Depression in Rural Communities and Primary Care Clinics in Chiapas, Mexico
- DOI
- 10.2991/jegh.k.181128.001How to use a DOI?
- Keywords
- Chiapas; depression; Mexico; prevalence; rural
- Abstract
Depression is a leading cause of disability worldwide and can be diagnosed and treated in primary care clinics. No studies to date have demonstrated the prevalence of depression in rural, primary care settings in Mexico. The objective of this study is to describe the prevalence of visits for depression in primary care settings in one group of rural communities within Chiapas, Mexico. We performed a cross-sectional, retrospective study of depression prevalence in primary care clinics in the Sierra region of Chiapas, Mexico during the calendar year of 2014. We determined the average depression prevalence is 7.9% (6 community clinics, n = 4555). The prevalence of depression in rural Chiapas, Mexico is much higher than the Mexican national average of 4.0–4.5% found in a home-based survey. Further efforts to understand the causes, develop improved mental health services in primary care, and reduce the higher burden of depression in rural communities in Mexico are urgently needed.
- Copyright
- © 2019 Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Depressive disorders are the fifth leading cause of years lived with disability globally and were responsible for 1.84% of disability-adjusted life years in 2016 [1,2]. However, fewer than half of individuals suffering from depression worldwide receive any form of treatment [3]. Mental health historically has not received the same attention as communicable diseases and other chronic illnesses, and consequently, has also been under-researched [4]. Specifically, in resource-limited rural communities, lack of access to medical care has resulted in mental disorders going untreated. The World Health Organization (WHO) reports that an estimated 50% of patients suffering from depression do not receive treatment [3]. In Mexico, the delay in treatment for mood disorders is estimated to be as high as 14 years [5]. Nevertheless, depression can be both readily diagnosed and treated in primary care settings with existing tools. In a randomized trial of older adults, Gallo et al. [6] found that primary care-based interventions for depression reduced mortality. To emphasize the need for improvement, the WHO’s Mental Health Action Plan 2013–2020 set a global target goal of increasing service coverage for severe mental disorders, including moderate and severe depression, by 20% by 2020 [7]. In order to achieve this increase in coverage, it will be necessary to improve mental health related diagnosis and management in primary care, especially in rural and marginalized communities.
The Patient Health Questionnaire (PHQ) is an instrument used to make objective, criteria-based diagnoses of mental disorders commonly encountered in primary care [8]. The PHQ-9 is used to score each of the nine criteria in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-V) to assist in the diagnosis of depression, assess severity, and monitor response to treatment [8]. Lowe et al. [9] found the PHQ-9, administered by nurses and clinicians, to be a responsive and reliable tool to monitor treatment outcomes. Also, the Spanish version of the PHQ-9 has been demonstrated to be effective for primary care patients in Chile and for hospitalized patients in Spain [10,11]. The diagnostic accuracy of the Spanish version has been validated in the hospital setting to be comparable to the English version in primary care settings [12]. Arrieta et al. [13] have recently validated the Spanish version of the PHQ-9 for diagnosis of depression in rural Chiapas.
Chiapas is one the poorest and most marginalized states within Mexico. More than half of the state’s population lives below Mexico’s poverty line, and the population has a high burden of chronic illness [14,15]. National depression prevalence in Mexico is estimated to be 4.0–4.5% [16–18]. However, in rural Chiapas the rate may vary greatly from the national average owing to several socioeconomic factors such as the increased burden of poverty, financial stress, poor access to health services, and lack of economic and educational opportunities. Poverty begets additional risks for individuals to develop depression, and potentially serves as a synergistic factor to social and biological determinants of illness if appropriate medical interventions are not available [19]. As non-communicable chronic diseases and comorbidities account for an increasing portion of the burden of disease globally, it is paramount to accurately measure the prevalence of depression in addition to the burden of other chronic diseases [20]. Importantly, in a primary care setting, the estimation of prevalence of such chronic diseases has been shown to be an acceptable study method for measuring the burden in a specified population [21,22].
Depression prevalence in primary care has been shown to range from 6% to 13% with only one available study that evaluates depression prevalence in a low-resource, rural, primary care setting [23–25]. Although the prevalence of depressive symptoms has been studied in low-income women in rural communities, no studies to date have demonstrated the prevalence of depression in primary care settings for rural populations in Mexico [26]. Assessing depression in primary care settings is important because most patients first present to their general practitioner; unfortunately, access to comprehensive mental health services, such as psychiatry and psychology, is limited in many states in Mexico. For example, although the national ratio of psychiatrists to patients is 3.47/100,000 inhabitants and 18.86/100,000 in Mexico City, the ratio is a mere 0.54/100,000 in Chiapas, the second lowest ratio in the nation [27]. In 2008, less than one-third of the primary health care centers had protocols for evaluation and treatment of mental illness, and less than 15% of the providers had ever received continuing education on mental health [28]. As a middle-income country, Mexico has more than 3800 psychiatrists [27]. However, as the aforementioned numbers demonstrate, the majority of these providers work in urban centers such as the capital, Mexico City [27]. Indeed, significant economic and social disparity manifests in the distribution of specialists nationally.
Compañeros en Salud México (CES), an affiliate organization of the international nongovernmental organization Partners In Health (PIH), has made mental health an organizational priority. PIH has decades of experience providing healthcare in rural Chiapas and more than 4 years of experience administering 10 government clinics with a combined average of more than 30,000 patient visits per year. CES clinicians are given training on a continual basis in the diagnosis of and management of both common mental disorders, including depressive disorders, and severe mental disorders, such as psychotic illness. In addition, the organization conducts active case-finding activities in the communities with teams of physicians and medical students to help link patients with mental illness to available clinics.
The objective of this study is to describe the prevalence of depression in a primary care setting in rural communities in Chiapas, Mexico, through a cross-sectional, retrospective 1-year period prevalence chart review.
2. METHODS
This was a cross-sectional study aimed at determining the prevalence of depression in patients older than 18 years who presented for care at one of six CES-supported clinics. The study used data from the electronic medical record (EMR) system in the CES-supported clinics in the health jurisdictions of Villaflores and Motozintla. Institutional review board approval was given by Brigham and Women’s Hospital’s Partners Human Research Committee (Boston, MA, USA) and by Wright State University (Dayton, OH, USA). An in-country research committee also provided oversight and guidance.
A screen of the EMR was used to identify the number of patients 18 years and older seen by CES physicians between January 1, 2014 and December 31, 2014, and to tabulate baseline characteristics: sex, age, clinic utilization, social protection beneficiaries, diabetes, hypertension, and epilepsy. A separate screen was used to identify the total number of unique patients 18 years and older who were seen at CES clinics between January 1, 2014 and December 31, 2014 who received the diagnosis of depression by a physician. The presence of depression was confirmed by either a documented PHQ-9 score of 10 or greater, or documentation of five or more of the nine symptoms of depression for 2 weeks or greater per the DSM-V criteria in the physicians’ notes, along with a coded diagnosis of depression. The dataset was created by extracting deidentified variables: community, sex, age, PHQ-9 score, and depression diagnosis. The prevalence of depression and the associated 95% confidence interval were calculated for the entire sample and relevant subgroups. Odds ratios with 95% confidence intervals were calculated through logistic regression. All calculations were performed with deidentified patient data with the statistical software package, IBM SPSS Statistics, version 21.0 (IBM, Armonk, NY, USA).
3. RESULTS
A total of 4674 unique adult patients were seen at the six study clinics during the study time frame. Of these 4674 patients, 119 did not have complete demographic data recorded in the EMR and were excluded from analysis. The total number of adult patients who presented to the six clinics with depression during the calendar year of 2014 was 360 out of 4555 for an annual prevalence of 7.9%. Of the 360 patients with depression, 298 were female and 62 were male. Table 1 highlights baseline demographic and clinical characteristics of the study population. Female sex and patients aged 60–69 years were associated with a significantly higher risk of depression. The prevalence of hypertension was higher among patients with depression than among patients without depression (7.2% vs. 4.7%). Figure 1 shows the depression prevalence by sex (male = 3.9%, female = 10.1%) during the study period, and Figure 2 demonstrates the distribution of depression by age and sex. Depression prevalence peaked in females aged 50–59 years at 16.0%.
| Characteristic | All patients (n = 4555) | Depression (n = 360) | No depression (n = 4195) | Odds ratio (95% CI) | p-value |
|---|---|---|---|---|---|
| Sex | |||||
| Female, n (%) | 2958 (64.9) | 298 (82.8) | 2660 (63.4) | 2.77 (2.01–3.67) | <0.001 |
| Age (y) | |||||
| Mean, n (%) | 40.5 (±16.4) | 41.4 (±14.8) | 40.4 (±16.5) | – | 0.266 |
| 18–29 | 1436 (31.5) | 89 (24.7) | 1347 (32.1) | – | – |
| 30–39 | 1071 (23.5) | 93 (25.8) | 978 (23.3) | 0.97 (0.58–1.62) | 0.92 |
| 40–49 | 798 (17.5) | 73 (20.3) | 725 (17.3) | 1.4 (0.84–2.34) | 0.2 |
| 50–59 | 571 (12.5) | 62 (17.2) | 509 (12.1) | 1.48 (0.88–2.50) | 0.14 |
| 60–69 | 380 (8.3) | 24 (6.7) | 356 (8.5) | 1.80 (1.05–3.06) | 0.03 |
| ≥70 | 299 (6.6) | 19 (5.3) | 280 (6.7) | 0.99 (0.53–1.90) | 0.98 |
| Clinic utilization | |||||
| Mean number of visits | 2.5 (±2.3) | 4.4 (±3.2) | 2.3 (±2.2) | – | <0.001 |
| Social protection beneficiaries | |||||
| Seguro populara | 3750 | 298 | 3452 | 1.04 (0.78–1.38) | 0.82 |
| Prosperab | 2098 | 174 | 1915 | 1.11 (0.90–1.38) | 0.33 |
| Chronic diseases | |||||
| DM | 150 (3.3) | 18 (5.0) | 132 (3.1) | 1.62 (0.98–2.68) | 0.06 |
| HTN | 222 (4.9) | 26 (7.2) | 196 (4.7) | 1.56 (1.04–2.43) | 0.03 |
| Epilepsy | 57 (1.3) | 1 (0.3) | 56 (1.3) | 0.21 (0.03–1.49) | 0.08 |
Social Protection System in Health;
Conditional Cash Transfer Program;
CI, confidence interval; DM, diabetes mellitus; HTN, hypertension.
Baseline demographics and clinical characteristics of the study population
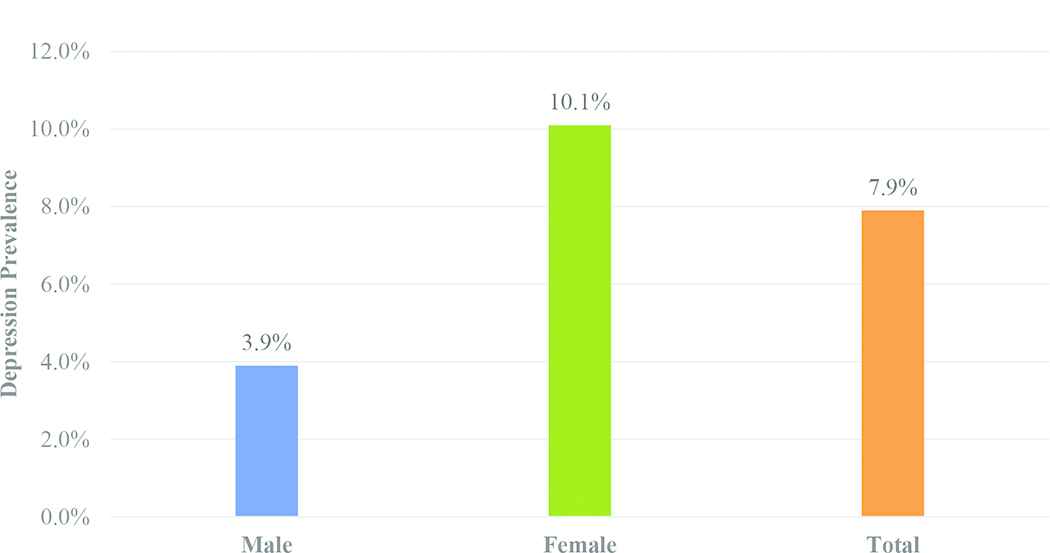
Depression prevalence by sex.
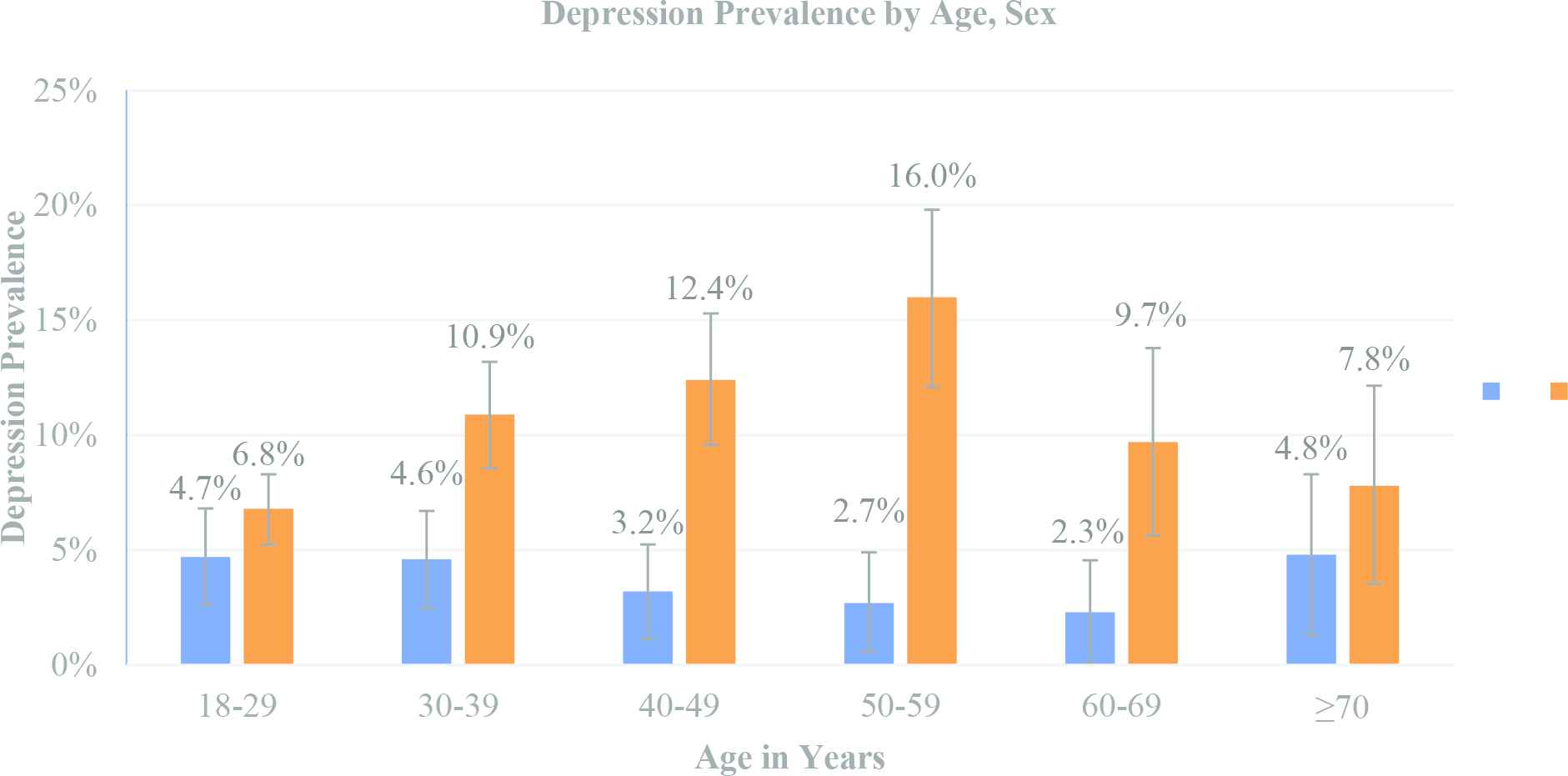
Distribution of depression by age and sex.
4. DISCUSSION
To the best of the authors’ knowledge, this is the first study to assess depression prevalence in rural primary care clinical settings in Mexico. This is relevant because more than one-fifth of the country’s population resides in rural communities [29]. Our study identified key determinants in depression prevalence based on geographic, sex, and age factors.
This study demonstrates Figure 1 an increased burden of depression prevalence in the six primary care clinics (7.9% vs. 4.5% nationally) [16–18]. It should be noted that the prevalence in a primary clinical care setting may be higher than the prevalence in a general population, because people who visit a primary care clinic will be diagnosed with depression. The paucity of economic opportunities and the geographical, political, and economic realities in the region may contribute to higher depression rates in the primary care clinics supported by CES in Chiapas.
The study results demonstrated a higher burden of depression among females (10.1%) than in males (3.9%) with a female/male ratio of 2.5:1. Although a lower rate of Mexican men seeking treatment has been reported elsewhere, there are important psychosocial, geographical, and sex-role factors to consider as contributing to the sex disparity [5]. Previous research shows females more quickly “translate nonspecific feelings of distress into conscious recognition that they have emotional problems” than males [30]. One possible contributing factor to the sex discrepancy is the ease of clinic access and utilization between males and females. In the study area, men work in the fields during the day, often more than an hour or farther away from the clinic, whereas women often work at home, closer to the clinic.
Our study also shows a higher percentage of depression in young to middle-aged adults compared to the general population Figure 2. Although depression in any age group can have devastating consequences, depression in young to middle-aged adults is particularly worrisome. The well-being of this age group is hindered by the “conditions of poverty, such as stress, increased negative life events, worse physical health, reduced access to health care and stigma,” which are all “thought to precipitate or maintain mental ill-health” during the most productive years [19].
Several limitations of the study were identified during the development of the study design and analysis. Local residents recognized the presence of increased therapeutic capabilities in the CES-administered clinics. As a result, there may have been a funneling effect of patients coming to our clinics preferentially over others, thus leading to increased rates of diagnosing disease in our clinics.
5. CONCLUSION
In this study, we report the period prevalence of depression during the calendar year of 2014 in six rural clinics in Chiapas, Mexico to be 7.9%. This rate of depression contrasts with the estimated national rate of 4.0–4.5%. Future studies are needed to better delineate the etiology of increased prevalence and low care-seeking behavior for depression. With appropriate training and ongoing supervision and support, as well as increased availability of medications and culturally sound nonpharmacologic treatments, there is ample evidence that depression can be diagnosed and treated in rural primary care clinics in Mexico. As a leading cause of disability worldwide, efforts to further understand the causes, to develop improved mental health services in primary care, and to reduce the higher burden of depression in rural communities in Mexico are urgently needed.
CONFLICTS OF INTEREST
None declared.
REFERENCES
Cite this article
TY - JOUR AU - Michael L. Elliott AU - Mercedes Aguerrebere AU - Patrick F. Elliott PY - 2019 DA - 2019/01/01 TI - Depression in Rural Communities and Primary Care Clinics in Chiapas, Mexico JO - Journal of Epidemiology and Global Health SP - 103 EP - 106 VL - 9 IS - 2 SN - 2210-6014 UR - https://doi.org/10.2991/jegh.k.181128.001 DO - 10.2991/jegh.k.181128.001 ID - Elliott2019 ER -
