Anaesthesia, surgery, obstetrics, and emergency care in Guyana
- DOI
- 10.1016/j.jegh.2014.08.003How to use a DOI?
- Keywords
- Anaesthesia; Surgery; Obstetrics; Emergency medicine; Global health; Guyana
- Abstract
The surgical and anaesthesia needs of low-income countries are mostly unknown due to the lack of data on surgical infrastructure and human resources. The goal of this study is to assess the surgical and anaesthesia capacity in Guyana.
A survey tool adapted from the WHO Tool for Situational Analysis to Assess Emergency and Essential Surgical Care was used to survey nine regional and district hospitals within the Ministry of Health system in Guyana.
In nine hospitals across Guyana, there were an average of 0.7 obstetricians/gynaecologists, 3.5 non-OB surgeons, and 1 anaesthesiologist per hospital. District and regional hospitals performed an annual total of 1520 and 10,340 surgical cases, respectively. All but 2 district hospitals reported the ability to perform surgery. An average hospital has two operating rooms; 6 out of 9 hospitals reported routine medication shortages, and 4 out of 9 hospitals reported routine water or electricity shortages. Amongst the three regional hospitals, 16.1% of pregnancies resulted in Caesarean section.
Surgical capacity varies by hospital type, with district hospitals having the least surgical capacity and surgical volume. District level hospitals routinely do not perform surgery due to lack of basic infrastructure and human resources.
- Copyright
- © 2014 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
1. Introduction
Recent estimates propose that as much as 28% of the global burden of disease comprise conditions that are potentially amenable to surgical intervention [1]. With this in mind, the role of surgery in public health can no longer be denied and emergency and essential surgical care must be included in basic healthcare in low- and middle-income countries (LMICs) [2].
This surgical and anaesthesia infrastructure survey was previously completed in Guatemala [3], Nicaragua [4], Bolivia [5], and Guyana. Guyana serves as the headquarters for the Caribbean Community (CARICOM). Therefore, this study in Guyana serves not only to elucidate the surgical capacity of a second South American country (after Bolivia), but also of the Caribbean, which is relatively less studied. This article aims to increase the knowledge base of surgical care in Latin America and enables initial comparisons to be drawn between nations in this region.
2. Background
Guyana is a low-middle-income country (LMIC) with a small population of approximately 750,000. Consistent with The World Bank description, 35% of the population of Guyana fall below the poverty line and has a GDP per capita of $8000 USD. Amongst those Guyanese with a tertiary level education, more than 80% have emigrated. Despite housing the headquarters for CARICOM, which is the largest and most powerful economic union in the Caribbean, there are economic and healthcare disparities. Overall WHO health indicators/statistics rank Guyana 128th in the world, with its total expenditure on health as a percentage of GDP as 5.9%. Statistics suggest an overall shortage of healthcare workers and access to medical services. Notably there are too few physician anaesthesiologists, obstetricians, and surgeons. The life expectancy at birth for both sexes in Guyana is 63 years, compared with a global average of 70 years [6]. The mortality rate under 5 years for both sexes is 36/1000, which is less than the global average of 51/1000. The birth rate (fertility rate) is 2.2/woman as compared with 2.4/woman globally. The Guyana Ministry of Health Maternal Morbidity and Mortality reduction campaign to investigate the root cause of the contributors to the high rate of maternal mortality started since the global average maternal mortality ratio is 210/100,000 live births as compared with Guyana’s maternal mortality ratio of 280/100,000 live births. Maternal Mortality is noteworthy as a Millennium Development Goal since 2000 [7]. The percentage of C-sections in Guyana – 16.5% – is higher than the recommended WHO rates of 5–10% [8] (Table 1).
| United States | Guyana | Bolivia | |
|---|---|---|---|
| Life expectancy at birth for both sexes (years) | 79 | 63 | 67 |
| Under 5 mortality rate (per 1000 live births) | 8 | 36 | 51 |
| Total fertility rate (per woman) | 2 | 2.2 | 3.3 |
| Maternal mortality ratio (per 100,000 live births) | 21 | 280 | 190 |
| Overall health system ranking | 37 | 128 | 126 |
World Health Organization health indicators.
2.1. Medical education
Guyana is home to three major centres for medical education: University of Guyana, American International School of Medicine, and Texila American University. Post-graduate education is limited; therefore, Guyanese physicians utilize options for medical training in countries such as Cuba and China. The pathway for Guyanese doctors into Cuban medical training is part of a Guyana government-funded programme to send medical students to Cuba. In addition, there is a sizable representation from the Cuban medical community working in Guyana on the Ministry of Health contracts. Cuban nationals working in Guyana are found in hospitals and health centres throughout the country. Government scholarships support this training and result in an obligatory government service in medical fields for a five-year period. Thereafter, trained physicians choose their site of practice with most practicing in urban areas.
External partnerships for post-graduate education and training in anaesthesia, surgery, obstetrics and emergency medicine are substantial and sustained within Guyana. The Canadian Association of General Surgeons assisted in developing a Diploma in Surgery to promote safe surgical practice [9]. Long-term academic relationships in Guyana have promoted the healthcare system and advancement of specialties, including Emergency Medicine, Surgery, and Obstetrics. Participating universities include McMaster University (Surgery and Paediatrics), Case Western University (Obstetrics) and Vanderbilt University (Emergency Medicine) [9–11]. Future goals include promoting Anaesthesiology from Vanderbilt University.
2.2. National hospital system
Guyana is divided into ten regions with the vast majority of the population density concentrated along the eastern two-thirds of the coast [12]. There are 30 Ministry of Health Hospitals, sub-divided as 6 regional hospitals and 24 district hospitals. Despite the small land area, Guyana comprises coastal plains, rainforest, and savannahs. The three most populous areas are Georgetown with a population of 235,017 (Georgetown Public Hospital Corporation), Linden with a population of 44,690 (Linden Hospital), and New Amsterdam with a population of 35,039 (New Amsterdam Hospital). The aforementioned cities are home to the most comprehensive regional hospitals and house a majority of the surgical infrastructure. Trauma – from road traffic accidents and violence – is the most common surgical presentation. Because of a lack of obstetricians, obstructed labour and other maternal sequelae are expectantly managed without surgery whenever possible. When surgical intervention is required, medical evacuation by fixed wing aircraft is provided by the military or by the volunteer Pilots Association [13].
2.3. Access and availability of facilities
Most of the population within Guyana, about 663,000 people, have access to medical care due to the concentration of population in urban areas. The rural populations are served by district hospitals where the services are limited and distances travelled for care are greater and/or more challenging due to lack of transportation infrastructure. Non-emergent care not available at the district hospital requires a referral to the capital or regional hospitals. This care is limited by distance, transportation, and expense. The average Guyanese living in the rural areas cannot afford to travel for their medical care.
Emergency care at the district hospital is very limited since stabilization typically refers to placing a peripheral intravenous catheter and transporting the patient to a referral hospital. Most district hospitals are without endotracheal and thoracostomy tubes and may not have functional defibrillators.
2.4. In-country medical transport
While there are efforts underway to pull together various public and private assets into a coordinated Emergency Medical System under a proposed Guyana National Ambulance Authority, access to medical transportation remains extremely limited. Ground ambulances, which are generally based at individual hospitals and often staffed with untrained attendants, are generally tasked with inter-facility transfers. Ambulance response to the scene of accidents is haphazard at best and not yet supported by an integrated communication or dispatch system. The development of training for Emergency Medical Technicians is in its infancy, with the first 22 basic EMTs completing training in February of 2014.
The development of an effective EMS system to support access to timely emergency surgical care is severely challenged by Guyana’s geography. Only a small percentage of the country’s nearly 200,000 square kilometres are accessible by road, resulting in a regular need for aeromedical evacuation from interior locations. This need is currently met by a combination of public and private efforts. At times, the government of Guyana may absorb the cost of a medical evacuation flight, either utilizing military aircraft or contracting with private aircraft. In addition, the national Aircraft Owner’s Association (AOA) operates under its own “longstanding policy of evacuating any sick or injured person free of charge on their aircraft”, with over 100 such evacuations reported in 2011 [13].
2.5. Pharmaceuticals and equipment
The Ministry of Health reports the availability of all medicines on the WHO Essential Medicine list. Guyana has a single distributor of pharmaceuticals–The Materials and Management Unit (MMU) based in Georgetown. Throughout the country, there are chronic shortages of intravenous antibiotics, anti-hypertensive medications, and oral hypoglycaemic (diabetic) medications. Oral analgesia medications are largely available as is injectable (IV) morphine. The same distributor, MMU, is responsible for the allocation and distribution of medical equipment.
University trained pharmacists are available at the regional hospitals. However, district hospitals typically have pharmacy technicians. Biomedical engineers work for Meditron©, the only biomedical engineering company in Guyana. Meditron© is a small private company which services the whole country, thus wait time for servicing and repair of equipment is frequently prolonged. Biomedical technicians are available at GPHC, but repair and servicing are limited in part by lack of training and the inability to access service manuals and spare parts, especially for donated equipment.
3. Methods
Following Vanderbilt University Medical Center IRB approval and approval from the Guyanese Ministry of Health, a systematic survey of 9 hospitals was conducted utilizing the survey tool originally designed by the Harvard Humanitarian Initiative, adapted from the WHO GIEESC situational analysis tool (Appendix A). Because of the unusually small and geographically concentrated population base of Guyana, the major regional hospitals and representative district hospitals were visited and surveyed. The situational analysis tool was adapted to Guyana by addressing all of the applicable points (Appendix A, NGO = non-governmental organization).
4. Results
The survey was completed in 9 district and regional hospitals in Guyana (Fig. 1). Emergency and essential surgery is performed at the regional hospitals in urban areas representing 3 of the 9 hospitals surveyed. In addition, cardiac surgery is available at GPHC, vascular surgery at New Amsterdam, and major orthopaedic and trauma surgery at GPHC, Linden, and New Amsterdam. While four district hospitals are reported to perform surgery, the hospitals surveyed did not routinely operate and no district hospitals had the capability to perform emergency surgery. Basic resuscitation and stabilization are available at the district hospitals, but patients requiring further intervention are routinely transferred to a higher level of care facility. Several district hospitals accepted surgical mission teams who provided the equipment and human resources required.
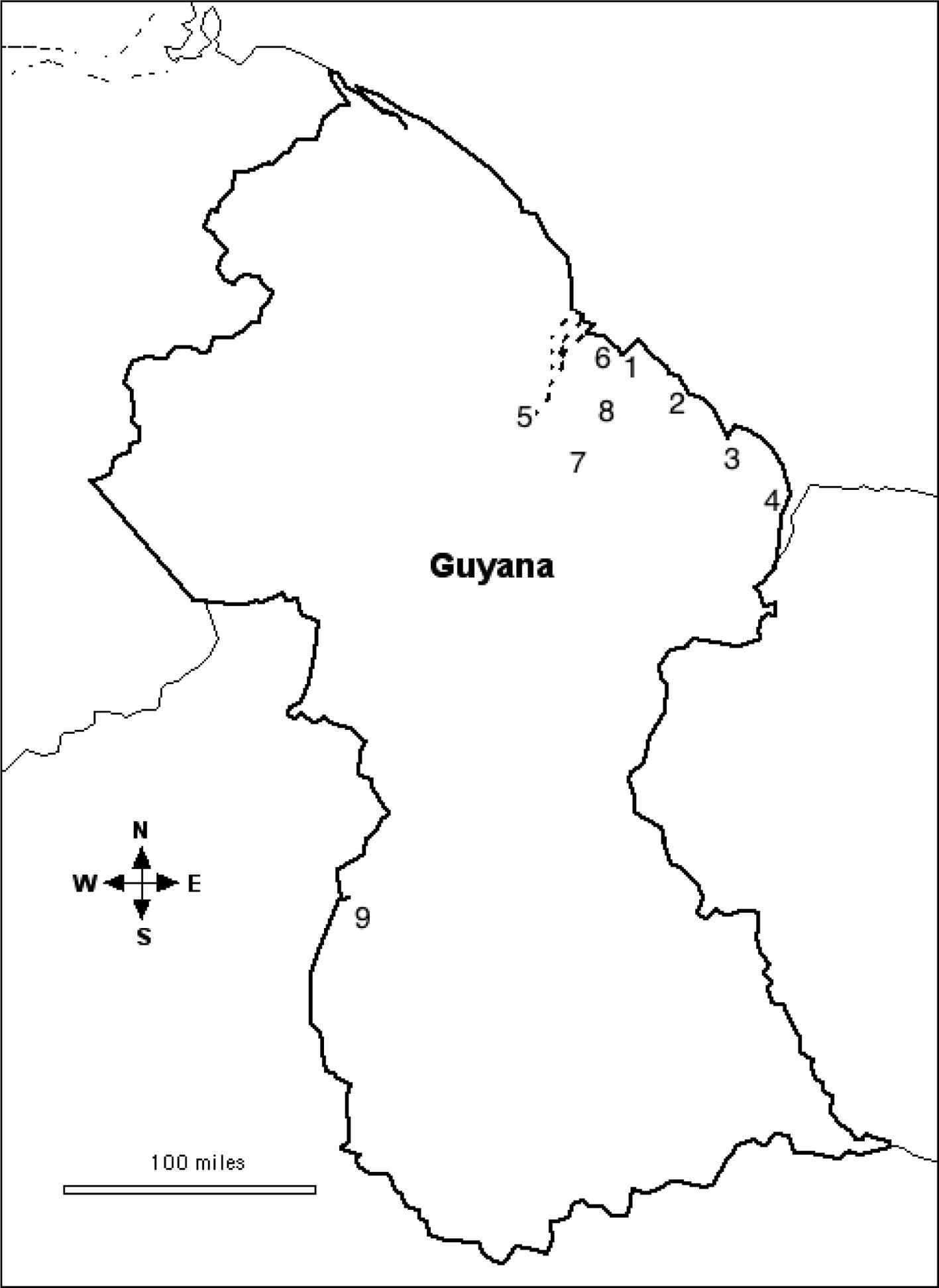
Hospital key. 1. Georgetown public hospital corporation. 2. Mahaicony district hospital. 3. New Amsterdam regional hospital. 4. Skeldon district hospital. 5. Bartica district hospital. 6. West Demerara district hospital. 7. Linden regional hospital. 8. Diamond-East Demerara district hospital. 9. Lethem district hospital.
4.1. Access and availability of facilities
The mean catchment population between hospitals was 136,889 (Table 2), but with a range of 5000–740,000. The average number of hospital beds and operating rooms (OR) per hospital is highly variable (Table 2). There is 1 OR per 43,142 people within a district hospital’s catchment and 1 OR per 62,500 people within a regional referral hospital’s catchment. On average there is 1 OR per 38,947 people in Guyana. Patients travel 60 km, on average, to reach a hospital. Travel may consist of a boat ride and several days of travel.
| District hospitals (6) | Regional hospitals (3) | |
|---|---|---|
| Catchment population | 50,333 | 310,000 |
| Estimated average distance traveled to reach hospital (km) | 36.3 | 110 |
| Number of beds per hospitals | 49 | 247 |
| Number of ORs per hospital | 1.1 | 4 |
| Total physicians | 6 | 24 |
| Anaesthesiologists | 0.2 | 2.6 |
| OB/GYNs | 0.3 | 9.6 |
| Surgeons | 0.3 | 1.6 |
| General medical officers (GMOs) | 9.8 | 102 |
| Nurses | 41.6 | 190.6 |
| Auxiliary nurses | 8.1 | 101.6 |
| Anaesthesia techs | 1 | 2 |
| Pharmacists | 1.8 | 7.3 |
| Midwives | 6 | 33.3 |
| Pharmacy techs | 4 | 12 |
| Total operations | 1520 | 10,340 |
| Emergency operationsa | 85 | 3370 |
| General surgeries | 630 | 1903 |
| Paediatric surgeries | 38 | 508 |
| OB/GYN surgeries (included C-section) | 588 | 2216 |
| Other specialty surgeries | 179 | 2343 |
| Presence of autoclaves | 5 | 3 |
| Presence of pulse oximetry in the ORs | 6 | 3 |
| Ability to track health outcomes | 3 | 3 |
| Ability to track surgical site infections and adverse drug reactions | 0 | 3 |
| Ability to track antibiotic resistance | 0 | 0 |
| Ability to track post-anaesthesia complications | 0 | 1 |
Emergency and urgent surgery necessitates an operation within 6 h.
Human resources, access and availability, and surgical volume at hospitals surveyed (by hospital type) (all values are the mean).
4.2. Access to human resources
There has never been an Anaesthesia Society in Guyana. There are 5 physician anaesthesiologists in Guyana, 4 at GPHC and 1 at a private hospital. There are 3 visiting physician anaesthesiologists in Guyana for 2 years via a government to government arrangement, which consists of 1 at GPHC and 2 at regional hospitals. There are 17 nurse anaesthetists in Guyana, 8 at GPHC, 2 at private hospitals, and 7 at district and regional hospitals (Table 2). There are 3 major curriculae for anaesthesia training at GPHC: Diploma in Nurse Anaesthesia (2 years), Diploma in Anaesthesia and Intensive Care (2 years), and Master of Medicine in Anaesthesia and Intensive Care (4 years).
4.3. Equipment and infrastructure
Every hospital surveyed had ORs, functional bathrooms, and sterilization capacity. All of the ORs providing surgical services have pulse oximetry, but pulse oximetry in the recovery area (PACU) and/or ICU is not guaranteed. Improvement in patient safety and monitoring could be made with the addition of portable pulse oximetry (Table 2).
4.4. Operative data
The total case volume in the hospitals surveyed was 11,860 annually. The mean number of cases per hospital was 3447 annually at regional referral hospitals. Six of the 9 hospitals surveyed routinely collect operative data. Amongst the cases reported, 32.1% of cases were classified as urgent or emergent (necessitating surgery within 6 h), 21.3% were classified as non-emergent general (adult, not sub-specialty) surgical, 4.6% of cases were paediatric, 23.6% were obstetric, and 18.4% were sub-specialties, including orthopaedic, ENT, vascular, and ophthalmic cases.
The regional hospitals surveyed collected Caesarean section rates. Within these 3 hospitals, the average percentage of births that resulted in Caesarean section was 16.1%.
4.5. Outcomes data
The ability to track outcome data varied greatly amongst the surveyed hospitals (Table 2). Of the 4 district hospitals providing surgical outreach (via visiting surgeons), 2 hospitals reported no operative deaths in the past year, 1 hospital reported 1 operative death in the past year (case fatality rate = 0.001%), and 1 hospital could not report the operative deaths indicating that the records were kept by the surgical mission team. Of the 3 regional hospitals, 1 reported no operative deaths, 1 reported 2 operative deaths and 1 post-operative death, and 1 reported 3 operative deaths and 1 immediate post-operative death. None of the regional hospitals reported deaths within 24 h of surgery or anaesthesia.
5. Discussion
This survey of 9 hospitals in Guyana reveals limits in the provision of emergency surgery and challenges in anaesthesia safety similar to situations documented in other countries by these surveys. The unique attributes of surgical care in Guyana include the absence of surgery at the district hospital level and the range of surgical services provided at the regional facilities, including a relatively high caesarean section rate.
5.1. Surgery and safe anaesthesia
Similar to many hospital systems in LMICs, Guyana functions with district hospitals and regional referral hospitals. The WHO recommends that district hospitals provide emergency surgery to optimize outcomes [14], but few district hospitals in Guyana are capable of providing these services. The contribution of trauma and maternal conditions to overall morbidity and mortality will only be improved when safe anaesthesia and emergency surgery are immediately available at the point of first patient contact. The geography of Guyana poses unique challenges for transportation and transfer of patients from rural areas to the urban regional facilities. While a smaller percentage of the population resides in these areas, the role of the district hospital in Guyana cannot be diminished. As predicted by other surveys, the regional hospitals have the most robust surgical capability. However, this survey reveals deficiencies at this level as well. Therefore, improvements in surgical infrastructure and anaesthesia must be prioritized throughout the system with support from the Ministry of Heath for overall improvement in population health in Guyana. Tracking of perioperative mortality rates will similarly improve anaesthesia and surgical outcomes and should be collected, reported, and compared with other countries in the WHO Americas region [15].
5.2. Equipment and patient safety
Consistent with observations in many LMICs, biomedical engineers are rarely trained or professionally supported. There are no formal structured biomedical engineering training courses available in Guyana. The only biomedical engineering company is Meditron© which trains and employs staff to maintain biomedical equipment. GPHC also trains staff with an electronics background to work as biomedical technicians. GPHC will also contract with several biomedical equipment vendors in the region whose technicians come from Trinidad or elsewhere as needed. These informally trained technicians form the backbone of the services of the biomedical department at the hospital. Thus, there is some competition with Meditron©, since they serve GPHC and other public hospitals, managing less complex equipment and those hospitals that do not have service contracts. Broken and dysfunctional medical equipment is common in LMICs. Approximately half of the anaesthesia machines outside of GPHC, Linden, and New Amsterdam have malfunctioning components. Approximately half of the ventilators outside of GPHC in the ICU or Emergency Department have malfunctioning components. None of the hospitals outside of GPHC and New Amsterdam had a functioning laboratory machine to obtain serum electrolytes.
Data from 54 LMICs worldwide found that approximately 77,700 ORs are not equipped with pulse oximetry [16], and yet surgery continues. Companies such as LifeBox© are addressing this problem, and have made a pulse oximeter for a retail cost of around $250 USD. Other low-tech, durable solutions are urgently needed in these settings to ensure safety.
5.3. World Health Organization Americas regional comparison
Comparisons can be made between Guyana and other LMICs in the WHO Americas region where this survey has been completed [6]. Nicaragua has 580 OB/GYN, 1040 non-OB/GYN surgeons, and 250 anaesthesiologists [4]. Nicaragua’s national referral hospitals perform 7776 surgeries annually and all but six (out of 28 surveyed) of their primary hospitals provide surgical services. Guatemala, by comparison, provided surgical services at 21 (out of 22 surveyed) hospitals with an average of 6.7 OB/GYN, 7.8 non-OB/GYN surgeons, and 3.8 anaesthesiologists per hospital and performed 4305 surgeries annually at their national referral hospitals [3]. Bolivia, a country in South America, has 1270 OB/GYN, 1807 surgeons, and 500 anaesthesiologists, thus placing a large anaesthesia burden on the country [5]. Basic and general hospitals in Bolivia performed an average of 730 and 2858 operations per year, respectively [5]. Although comparisons can be made between LMICs in similar WHO regions, population differences of Nicaragua (8 times larger), Guatemala (20 times larger), and Bolivia (14 times larger) make Guyana unique in assessing the deficiencies to provide safe surgical and anaesthetic care.
6. Conclusion
Surgery is essential to healthcare systems and public health [17]. Emergency and essential surgery and safe anaesthesia are not adequately available to address the surgical and trauma burden, and the countrywide goals are to decrease the maternal mortality rate in Guyana. Additional factors limiting safe anaesthesia and surgical care include equipment, essential medications and blood products. Unlike many LMICs, Guyana is also working to improve pre-hospital care through developing and improving the EMS. This has the potential to impact trauma and maternal outcomes, both in the urban areas and the vast rural areas. Bolstering the surgical training at GPHC and encouraging Guyanese physicians to stay in Guyana will improve Guyana’s surgical capacity. With sustained external support to build important medical specialties, Guyana is poised to improve anaesthesia, surgical safety, improve outcomes, and become a model for healthcare in Latin America.
Competing interests
No external funding and no competing interests declared.
Acknowledgment
Mrs. Melissa Rockliffe-Glen, Georgetown Public Hospital Corporation.
Appendix A. Survey tool
Department:
Hospital name:
Level of hospital (Departmental/Regional/National):
Section A: Access and Availability
- 1.
Hospital capacity
- 2.
Population served (catchment area)
- 3.
Avg distance traveled to reach hospital
- 4.
Total number of hospital beds
- 5.
Total number of ORs
Section B: Access to Human Resources
- 1.
# of Physicians
- 2.
# of Surgeons
- 3.
# of Ob/Gyns
- 4.
# of other surgeons (non-MD)
- 5.
# of Anaesthesiologists
- 6.
# of Anaesthesia Techs
- 7.
# of Nurses
- 8.
# of Auxiliary Nurses
- 9.
# of Midwives
- 10.
# of Pharmacists
- 11.
# of Pharmacy Techs
Section C: Infrastructure
- 1.
Water: [Y/N] [always/often/infrequently/never available]
- 2.
Electricity: [Y/N] [always/often/infrequently/never available] [hardwire/generator/both]
- 3.
General sanitation: [Y/N]
- 4.
Sterilization of instruments: [Y/N]
- 5.
List autoclave or type of equipment:
- 6.
Sterilization of operating rooms: [Y/N]
- 7.
Sterilization of toilet facilities: [Y/N]
- 8.
Blood products: [Y/N]
- 9.
Types of products available:
- 10.
In-house blood bank: [Y/N]
- 11.
Red Cross blood bank: [Y/N]
- 12.
Living blood bank (donors): [Y/N]
- 13.
Oxygen source: [Y/N] [cylinder/piped/concentrator/other]
Section D: OR Information and Procedures
- 1.
# of OR Cases Per Year
- 2.
# of Emergency Surgical Cases
- 3.
# of General Surgical Cases
- 4.
# of Paediatric Surgical Cases
- 5.
# of Ob/Gyn Surgical Cases
- 6.
C-section rate
Section E: Outcomes
- 1.
Is there capacity to measure outcomes? [Y/N]
- 2.
Are OR deaths measured or tracked? [Y/N]
- 3.
Are OR deaths investigated as to cause? [Y/N]
- 4.
# of Deaths due to surgery while in OR: If known, cause of death
- 5.
# of Deaths due to surgery immediately post-op: If known, cause of death
- 6.
# of Deaths due to anaesthesia immediately post-op: If known, cause of death
- 7.
# of Deaths due to surgery in the first 24 h: If known, cause of death
- 8.
# of Deaths due to anaesthesia in the first 24 h: If known, cause of death
- 9.
Capacity to track adverse drug reactions: [Y/N] If yes, give #
- 10.
Capacity to track surgical infections: [Y/N] If yes, give #
- 11.
Antibiotics Resistance: [Y/N] If yes, give #
Section F: Equipment
- 1.
Oxygen supply in each operating location: [Y/N]
- 2.
Pulse oximeter in each OR: [Y/N]
- 3.
Pulse oximeter in each post-op area: [Y/N]
- 4.
Soap dispensers available: [Y/N]
- 5.
Sutures available: [Y/N]
- 6.
Quality of sutures:
- 7.
Availability of culture media: [Y/N]
- 8.
Air conditioning in ORs: [Y/N]
Section G: NGO Delivery of Surgical Services
- 1.
Surgical NGOs: [Y/N]
- 2.
Short-term Surgical Missions: [Y/N]
- 3.
Mission Hospital Providing Surgery: [Y/N]
Section H: Pharmaceuticals
- 1.
Access to essential medicines: [Y/N]
- 2.
Routine shortage of medications: [Y/N]
- 3.
Access to Antibiotics: [Y/N]
- 4.
Access to Narcotics: [Y/N]
- 5.
Access to non-narcotic pain medicines: [Y/N]
- 6.
Refrigeration of medicines: [Y/N]
- 7.
Where do inpatients get medicines? (In-house pharmacy, purchase before, etc.)
- 8.
Custom formulary: [Y/N]
References
Cite this article
TY - JOUR AU - H.J. Vansell AU - J.J. Schlesinger AU - A. Harvey AU - J.P. Rohde AU - S. Persaud AU - K.A. McQueen PY - 2014 DA - 2014/10/07 TI - Anaesthesia, surgery, obstetrics, and emergency care in Guyana JO - Journal of Epidemiology and Global Health SP - 75 EP - 83 VL - 5 IS - 1 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2014.08.003 DO - 10.1016/j.jegh.2014.08.003 ID - Vansell2014 ER -
