Anatomical characterization of the vertebral artery from a local study population using angiography by computed tomography
- DOI
- 10.1016/j.artres.2018.07.002How to use a DOI?
- Keywords
- Vertebral artery; Anatomic variation; Computed tomography angiography; Vertebral artery dissection
- Abstract
Purpose: Despite most anatomical variations of the vertebral artery (VA) related to the origin and intraforaminal entrance remain asymptomatic because of the collateral irrigation system, it is important to know their anatomical presentation in order to prevent complications than could be neurologically devastating for patients. The aim of this study was to characterize the VA anatomy using computed tomography angiography (CTA) in the Colombian population.
Methods: Study was descriptive, observational and cross–sectional. Neck and thorax CTA studies performed between 2010 and 2017 in adult population were reviewed. Studies with low image-quality or artifacts, or patients with vascular malformations or injuries history, as well as non-Colombian patients were excluded. Frequencies and percentages were calculated.
Results: 500 CTA were studied, 362 (72.4%) from male patients, 138 (27.6%) from female patients. In the 18% (n = 90) of the study population, there was at least one VA variation; 73.33% (n = 66) of these cases were male patients and 26.67% (n = 24) were female patients, however, the percentage of VA variations was similar in both genders (18.23% men, 17.39% women).
Conclusion: Our findings suggest that the VA anatomy should be assessed prior to any surgical procedure in thoracic or neck region that involves the VA as any complication may be deleterious for the patient. Patients with neurological symptoms and VA variations should be evaluated for arterial dissection. VA variants should be included in the radiology report as they may be useful for clinicians not only for diagnostic but also for preventive purposes.
- Copyright
- © 2018 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Introduction
For the study of the vertebral artery (VA), the classical anatomy has divided it from caudal to cephalic in 4 segments. The prevertebral part, from VA origin in the subclavian artery (SA) to the transverse process of C7, where the VA ascends posterior to the common carotid artery and vertebral vein, and anterior to the prevertebral muscles and the cervicothoracic ganglion; the transverse or cervical segment, where the VA enters commonly through the transverse foramen of C6 to ascend through the transverse foramina of the first six cervical vertebrae, until reaching the transverse process of the Atlas (C1), usually accompanied by the vertebral nerve and the vertebral venous plexus in front of the ventral branches of the corresponding spinal nerves; the atlantic or suboccipital portion, where the VA pass through the suboccipital trigone to the foramen magnum; and the intracranial segment, when the VA enters to the skull going through the dura mater and the arachnoid, ascending anterior to the roots of the hypoglossal nerve and going medially and anterior to the medulla oblongata to anastomose with the contralateral VA giving origin to the basilar artery.1–5
The main variations of the VA are related to the origin, course, and intraforaminal entrance, and may be unilateral or bilateral in both male and female patients.6 Although most variations of the VA remain asymptomatic because of the collateral irrigation system, in some cases it is important to know its course and anatomy, such as management of thoracic and neck trauma or surgical procedures with an anterior approach to the cervical spine where complications may involve the cerebellum, brainstem, and spinal cord, being potentially devastating for patient.7–9 Moreover, despite most common etiology of the VA dissection is blunt trauma, spontaneous dissection, and antecedent of neck manipulation or other sudden movements, VA dissection may also result from uncommon intraforaminal entrance induced by normal physiologic motion.10 VA dissection has been associated with thrombosis, occlusion, dissection-induced stenosis, and pseudoaneurysm formation; and it represents, with the carotid dissections, around the 2% of all ischemic strokes, and up to 25% of the cases in young and middle-age patients.11–14 Knowledge of the VA anatomy may be useful in cases when patients have neurologic symptoms with physiologic cervical movements without trauma history, as it may correspond to a VA dissection.10
Anatomy of the VA has been described extensively in both in-vivo and postmortem studies, mainly in high-income countries. However, to our knowledge, this is the first study of VA anatomy concerning the origin and intraforaminal entrance from the Colombian population with the largest sample in the studies reported from the low- and middle-income countries. Hence, the aim of this study was to characterize the VA anatomy using computed tomography angiography in the Colombian population.
Methods
Subjects
All neck and thorax computed tomography angiographies performed in adult population (older than 18 years) between 2010 and 2017 were reviewed. Studies with low image-quality, or with artifacts related to beam hardening or patient movement that could affect the assessment of the vascular structures of interest were excluded. Patients with history of vascular malformations or injuries, as well as non colombian patients were also excluded. The Institutional Ethics Committee approved this study.
Acquisition protocol
All studies were performed in a multidetector computed tomography equipment (LightSpeed, VCT, General Electric Medical Systems, USA), obtaining axial acquisitions from the thoracic operculum to the base of the skull in three phases: a single phase, an arterial phase after injection of the contrast medium, and a venous phase after the arterial phase. A 75 mL of water-soluble contrast medium was used at an injection rate of 5.0 mL/s with subsequent injection of 40 mL of saline at the same rate. The images were obtained from the Picture Archiving and Communication System (PACS) from the institution, and they were analyzed with the Vascular CT workflow of Syngo. Via VA30A_HF06 (SIEMENS, Germany) using multiplanar, maximum intensity projections and volume rendering techniques.
Image interpretation
All images were reviewed and analyzed by a radiologist with 16 years of experience in neck and thorax studies, and a professional in morphology specialist in anatomy with more than 10 years of experience in both in-vivo and post-mortem morphological studies. As variables were considered sex, laterality of the variation, the origin of the VA and first foramen of penetration of the artery.
Statistical analysis
Frequencies and percentages were calculated using Excel® for the prevalence of VA regarding the sex, location, the origin of the vessel and the first foramen of penetration of the artery.
Results
From 705 studies initially reviewed, 500 CTA studies were included after exclusion criteria, 362 (72.4%) from male patients, and 138 (27.6%) from female patients. The mean age was 41.94 years-old, and the standard deviation was 18.79 years-old. In the 18% (n = 90) of the study population, there was at least one variant of the vertebral arteries; 73.33% (n = 66) of these cases were male patients and 26.67% (n = 24) were female patients, however, the percentage of the presence of some variation was similar in both genders (18.23% in men, 17.39% in women).
The right vertebral artery was originated from the right subclavian artery in all male patients, while in female patients, it was originated from the right subclavian artery in 137 (99.3%) patients and from the common carotid artery in 1 (0.7%) patient. In male patients, the left vertebral artery was originated from the left subclavian artery in 332 (91.7%) cases and from the aortic arch in 30 (8.3%) cases, while in female patients the origin was from the left subclavian artery in 126 (91.3%) patients and from aortic arch in 12 (8.7%) patients. Regarding the origin, bilateral variations were not observed.
The relationship among the sex, laterality and cervical vertebrae where the vertebral artery enters through the transverse foramen is detailed in Tables 1 and 2 for all male and female patients, respectively. There was only one case of aberrant right VA in a female patient with intraforaminal entrance at C5. Table 3 describes all the aberrant left VA cases (n = 42) regarding the relationship between sex and cervical vertebrae where the artery enters through the transverse foramen.
| Right VA | |||||||
|---|---|---|---|---|---|---|---|
| C3 | C4 | C5 | C6 | C7 | Total | ||
| Left VA | C3 | – | – | – | 1 (0.28%) | – | 1 (0.28%) |
| C4 | – | – | 1 (0.28%) | 3 (0.82%) | – | 4 (1.10%) | |
| C5 | – | 1 (0.28%) | 2 (0.55%) | 25 (6.91%) | – | 28 (7.73%) | |
| C6 | – | 6 (1.66%) | 13 (3.59%) | 299 (82.60%) | 4 (1.10%) | 32 (88.95%) | |
| C7 | – | – | 1 (0.28%) | 5 (1.38%) | 1 (0.28%) | 7 (1.93%) | |
| Total | – | 7 (1.93%) | 17 (4.70%) | 333 (91.99%) | 5 (1.38%) | ||
Relationship among the sex, laterality and the cervical vertebrae where the VA enters in male patients.
| Right VA | |||||||
|---|---|---|---|---|---|---|---|
| C3 | C4 | C5 | C6 | C7 | Total | ||
| Left VA | C3 | – | – | – | – | – | |
| C4 | – | – | – | – | – | ||
| C5 | – | – | 2 (1.45%) | 9 (6.52%) | – | 11 (7.97%) | |
| C6 | – | – | 7 (5.07%) | 117 (84.78%) | 1 (0.72%) | 125 (90.58%) | |
| C7 | – | – | – | 2 (1.45%) | – | 2 (1.45%) | |
| Total | – | – | 9 (6.52%) | 128 (92.75%) | 1 (0.72%) | ||
Relationship among the sex, laterality and the cervical vertebrae where the VA enters in female patients.
| Cervical vertebrae | Total (%) n = 42 | Male | Female |
|---|---|---|---|
| C3 | 1 (2.38%) | 1 | 0 |
| C4 | 7 (16.67%) | 3 | 4 |
| C5 | 28 (66.67%) | 20 | 8 |
| C6 | 4 (9.52%) | 4 | 0 |
| C7 | 2 (4.76%) | 2 | 0 |
Relationship between sex and cervical vertebrae where the aberrant left VA enters through the transverse foramen.
Discussion
Variations of the aberrant VA origin have acquired great importance in the management of upper thoracic and neck trauma, as well as in the planning of vascular surgeries or endovascular interventions in this region. Furthermore, knowledge of the VA variants is important because despite they are asymptomatic, they could have clinical implications. Komiyama et al. 15 reported that 19.0% of the left VA that originated in the aortic arch developed arterial dissection of the same vessel, whereas only 1.1% of the left VA originating in the left SA presented this condition, arguing that the vessel with aberrant origin directly receives the pulsating force of the heart, in addition to the alteration of the hemodynamic resistance caused by the fatigue in the distal portion associated with vessel length.15 On the other hand, Inzunza et al. added that this condition also increases the risk of cerebrovascular events as a consequence of hemodynamic disturbances.16 Moreover, the fact that the prevertebral AV segment is longer implies that the trajectory and integrity of the vessel may be altered as it will be in touch with more anatomical structures, especially in the upper mediastinum.
In the present study, an origin of the VA different to the subclavian artery was observed in 8.6% (n = 43) of the cases, all unilateral, 8.4% (n = 42) of the left VA originating in the aortic arch, and 0.2% (n = 1) of the right VA originating in the right common carotid artery. The origin from the aortic arch of the left VA has been extensively described in the literature.4,15–19,22,23 The results obtained in the present study are similar to those previously reported by Muñoz, Herrera et al., and Sureka et al. in Chile, Colombia, and India, respectively, but significantly higher than those reported by Adachi and Kósla et al., whose studies included samples of similar size in Japanese and Polish populations, respectively (Table 4).4,6,16–19 The origin of the left VA from the aortic arch has been explained from the embryological point of view by a persistence of the sixth intersegmental artery, which maintains the connection with the longitudinal anastomosis.20,21 Regarding the aberrant origin of the right VA from the right common carotid artery, a prevalence of 0.18% have been reported,22,23 similar to what was observed in the present study (0.20%) (Fig. 1).
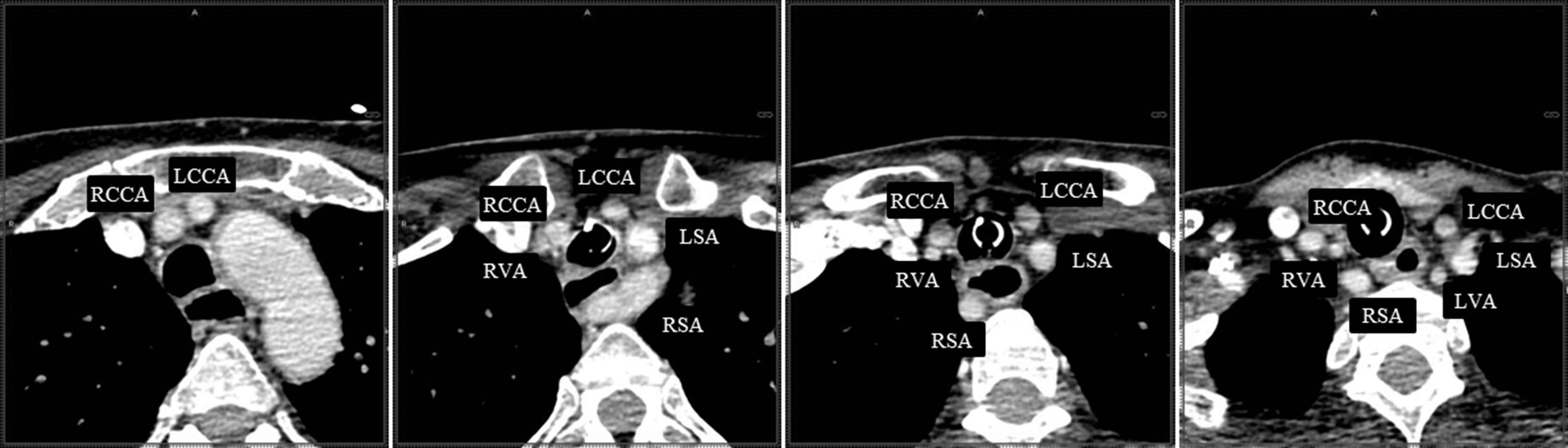
Axial CTA images where an aberrant origin of the right vertebral artery (RVA) from the right common carotid artery (RCCA) is observed. (LCCA: Left Common Carotid Artery; LSA: Left Subclavian Artery; RSA: Right Subclavian Artery; LVA: Left Vertebral Artery).
| Author | Publication Year | Country | Aberrant left AV origin from aortic arch | Sample |
|---|---|---|---|---|
| Adachi | 1928 | Japón | 5.4% | 516 cadavers |
| Muñoz | 1933 | Chile | 8.0% | 300 cadavers |
| Herrera et al.(7) | 2012 | Colombia | 8.2% | 122 cadavers |
| Tetiker et al.(5) | 2014 | Turkey | 3,8% | 79 CTA |
| Kósla et al.(14) | 2014 | Polonia | 5.5% | 110 CTA |
| Sureka et al.(4) | 2015 | India | 9.1% | 120 CTA |
| Estudio actual | 2016 | Colombia | 8.4% | 500 CTA |
Prevalence of aberrant left VA origin from aortic arch in different populations.
In relation to the intraforaminal entrance of the VA, in the 16.8% of cases (n = 84) the VA entered through a transverse foramen from different cervical vertebrae than C6, of which 90.48% (n = 76) was unilateral, whereas 9.52% (n = 8) had a bilateral presentation, 5.95% (n = 5) homogeneous and 3.57% (n = 3) heterogeneous (Fig. 2). The variation frequency was higher in man (17.40%) than female (15.23%), and in the left VA (10.6%, n = 53) than the right VA (7.8%, n = 39). Some studies have reported that left AV originating from the aortic arch often enter through a foramen other than C6, reporting values between 66.7% and 90.9% of the cases.6,22 In the present study, 80.95% (n = 34) of the left VA that originated in the aortic arch entered through a transverse foramen different from that of C6 (C3, 2.38%; C4, 7.14%; C5, 66.67%; C7, 4.76%).
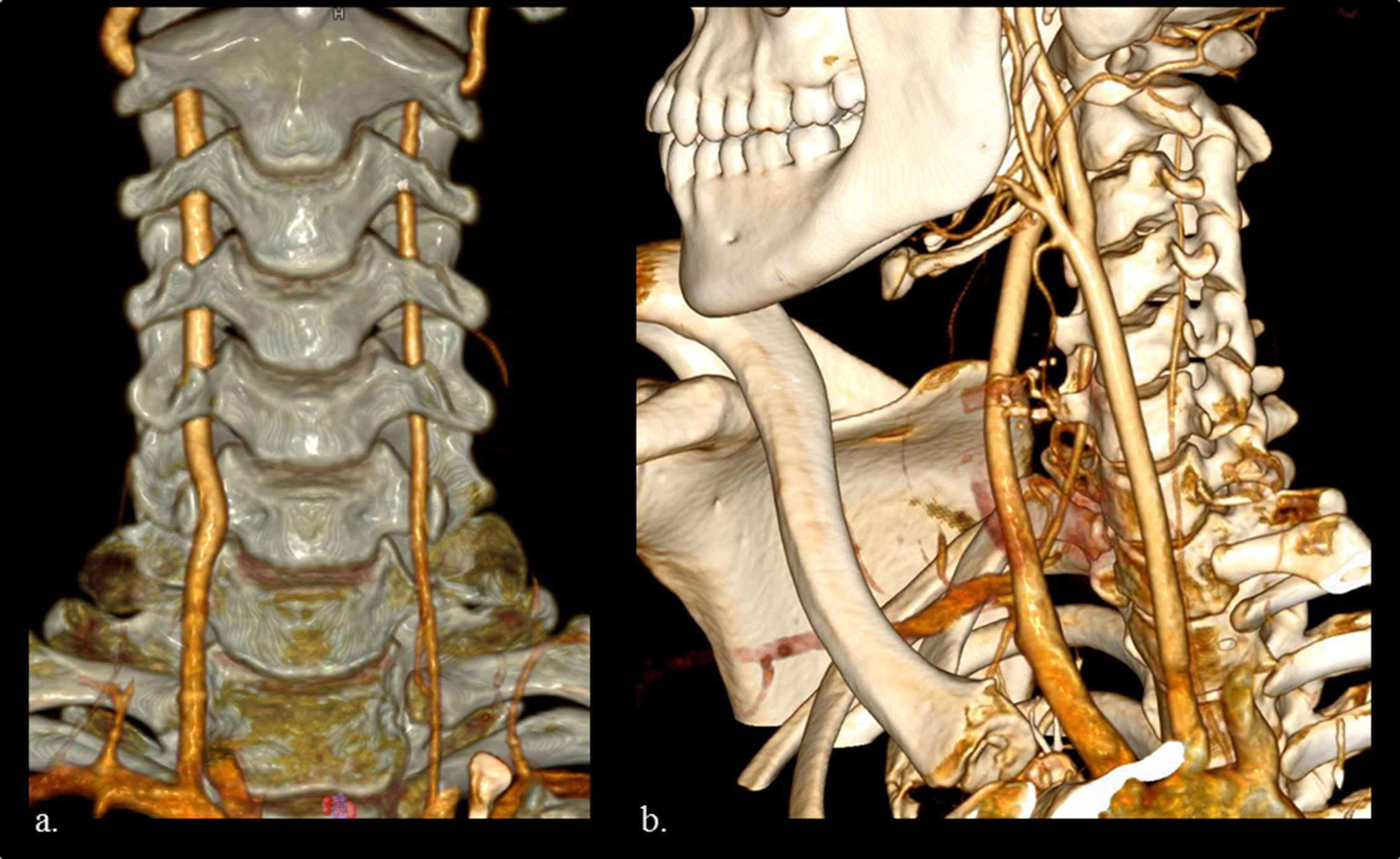
Volume Rendering Technique (VRT) images showing a bilateral homogeneus variation where both vertebral arteries enter through the transverse foramen of cervical vertebrae C5 (a); and an heterogeneous entrance where the right vertebral artery enters through the transverse foramen of C6 while the left vertebral artery enters through the transverse foramen of C4 (b).
Knowledge about intraforaminal entrance of the VA is important in surgical procedures where the approach is anterior to the cervical spine as any complication at this level associated with the VA may involve the cerebellum, brainstem, and spinal cord leading in severe neurologic deficits, infarction, loss of consciousness or central respiratory dysfunction.5,24 Moreover, the anomalous intraforaminal entrance of the VA may be associated with artery dissection not only as a result of neck manipulation or sudden movements but also induced by normal physiological motion.10,25
Conclusion
Considering the prevalence of VA variations in Colombian population, VA anatomy should be assessed prior to any surgical procedure in thoracic or neck region that involves these vessels as any complication may be deleterious for the patient. Furthermore, neurological symptoms in patients with AV variants regarding the origin or intraforaminal entrance, should be evaluated for arterial dissection. VA variants should be included in the radiology report as they may be useful for neurology clinicians not only for diagnostic purposes but also for preventive purposes.
Financial support
Authors declare no financial support for this research.
Ethical committee
This study was approved by Institutional Ethical Committee that does comply with the laws in Colombia.
Conflict of interests
None to declare.
Acknowledgements
This study was partially presented at the XII Colombian Congress of Morphology on October 2016 in Cali, Colombia where it was awarded as the Best Poster of Anatomical Variation. We want to thank the radiology department of the hospital Fundación Valle del Lili for facilitating the evaluation of the images that were used for this study.
References
Cite this article
TY - JOUR AU - Gloria Patricia Baena-Caldas AU - Juan Felipe Orejuela Zapata AU - Ana María Granados Sánchez PY - 2018 DA - 2018/08/03 TI - Anatomical characterization of the vertebral artery from a local study population using angiography by computed tomography JO - Artery Research SP - 39 EP - 43 VL - 23 IS - C SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2018.07.002 DO - 10.1016/j.artres.2018.07.002 ID - Baena-Caldas2018 ER -
