Call for Awareness: ST-Segment Elevation Myocardial Infarction Presentation is Delayed more than What We Expect
 , Hala El-Saka2, Bushra E. Al-Hutahly3, Alaa E. Abd Elmoniem3,
, Hala El-Saka2, Bushra E. Al-Hutahly3, Alaa E. Abd Elmoniem3, 
- DOI
- 10.2991/dsahmj.k.201105.001How to use a DOI?
- Keywords
- Acute myocardial infarction; histopathology; thrombectomy
- Abstract
Background: ST-Segment Elevation Myocardial Infarction (STEMI) therapy in Saudi Arabia may have particular limitations because of geographic limitations, human resource distribution, and lack of an effective first response system. The aim of this study is to investigate the effective age of STEMI in Saudi Arabia by focusing on the histopathology of extracted thrombus.
Methods: Details of 25 consecutive cases of STEMI patients who were treated with primary Percutaneous Coronary Intervention (PCI), including using suction thrombectomy, were analyzed using clinical, angiographic, and histopathological data. Based on histopathological findings supported by immunohistochemical study, we further classify the small cohort according to age and compare them with available data in the literature.
Results: Results showed that nine out of 25 patients had non-recent thrombus (36%), which suggests the age of STEMI of more than 24 h. In a literature review of histopathology studies on thrombus in STEMI, the rate of non-recent thrombus in STEMI of 30% is no different to our own finding. We observed a high incidence of no-reflow in this cohort [14/25 (56%) patients had no reflow], which might be histopathologically related to the late presentation.
Conclusion: In this single-center study, one-third of patients with STEMI who were candidates for primary PCI treatment have non-fresh thrombus. This study encourages the adoption of a more effective first response system as part of the Saudi STEMI program including greater efforts to enhance patient and physician education.
- Copyright
- © 2020 Dr. Sulaiman Al Habib Medical Group. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
ST-Segment Elevation Myocardial Infarction (STEMI) management success is markedly affected by time of revascularization (time is myocardium). One of the most important quality assurance measure in STEMI is the time of hospital contact to first device use, which should be ≤90 min [1] or wiring the lesion in ≤120 min [2]. More data support an even more narrow window in patients who present within the first 2 h of onset of symptom to negate the potential benefit of thrombolysis compared to primary Percutaneous Coronary Intervention (PCI). It has been calculated that each 30-min delay in reperfusion may result in an increase of up to 7.5% in 1-year mortality [3,4]. The timing of revascularization is paramount in all STEMI patients; in fact, in one study, a contact (door)-to-balloon (D2B) time from 150 to 180 min resulted in in-hospital mortality as high as 20% [5].
There is marked heterogeneity in the management of STEMI in Saudi Arabia because of geographic limitations, human resource distribution, and lack of an effective first response system. However, there is marked increase of PCI-capable centers in the country over the past decade, from 40 centers to 72 hospitals. In the STARS-1 program (Saudi Acute Myocardial Infarction Registry), 45% had PCI—in which 65% and 42% of men and women, respectively, had D2B time of <90 min. Only 5.2% of all patients with acute coronary syndrome utilized the ambulance service (emergency medical services) to reach the hospital [6]. In addition, we noticed a significant number of patients who underwent a successful primary PCI, in what appeared to be within the time limit of guidelines, but still sustained a permanent damage to the heart function. This might be explained by a late presentation owing to miscalculated onset of symptoms, which is supposed to be within 12 h so patients can be considered eligible for primary PCI. For a more accurate estimation of time of onset of symptoms, we believe histopathology could provide a hint of such time [7]. Therefore, our aim is to study the actual age of STEMI by examining the histopathology of extracted thrombus.
2. MATERIALS AND METHODS
This study focused on 25 consecutive STEMI patients eligible for primary PCI who were admitted to the emergency department of King Fahd Specialist Hospital in Buraidah, Saudi Arabia. Patients were considered eligible for primary PCI if they had symptoms of acute STEMI (the worst pain) within 12 h of presentation accompanied by ST-segment elevation of more than 0.2 mV in two or more contiguous leads. The primary PCI was performed via femoral access in a standard technique. Suction thrombectomy was performed as per operator discretion when there is a visible thrombus angiographically. The only device used was Export 6 Fr suction catheter (Medtronic Vascular Incorporation, Santa Rosa, CA, USA). The standard pharmacological therapy includes pretreatment in the emergency department using 300 mg aspirin, 600 mg clopidogrel, and 5000 units of unfractionated heparin. The use of IIb/IIIa inhibitors and antithrombotic therapy was at the discretion of the operator.
All patients consented to participate in this study. The exclusion criteria were as follows: (1) when no thrombi were retrieved by the thrombectomy device; (2) the patient refused to participate; and (3) when the primary PCI is performed more than 12 h after onset of symptoms. Clinical, angiographic, and histopathological data were collected prospectively from all included cases. The thrombectomy samples were transported immediately to the histopathology laboratory on a special container with formaldehyde solution. If the procedure was performed beyond the working hours of the histopathology laboratory, the samples were kept in the catheterization laboratory (in formaldehyde solution) until the next working day of the histopathology laboratory. The histopathology data were classified according to the estimated age of thrombus: (1) fresh thrombus; (2) lytic thrombus, age 1–5 days; and (3) organized thrombus, age longer than 5 days [7].
3. RESULTS
From March to June 2012, a total of 25 consecutive STEMI patients who were eligible for the study were enrolled and included for prospective data collection. All patients clinically fulfilled the criteria for primary PCI (i.e., onset of symptoms within 12 h and D2B time within 120 min). All patients signed the informed consent form.
The participants consisted of men with an average age of 49.5 ± 11 years, of whom 20% had a history of coronary artery disease. The culprit vessels were right coronary artery, left anterior descending artery, and left circumflex in 48%, 44%, and 8%, respectively. There were two cardiogenic shock patients, and 44% had diabetes mellitus. The average D2B time was 127 ± 52 min. A no-reflow phenomenon was observed in 14 patients (56%). Upon histopathology study, we noticed that a predominant cleft of cholesterol was present, which may denote a high prevalence of dyslipidemia (Figure 1). The histopathology classification of thrombus based on age showed that 17 patients had recent thrombus (Figure 2), four patients had lytic thrombus (Figure 3), three patients had organized thrombus (Figure 4), two patients had no thrombus, and only patient had plaque components (Table 1). The histopathology data showed eight out of 25 patients had non-recent thrombus (32%), which implies the age of STEMI is more than 24 h despite the patients being clinically eligible for primary PCI (i.e., recorded onset of symptoms of <12 h).
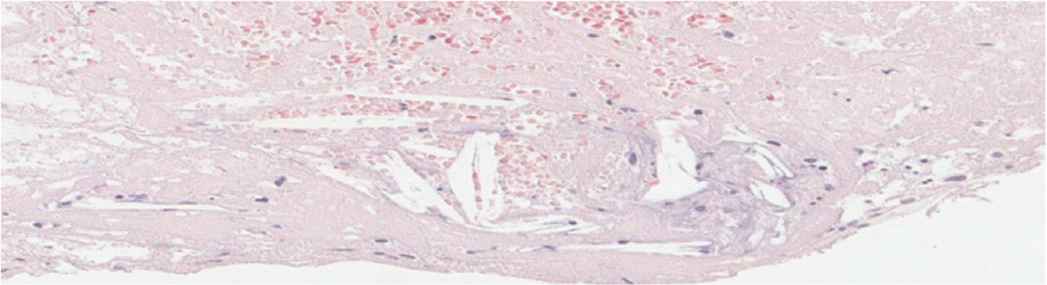
Cholesterol clefts (54.5%). H&E, hematoxylin and eosin.
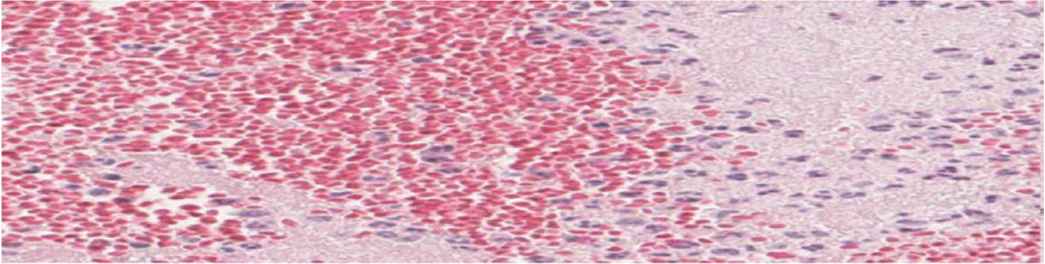
Fresh thrombus (72.72%) showing intact Red Blood Cells (RBCs) and granulocytes amidst fibrin. Hematoxylin and Eosin (H&E), 40×.
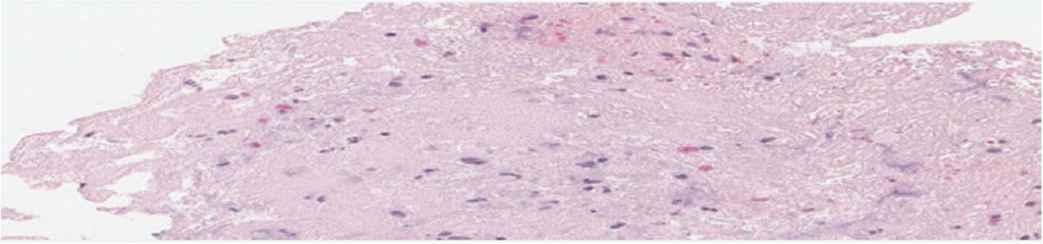
Lytic thrombus (9.09%) showing homogenization of structural elements with nuclear fragmentation. Hematoxylin and Eosin (H&E), 40×.
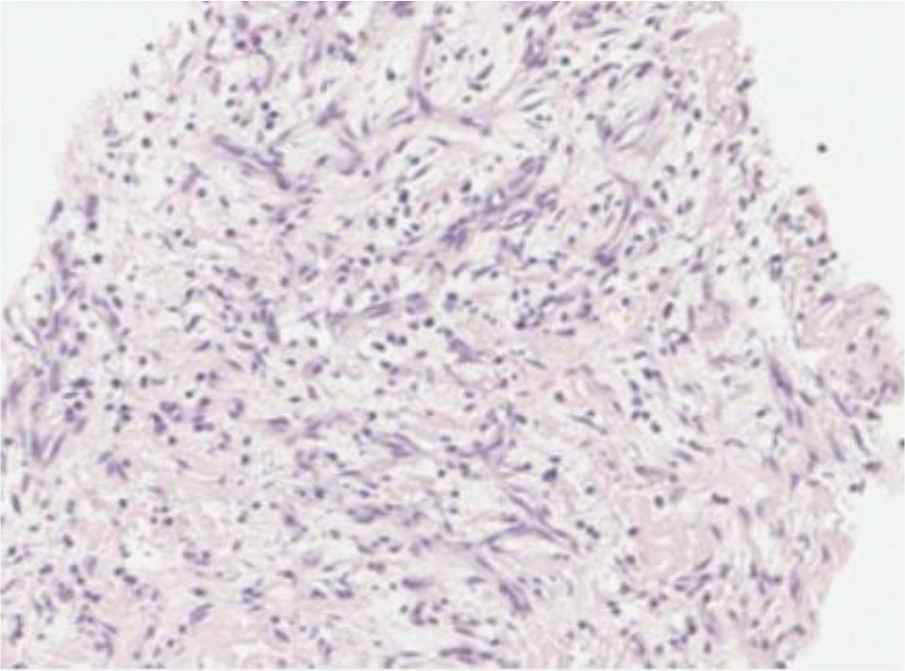
Organized thrombus (18.18%) showing ingrowth of spindle-shaped cells and capillary vessel ingrowth. Hematoxylin and Eosin (H&E), 40×.
| No. | Age of thrombus | Other components |
|---|---|---|
| 1 | Recent thrombus | |
| 2 | Lytic thrombus | |
| 3 | Recent thrombus | |
| 4 | Recent thrombus | |
| 5 | Recent thrombus | Plaque component |
| 6 | Recent thrombus | |
| 7 | Recent thrombus | Plaque component |
| 8 | Lytic thrombus | |
| 9 | Organized thrombus | |
| 10 | Recent thrombus | Plaque component with cholesterol clefts and calcification |
| 11 | Recent thrombus | |
| 12 | Recent thrombus | Plaque component |
| 13 | Recent thrombus and lytic thrombus | |
| 14 | Lytic thrombus | |
| 15 | Recent thrombus and organized thrombus | |
| 16 | Recent thrombus | |
| 17 | Recent thrombus | |
| 18 | Recent thrombus | Plaque component |
| 19 | Recent thrombus | Plaque component and cholesterol clefts |
| 20 | Recent thrombus | Plaque component and cholesterol clefts |
| 21 | Recent thrombus and organized thrombus | |
| 22 | No thrombus | Plaque component |
| 23 | Recent thrombus | Plaque component |
| 24 | No thrombus | Plaque component |
| 25 | Recent thrombus |
Histopathology data
The average time of symptom-to-balloon time is 5 h and 30 min with a standard deviation of 193 min. Table 2 demonstrates the detailed timing of symptoms and balloon together with the result of histopathology analysis to each corresponding patient.
| Symptom time (hh:mm) | Balloon time (hh:mm) | Symptom-to-balloon time (hh:mm) | Histopathology result |
|---|---|---|---|
| 4:00 | 10:31 | 6:31 | Recent |
| 20:00 | 23:40 | 3:40 | Lytic |
| 11:30 | 14:27 | 2:57 | Recent |
| 11:30 | 15:30 | 4:00 | Recent |
| 17:00 | 22:35 | 5:35 | Recent + plaque materials |
| 5:00 | 13:15 | 8:15 | Recent |
| NA | 9:45 | Recent + plaque materials | |
| 11:40 | 13:22 | 1:42 | Lytic |
| 1:00 | 3:10 | 2:10 | Organized |
| 3:00 | 14:39 | 11:39 | Recent + plaque materials |
| 17:00 | 20:04 | 3:04 | Recent |
| 12:00 | 18:36 | 6:36 | Recent + plaque materials |
| 3:00 | 12:40 | 9:40 | Lytic |
| NA | 11:45 | Lytic | |
| NA | 9:25 | Organized | |
| 18:00 | 2:07 | 8:02 | Recent |
| 6:00 | 19:44 | 13:44 | Recent |
| 8:30 | 12:45 | 4:15 | Recent + plaque materials |
| 8:00 | 12:58 | 4:58 | Recent + plaque materials |
| NA | 6:17 | Recent + plaque materials | |
| 16:00 | 19:58 | 3:58 | Organized |
| 10:00 | 14:53 | 4:53 | Plaque materials |
| 17:00 | 21:09 | 4:09 | Recent + plaque materials |
| 19:20:00 | 20:50 | 1:30 | Recent + plaque materials |
| 0:00 | 4:12 | 4:12 | Recent |
Average symptom-to-balloon time is 5 h and 30 min (standard deviation, 193 min)
The incidence of no reflow in this small cohort study is very high (54%). A comparison between recent and old thrombus showed that there is no clear relationship with development of no reflow (Figure 5). There is no difference between “no reflow” and normal flow groups among recent thrombus patients (11 vs. 8, respectively; p = 0.73). In addition, there is no correlation between color of thrombus and development of no reflow, although the gross color of thrombus among patients with “no reflow” tend to be darker in color (12 vs. 9 in “no reflow” and normal flow, respectively; p = 0.39).
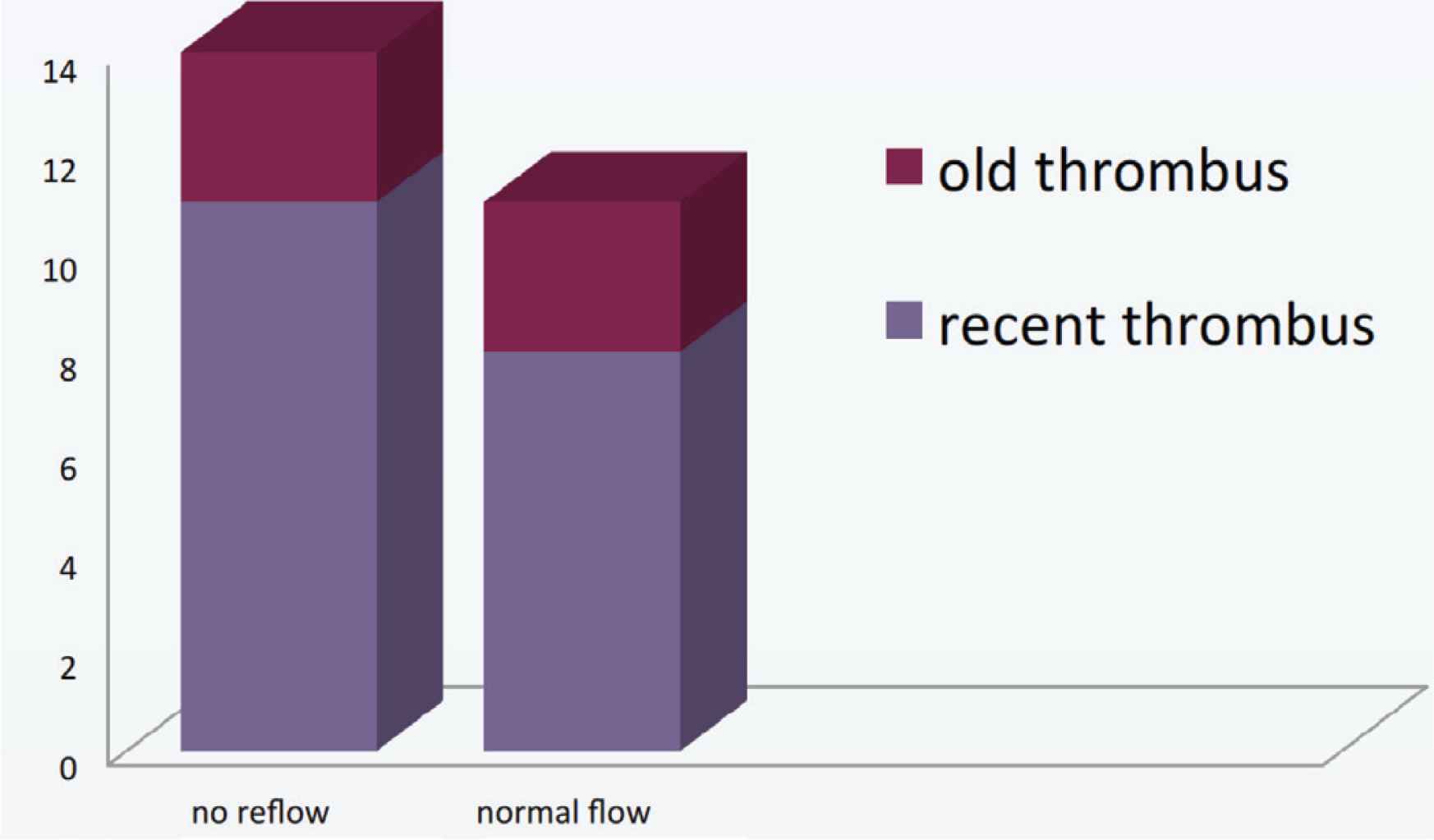
Comparison of no-reflow versus normal flow in terms of old and recent thrombi.
4. DISCUSSION
Our study showed that about a third of STEMI patients eligible for primary PCI and thought to have recent events are already late. This indicates that use of the D2B time value as a surrogate marker for clinical improvement is not an accurate tool to predict the clinical outcomes of patients after primary PCI. This is a call for public awareness to optimize the clinical benefit of STEMI management via early recognition of symptoms to encourage patients to seek early medical advice.
The D2B time exceeded the benchmark in more than half of the patients, in which the average value was 127 min. This can be explained by using actual balloon time back in 2011 while the majority of the cohort had export atherectomy prior to balloon time. Nowadays, we use first device use or angio time showing TIMI three flow, whichever earlier time would be recorded. Nevertheless, this observation provides a deeper insight indicating room for improvement in both emergency departments and cardiology departments. However, this does not explain why thrombus age exceeded 1 day in one-third of patients and, in some cases it was more than 5 days.
Symptom-to-balloon time may demonstrate a better age of STEMI compared with door time. As per the contemporary guidelines, the 12-h window remains for primary PCI, and our average symptom-to-balloon time is 5 h and 30 min (standard deviation, 193 min). This wide standard deviation is explained by the small sample size of this study. It should be noted that in four patients the symptom onset time was missing; however, as their histopathology data are recent (one organized and one lytic thrombus), this does not affect our general finding.
This disparity between the symptom onset time of STEMI and thrombus histopathology age might be attributed to the fact that plaque instability frequently occurs days or weeks prior to occlusive coronary thrombosis. The layered composition of thrombus suggests episodic growth of thrombus prior to the onset of occlusive thrombosis and the onset of symptoms. Therefore, the superficial layers of thrombus might be dislodged owing to the shear stress, leaving the older layer of thrombus behind to be extracted by the thrombectomy device.
In a literature review, we found similar findings to our study by Carol et al. [7], who showed that lytic or organized thrombi were aspirated in one-third of cases that presented within 12 after onset of symptoms. In this study, the material retrieved was sufficient for pathological analysis in 81 out of 118 consecutive STEMI patients who underwent thrombectomy. From that cohort, 83% presented within 12 h of symptoms.
It is well known that the no-reflow phenomenon correlates with longer ischemic time [8], although our observation of no correlation between recent and non-recent thrombus by histopathology in regard to the development of no-reflow phenomenon can be explained by the presence of collateral flow physiology that would limit the time of ischemia. In addition, owing to the small number of participants, we cannot generate a conclusion outside the aim of this study.
5. LIMITATIONS AND CONCLUSION
In a single-center study in Saudi Arabia (Prince Sultan Cardiac Center in Qassim), one-third of patients with STEMI who were eligible for PCI had thrombus that was more than 1 day old. This might partly explain the high prevalence of no reflow phenomenon (54%) in this cohort of 25 consecutive STEMI patients. This study encourages the adoption of a more effective strategy as part of the Saudi STEMI program, and greater efforts to enhance patient and physician education regarding this disease.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
OAS and AEAE study the conceptualization and writing (review and editing) the manuscript. HE-S carried out the histopathology readings as well as writing the legends. BEA-H and OAS collected the data and analysed them in the original draft.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Owayed Al Shammeri AU - Hala El-Saka AU - Bushra E. Al-Hutahly AU - Alaa E. Abd Elmoniem PY - 2020 DA - 2020/11/18 TI - Call for Awareness: ST-Segment Elevation Myocardial Infarction Presentation is Delayed more than What We Expect JO - Dr. Sulaiman Al Habib Medical Journal SP - 36 EP - 39 VL - 3 IS - 1 SN - 2590-3349 UR - https://doi.org/10.2991/dsahmj.k.201105.001 DO - 10.2991/dsahmj.k.201105.001 ID - AlShammeri2020 ER -
