Marked regional variations in the prevalence of sickle cell disease and β-thalassemia in Saudi Arabia: Findings from the premarital screening and genetic counseling program
- DOI
- 10.1016/j.jegh.2011.06.002How to use a DOI?
- Keywords
- Genetic testing; Hemoglobinopathies; Premarital screening; Epidemiology; Saudi Arabia
- Abstract
Background: Hemoglobinopathies represent a major public health problem in Saudi Arabia (SA). Reports suggest that their higher prevalence is not evenly distributed in SA. Regional differences were studied in sickle cell disease and β-thalassemia and their at-risk marriages using national data.
Methods: The carrier and case status of sickle cell disease and β-thalassemia were determined in couples approaching marriage between 2004 and 2009 using standard blood tests. Prevalence of both diseases and at-risk marriages in different SA administrative and geographical regions were calculated and compared.
Results: A total of 15,72,140 men and women were examined over 6 years. This represented 0.06% of the entire population of Saudi Arabia. The prevalence of couples who tested positive for sickle cell was 45.1 (42.4 for carriers and 2.7 for cases) per 1000 persons examined. The prevalence was highest in the Eastern region (134.1 per 1000), followed by Southern and Western regions (55.6 and 28.5 per 1000, respectively) and lowest in Central and Northern regions (13.7 and 13.5 per 1000, respectively). The prevalence of couples testing positive for β-thalassemia was 18.5 (18.0 for carriers and 0.5 for cases) per 1000 persons examined. The prevalence was highest in the Eastern region (59.0), moderate in the Southern, Western and Central regions (14.2, 10.2, and 10.1 per 1000, respectively) and lowest in the Northern region (3.9).
Conclusion: Vast regional differences in hemoglobinopathies among adult Saudis are being reported that may help policy makers better allocate resources of available preventive programs.
- Copyright
- © 2011 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/)
1. Introduction
Hemoglobinopathies are among the most commonly inherited genetic disorders in humans. The World Health Organization (WHO) estimated that at least 5% of the world’s population are genetic carriers for hemoglobinopathies (2.9% for thalassemia and 2.3% for sickle cell disease). Sickle cell disease is found predominantly in Africa and the Middle East, while β-thalassemia is predominant in Asia, the Mediterranean basin, and the Middle East [1]. Sickle cell disease and β-thalassemia represent a major public health problem in Saudi Arabia (SA) [2]. Both diseases can be cured by bone marrow transplantation; however, curative treatment is costly and unavailable except for a limited number of cases. As a result, both diseases carry with them huge economic and psychological burdens on the patient and the society. As a consequence, premarital screening and genetic counseling (PMS&GC) was mandated in SA in 2004 [3]. The main program objective was to reduce the prevalence of sickle cell disease and β-thalassemia by reducing the number of at-risk marriages. All couples with marriage proposals have to be tested for both diseases and get the appropriate counseling (if required) before consummating their marriage. The PMS&GC program was spread over five geographic regions (Central, Eastern, Western, Northern and Southern) and 13 administrative regions in order to cover the entire country. The Saudi population was 22.7 million at the start of the program in 2004 and it reached 25.4 million by 2009; the population covered by the PMS&GC program was limited to those individuals seeking marriage.
Prevalence studies published before [4–10] and after [11–16] the PMS&GC program suggested that the higher prevalence of sickle cell disease and β-thalassemia are not evenly distributed in SA. With the exception of a few studies [10,12,13], most studies covered only isolated regions in SA. Comparing prevalence from the majority of these studies is difficult because of inconsistency of study design, differences in laboratory techniques, diversity of the covered population (neonatal, children, adults), variability of studied years (pre- or post-PMS&GC program), and differences in sample power. The scope of this study is focused on regional differences in the prevalence of sickle cell disease and thalassemia, as well as the frequency of at-risk marriages using 6 years of national data from the PMS&GC program.
2. Methods
2.1. Population and geography
The PMS&GC program covered the entire Saudi population. Geographically, SA consists of 13 administrative regions, 20 Ministry of Health regions (after subdividing some administrative regions), or five geographic regions (Central, Eastern, Western, Northern and Southern).
2.2. The Saudi PMS&GC program
The program was stipulated by law in December 2003 and implemented in February 2004. The program infrastructure consisted of 150 health care reception clinics, 70 laboratories, and 78 genetic counseling clinics covering the 13 administrative regions across the country. All couples tested between 2004 and 2009 were included in the analysis.
According to the program guidelines, couples with marriage proposals had to report to the nearest health care clinic to apply for premarital certificates. At the health care clinics, the program staff collected basic demographic information, took blood samples (in EDTA anticoagulant), and offered educational materials about the program to the couples who applied. The blood samples were then sent to the designated laboratory for testing for sickle cell disease and thalassemia using hemoglobin (Hb) electrophoresis. Other blood tests done included: complete blood count, peripheral blood film, reticulocyte count, and sickling test. The diagnosis of β-thalassemia trait was established when Hb A2 was above 3.5% with low MCV in absence of Iron deficiency anemia. The diagnosis of alpha thalassemia was not included in the program due to its low clinical significance in most of the cases. In order to establish the diagnosis of sickle cell trait, the test must show the presence of Hb S with positive sickling. The results were interpreted according to standard laboratory diagnostic protocols [11,17].
Test results were shared with the examined couples before issuing the premarital compatibility certificates. The test results categorized each member of the potential couple as: free (healthy), carriers (carrying the trait) and cases (having the disease) as regards the genetic make-up of sickle cell disease and/or β-thalassemia. Safe marriages were declared when both or at least one member of the couple was healthy. At-risk marriages were declared when both members of the couple were carriers or cases (or one was a case and the other was a carrier) of sickle cell disease and/or β-thalassemia. Couples with safe marriage test results were issued instant compatibility certificates while at-risk couples were asked to attend personal genetic counseling meetings before issuing incompatibility certificates.
2.3. Data analysis
It was the health care clinics’ responsibility (N = 150) to collect and manage their own local laboratory data. Each of the 20 health regions were required to collect data from their respective health care clinics and fax standard monthly reports to the Directorate General of Non-Communicable Diseases of the Ministry of Health in Riyadh. The aggregate data collected from the reports were used to construct a central database that was used for the current analysis. The prevalence of carriers and cases of sickle cell disease and/or β-thalassemia were expressed per 1000 examined persons. The frequency of at-risk marriages was expressed per 1000 examined persons and per 100 positive results. Carrier–case ratio was defined as the ratio of carriers to cases among those who had any positive results for sickle cell disease and/or thalassemia. Prevalence of both diseases and at-risk marriages in different SA administrative and geographical regions were calculated and compared. Significant regional differences in prevalence and ratios were tested using Chi Square. All P-values were two-tailed. P-value <0.05 was considered as significant. OpenEpi (version 2.2, Atlanta, GA, USA) and Microsoft Office excel (2003) were used for all statistical analyses.
3. Results
A total of 15,72,140 men and women examined between 2004 and 2009 were included and analyzed. The average number of men and women examined in the PMS&GC program was 262,000 annually (ranged between 242,000 in 2004 and 296,000 in 2009). This represented an annual frequency of 10.9 marriage proposals per 1000 Saudis.
Out of 15,72,140 men and women examined, 70,962 (4.5%) tested positive for sickle cell gene (66,649 carriers and 4313 cases) (Table 1). The prevalence of the sickle cell gene was 45.1 (42.4 for carriers and 2.7 for cases) per 1000 examined persons. The prevalence was highest in the Eastern region (134.1), followed by Southern and Western regions (55.6 and 28.5, respectively) and lowest in Central and Northern regions (13.7 and 13.5, respectively) (Fig. 1). The highest prevalence of the sickle cell gene per 1000 examined persons in SA was seen in two administrative regions (Fig. 2A): the Eastern region (134.1) and Jazzan (126.6). However, four administrative regions (Qassim, Hail, Jouf, and Northern borders) demonstrated the lowest prevalence of sickle cell disease at below 5 per 1000 examined persons. The remaining administrative regions demonstrated the sickle cell disease prevalence between 14.4 and 36.0 per 1000 examined persons. There were considerable variations in the sickle cell disease prevalence within the same administrative or geographic regions. For example, sickle cell disease prevalence in Qunfudah (135.7) was significantly higher than its administrative (Makkah: 30.3) or geographic (Western: 28.5) regions. On the other hand, the sickle cell disease prevalence in Hafr Albaten (4.4) was significantly lower than other health regions of the Eastern region (Ahsa:, 183.4; Eastern region including Dammam: 128.2; overall: 134.1). The overall carrier–case ratio for sickle cell disease was 15.5 with considerable regional variations being highest in the Western region (33.9) and lowest in the Northern region (8.5) (Fig. 2).

Prevalence of sickle cell disease and β-thalassemia and frequency of at-risk marriages among examined persons in the PMS&GC program between 2004 and 2009 by geographic regions of Saudi Arabia.
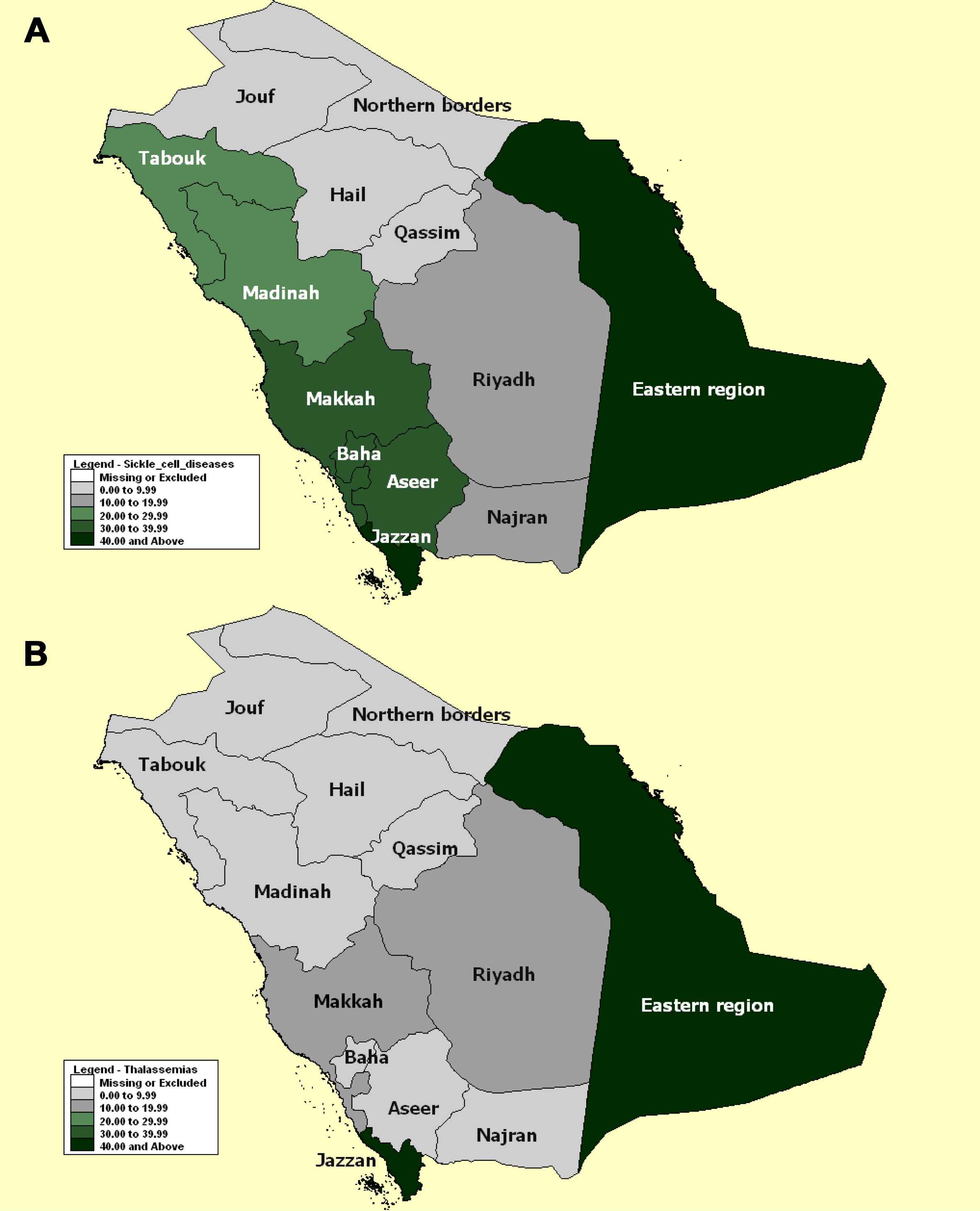
Annual prevalence of total sickle cell disease (A, above) and thalassemia (B, below) among examined persons in the PMS&GC program between 2004 and 2009 by administrative regions of Saudi Arabia.
| Examined persons | Genetic testing | Sickle cell disease | β-Thalassemia | At-risk marriages | Prevalence of positives per 1000 examined persons | Prevalence of sickle cell disease per 1000 examined persons | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Positives | Negatives | Carriers | Cases | Total | Carriers | Cases | Total | Carriers | Cases | Total | ||||
| Administrative regions: | ||||||||||||||
| Riyadh | 315,589 | 10,483 | 305,106 | 5600 | 399 | 5999 | 4112 | 372 | 4484 | 390 | 33.2 | 17.7 | 1.3 | 19.0 |
| Hail | 47,038 | 106 | 46,932 | 93 | 9 | 102 | 4 | 0 | 4 | 3 | 2.3 | 2.0 | 0.2 | 2.2 |
| Qassim | 96,391 | 350 | 96,041 | 175 | 5 | 180 | 164 | 6 | 170 | 3 | 3.6 | 1.8 | 0.1 | 1.9 |
| Eastern region | 258,137 | 49,850 | 208,287 | 32,017 | 2604 | 34,621 | 15,094 | 135 | 15,229 | 5175 | 193.1 | 124.0 | 10.1 | 134.1 |
| Baha | 43,208 | 1968 | 41,240 | 1547 | 10 | 1557 | 385 | 26 | 411 | 76 | 45.5 | 35.8 | 0.2 | 36.0 |
| Madinah | 111,521 | 2691 | 108,830 | 2144 | 135 | 2279 | 375 | 37 | 412 | 97 | 24.1 | 19.2 | 1.2 | 20.4 |
| Makkah | 326,128 | 13,961 | 312,167 | 9634 | 248 | 9882 | 4050 | 29 | 4079 | 1055 | 42.8 | 29.5 | 0.8 | 30.3 |
| Northern borders | 21,802 | 285 | 21,517 | 70 | 5 | 75 | 171 | 39 | 210 | 4 | 13.1 | 3.2 | 0.2 | 3.4 |
| Tabouk | 48,897 | 1407 | 47,490 | 1114 | 139 | 1253 | 149 | 5 | 154 | 35 | 28.8 | 22.8 | 2.8 | 25.6 |
| Jouf | 35,066 | 151 | 34,915 | 95 | 7 | 102 | 48 | 1 | 49 | 1 | 4.3 | 2.7 | 0.2 | 2.9 |
| Aseer | 164,706 | 5335 | 159,371 | 4858 | 168 | 5026 | 303 | 6 | 309 | 388 | 32.4 | 29.5 | 1.0 | 30.5 |
| Jazzan | 74,793 | 12,956 | 61,837 | 8894 | 577 | 9471 | 3370 | 115 | 3485 | 1682 | 173.2 | 118.9 | 7.7 | 126.6 |
| Najran | 28,864 | 425 | 28,439 | 408 | 7 | 415 | 10 | 0 | 10 | 16 | 14.7 | 14.1 | 0.2 | 14.4 |
| Total | 15,72,140 | 99,968 | 14,72,172 | 66,649 | 4313 | 70,962 | 28,235 | 771 | 29,006 | 8925 | 63.6 P < 0.001 |
42.4 P < 0.001 |
2.7 P < 0.001 |
45.1 P < 0.001 |
| Geographic regions: | ||||||||||||||
| Central | 459,018 | 10,939 | 448,079 | 5868 | 413 | 6281 | 4280 | 378 | 4658 | 396 | 23.8 | 12.8 | 0.9 | 13.7 |
| Eastern | 258,137 | 49,850 | 208,287 | 32,017 | 2604 | 34,621 | 15,094 | 135 | 15,229 | 5175 | 193.1 | 124.0 | 10.1 | 134.1 |
| Western | 480,857 | 18,620 | 462,237 | 13,325 | 393 | 13,718 | 4810 | 92 | 4902 | 1228 | 38.7 | 27.7 | 0.8 | 28.5 |
| Northern | 105,765 | 1843 | 103,922 | 1279 | 151 | 1430 | 368 | 45 | 413 | 40 | 17.4 | 12.1 | 1.4 | 13.5 |
| Southern | 268,363 | 18,716 | 249,647 | 14,160 | 752 | 14,912 | 3683 | 121 | 3804 | 2086 | 69.7 | 52.8 | 2.8 | 55.6 |
| Total | 15,72,140 | 99,968 | 14,72,172 | 66,649 | 4313 | 70,962 | 28,235 | 771 | 29,006 | 8925 | 63.6 P < 0.001 |
42.4 P < 0.001 |
2.7 P < 0.001 |
45.1 P < 0.001 |
PMS&GC, premarital screening and genetic counseling.
Number of examined persons in the PMS&GCa program between 2004 and 2009 and their genetic testing results by administrative and geographic regions of Saudi Arabia.
Out of 15,72,140 men and women examined, 29,006 (1.8%) tested positive (28,535 carriers and 771 cases) for β-thalassemia gene (Table 1). The prevalence of β-thalassemia was 18.5 (18.0 for carriers and 0.5 for cases) per 1000 examined persons. The prevalence was highest in the Eastern region (59.0), moderate in the Southern, Western and Central regions (14.2, 10.2, and 10.1, respectively), and lowest in the Northern region (3.9), (Fig. 1). Similar to sickle cell disease, Eastern region and Jazzan were the two administrative regions with the highest prevalence of β-thalassemia (59.0 and 46.6, respectively) (Fig. 2B). Four administrative regions (Riyadh, Makkah, Northern borders, and Albaha) had moderate β-thalassemia prevalence (range between 9.5 and 14.2). The remaining administrative regions demonstrated low β-thalassemia prevalence (below 4 per 1000 examined persons). Similar to sickle cell disease, there were considerable variations in the prevalence of β-thalassemia within the same administrative or geographical regions. For example, Qunfudah was significantly higher than other health regions of the Western region while Hafr Albaten, which administratively belongs to the Eastern region, demonstrated zero prevalence of β-thalassemia. The overall carrier–case ratio for β-thalassemia was 36.6 with considerable regional variations being highest in the Eastern region (111.8) and lowest in the Northern region (8.2), (Fig. 3).

Carrier–case ratio of sickle cell disease and β-thalassemia among examined persons in the PMS&GC program between 2004 and 2009 by geographic regions of Saudi Arabia.
3.1. At-risk marriages
In this category, a total of 8925 at-risk marriages were cited because both members of the couple were carriers or cases (or one was a case and the other was a carrier) of sickle cell disease and/or β-thalassemia. The frequency of at-risk marriages was 5.7 per 1000 examined persons and 8.9 per 100 positive results. Similar to the prevalence of sickle cell disease and β-thalassemia, the frequency of at-risk marriages was highest in the Eastern region followed by the Southern and Western regions and lowest in the Northern and Central regions (Fig. 1).
4. Discussion
This report studied regional differences in hemoglobinopathies and at-risk marriages using 6 years of national data from the PMS&GC program. Detecting regional differences in hemoglobinopathies may be critical for policy makers to better allocate resources and sometimes modify services to achieve the highest efficiency of the available screening program. Although this study is not the first to address regional differences in sickle cell disease and β-thalassemia in SA [10,12,13], it better reflects the current situation because the data from the PMS&GC program is unified, standardized and involves the whole country.
When comparing the current overall prevalence of sickle cell disease to previously published studies, the demonstrated rates seems to be much lower than studies done before the PMS&GC program, but are similar to those done after the PMS&GC program. In the largest national study of males and females between the ages of 2 and 60 years old in the 1980s and the early 1990s, El-Hazmi et al. [18] estimated sickle cell disease carriers and cases at 73.6 and 10.6 per 1000, respectively, compared with 42.4 and 2.7, respectively in this study which could be partially explained by the absence of the pediatric population in this study. In a more recent study of patients aged between newborn and 19 years old, Al-Qurashi et al. [13] estimated sickle cell disease cases at 2.4 per 1000, which is close to the estimation of this study. The same findings were reported during the first 2 years of PMS&GC program [12]. The differences in sickle cell disease rates in this study and pre-PMS&GC program studies may be confounded by the differences in the studied population and study methods. Moreover, adult-based rates (as in this study) should be lower than rates calculated from neonates or children as the former rates reflect incidence while the later rates reflect incidence and survival.
Unlike sickle cell disease, regional and overall prevalence of β-thalassemia in the current study was much lower than previously published rates irrespective of the timing of the PMS&GC program, with probably wider difference after the program than before it. For example, between the 1980s and the 1990s, β-thalassemia rates were estimated at 130 and 36 per 1000 examined persons in Eastern and Central regions (compared to 58.5 and 9.3), respectively [10]. β-Thalassemia carriers per 1000 were estimated earlier from the PMS&GC program to be 32 in all regions of SA and 34 in Al-Hassa region (compared with 18 and 26, respectively) [12].
The current regional differences in sickle cell disease and β-thalassemia in SA were generally similar to those reported previously, but the magnitude of such differences was probably lower. Similar to previous studies [10,12,13,18,19], the highest prevalence for both diseases was seen in the Eastern region while the lowest prevalence was seen in the Northern region (β-thalassemia) or both the Northern and Central regions (sickle cell disease). For sickle cell disease, geographic regional differences were 10-fold in the current study compared with about 25-fold in previous studies [10,13]. For β-thalassemia, the Eastern-Riyadh difference was 6.7-fold in the current study compared with about 9.0-fold in previous studies [12]. In both sickle cell disease and β-thalassemia prevalence, Jazzan was comparable with the Eastern region, but higher than the rest of the Southern and Western administrative regions (such difference was higher with β-thalassemia than with sickle cell disease). This created a Central belt of low prevalence of sickle cell disease sandwiched between high Eastern and South-Western regions. Such distinction was not seen with β-thalassemia (Fig. 2A and B).
It is difficult to explain regional differences in sickle cell disease and β-thalassemia in SA. Certain cultural factors in SA may contribute to the high prevalence of both diseases. These include the high frequency of consanguineous marriages (exceeding 55%) and the large family size [20–22]. Regional variations in the consanguinity rates in SA were reported with conflicting results [20,21]. Some published data suggested that the prevalence of first degree consanguinity is highest in the Eastern region (40.9%) and lowest in the Northern region (17.9%) [21]. It was also suggested that malaria hyper-endemic areas provide survival advantage and hence higher prevalence of sickle cell trait [18,19]. According to this hypothesis, areas that used to be endemic with malaria in the past (coastal areas in the Eastern and Southwestern regions) concentrated the sickle cell gene. Areas with higher prevalence of hemoglobinopathies (e.g. the Eastern region) could make it relatively difficult for an at-risk couple member to find an alternative socially suitable safe-match compared with low prevalence areas creating a vicious cycle of sickle cell trait concentration.
It was suggested that the Eastern region has more benign sickle cell disease compared with the South-West [23–25]. This possibly offered better survival chances of cases in the Eastern region. Consequently, the carrier–case ratio of sickle cell disease in this study was lower in the Eastern region (12.3) than the Western (33.9) and Southern (18.8) regions. Unlike the sickle cell disease, the carrier–case ratio of β-thalassemia was highest in the Eastern (111.3) and Western (52.3) regions. Whether this indicates more aggressive β-thalassemia in these regions compared with Central and Northern regions is something to be investigated. Not surprisingly, the Eastern region that had the highest prevalence of both sickle cell disease and β-thalassemia embraced 58% of all detected at-risk marriages during the study. This may necessitate allocation of more resources (clinics, laboratories and counselors) to the Eastern region. In addition, studying regional differences of responsible mutations, cultural factors, and morbidity and mortality behavior of both diseases may help the policy makers to improve the available prevention and management programs.
5. Conclusion
Based on 6 years of national data from the PMS&GC program, this study reports the vast regional differences in hemoglobinopathies among adult Saudi nationals approaching marriage. This may help policy-makers better allocate resources of available preventive and management programs.
Conflict of interest
None declared.
References
Cite this article
TY - JOUR AU - Ziad A. Memish AU - Tariq M. Owaidah AU - Mohamad Y. Saeedi PY - 2011 DA - 2011/07/28 TI - Marked regional variations in the prevalence of sickle cell disease and β-thalassemia in Saudi Arabia: Findings from the premarital screening and genetic counseling program JO - Journal of Epidemiology and Global Health SP - 61 EP - 68 VL - 1 IS - 1 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2011.06.002 DO - 10.1016/j.jegh.2011.06.002 ID - Memish2011 ER -
