10.143 DO - 10.1016/j.artres.2016.10.143 ID - Kiuchi2016 ER -
