Unusual Presentations of Intestinal Schistosomiasis
- DOI
- 10.2991/dsahmj.k.200514.001How to use a DOI?
- Keywords
- Bilharzia; colonic; intestinal; polyp; presentation; Saudi; schistosomiasis
- Abstract
Schistosomiasis is a common parasitic infestation that affects 200 million people worldwide. There are more than 76 endemic countries that suffer from this infestation, leading to 200,000 deaths annually. Intestinal schistosomiasis is known to cause a variety of serious gastrointestinal complications. Thus, it is important to diagnose it early to prevent such complications and relieve symptoms early. A typical infection with intestinal schistosomiasis tends to present with chronic diarrhea, abdominal pain, dysentery, and in severe cases portal hypertension and hepatosplenomegaly. However, in this study the authors report two cases that came with unusual presentations of intestinal schistosomiasis during their outpatient clinic evaluation.
Case Presentation: The first patient is a 33-year-old male Yemeni national who was referred for investigation of a pedunculated rectal polyp. The patient was otherwise asymptomatic with no significant medical history. The second patient is a 39-year-old male Saudi national who presented with constipation, abdominal pain, and bloating. The patient was initially diagnosed as a case of irritable bowel syndrome and was managed conservatively for 2 years with no improvement.
Conclusion: Histopathological evidence via biopsies revealed intestinal schistosomiasis in both patients. Therefore, in endemic areas it remains important to keep intestinal schistosomiasis in the differentials when dealing with vague intestinal signs and symptoms. It is also important to not rule out schistosomiasis from a negative stool egg screening alone as this tool tends to yield false negative results during acute infections and low-intensity chronic infections.
- Copyright
- © 2020 Dr. Sulaiman Al Habib Medical Group. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Schistosoma (Bilharzia) is the third most catastrophic and neglected tropical disease with a high morbidity and mortality rate, affecting 12.7 million individuals in the Middle East and the North African region; worldwide, it is believed that 200 million people are infected [1–3]. In Saudi Arabia alone, 0.025% of the population (in the year 2010) suffers from this devastating parasitic infection [4]. This infection is caused by flukes (trematodes) [1]. The Schistosoma species that infect human hosts are divided into five groups: Schistosoma japonicum, Schistosoma mansoni, Schistosoma haematobium, Schistosoma mekongi, and Schistosoma intercalatum. The S. japonicum group is found in southeastern and eastern Asia including China [5]. The S. mansoni group is mainly found in the sub-Saharan African region and North America [5]. Meanwhile, the S. haematobium group is seen in Africa, Indian Ocean Islands, Arabian Peninsula (including Saudi Arabia), and Mediterranean regions [5]. The last two groups are minor species; Schistosoma mekongi is seen in Laos and Cambodia, and Schistosoma intercalatum is seen in West and Eastern Africa [6].
Although the prevalence of this parasite is high, only 60% of patients are symptomatic and 10% require urgent medical attention [7]. Clinical symptoms are divided into acute and chronic stages. The acute stage is often mild and vague; hence, the diagnosis of schistosomiasis is not usual during this stage. Acute-stage symptoms include swimmer’s itch, cercarial dermatitis, bronchopneumonia, and Katayama syndrome [8]. In regards to the chronic stage, it can occur months to years after initial exposure. Intestinal schistosomiasis involves the deposition of eggs within the liver and intestinal wall, causing multiple granuloma formation [9]. Symptoms include abdominal pain, chronic diarrhea, fatigue, dysentery, per rectal bleeding, and in severe cases can lead to portal hypertension, ascites, and hepatosplenomegaly [7,9]. Other symptoms of schistosoma may arise depending on the location of egg deposit and granuloma formation, for example, cardiopulmonary schistosomiasis, Central Nervous System (CNS) schistosomiasis, and female/male genitourinary schistosomiasis [1]. In this study, we discuss two cases that presented with uncommon clinical findings of intestinal schistosomiasis. The two patients signed a consent form to participate in our study. The Department of Internal Medicine and Infectious Diseases at Dr. Sulaiman AlHabib Arryan Hospital approved our study.
2. CASE REPORTS
2.1. Case 1
A 33-year-old male Yemeni national who resides in Riyadh, Saudi Arabia (and often visits Yemen) was referred to the gastroenterology department by a surgical team with a rectal pedunculated polyp and a history of polyp prolapse via the anus during defecation. The polyp was associated with constipation and rectal bleeding. However, the patient did not complain of any upper gastrointestinal symptoms, abdominal pain, weight loss, fever, or symptoms of anemia. A Complete Blood Count (CBC) as well as prothrombin time and international normalized ratio were done. Then the patient refused to have additional laboratory tests. His CBC showed a low neutrophil and absolute neutrophil count (1.87 × 109/L; normal range, 2.0–6.9 × 109/L), and a high monocyte (0.68 × 109/L; normal range, 0.2–0.7 × 109/L) and eosinophil percentage (7.7%; normal range, 1–6%). The rest of his laboratory results were normal. A colonoscopy was performed, and it showed a large (2 × 2.5 cm2) mobile polyp with a large stalk in the rectum (Figures 1 and 2). It was about 8 cm from the anal verge. An endoloop snare polypectomy and a biopsy were performed, resulting in the unusual findings of several schistosome eggs along with inflammatory reaction, which prompted us to give the diagnosis of retention polyp with extensive colonic schistosomiasis (Figure 3).
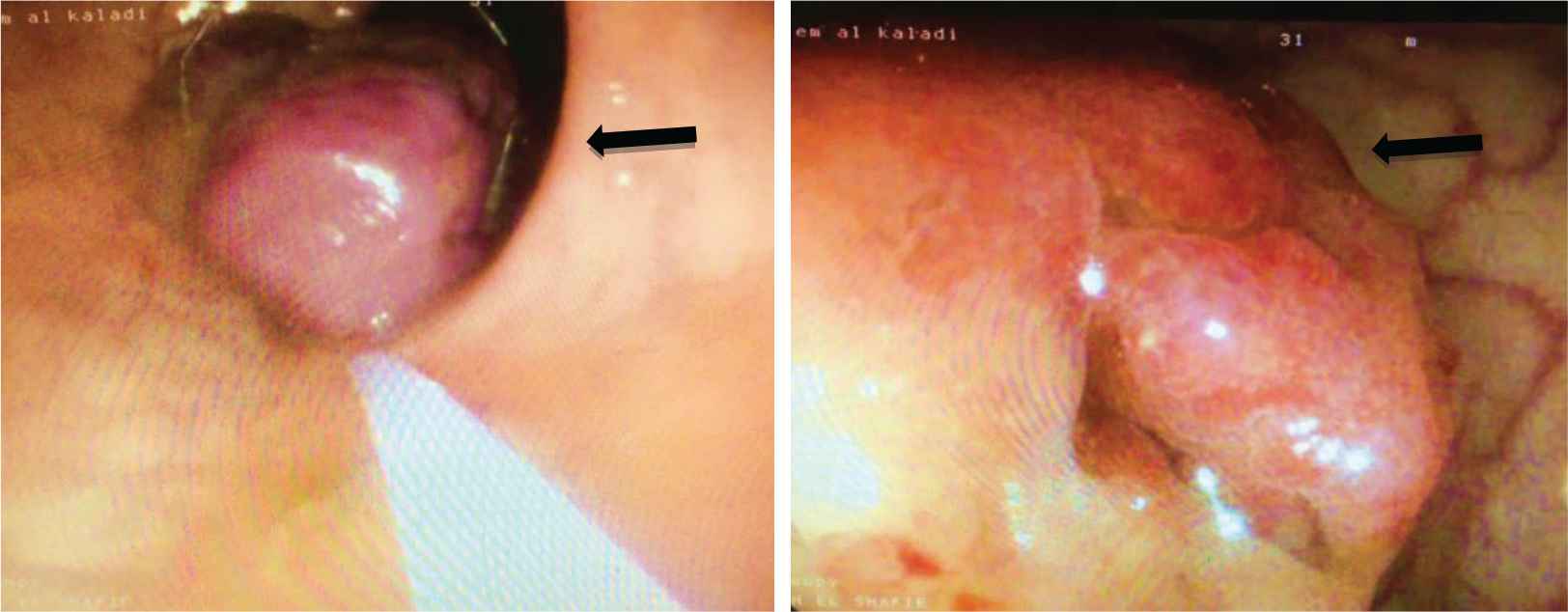
Pedunculated polyp measuring 2 × 2.5 cm2 found within the rectum
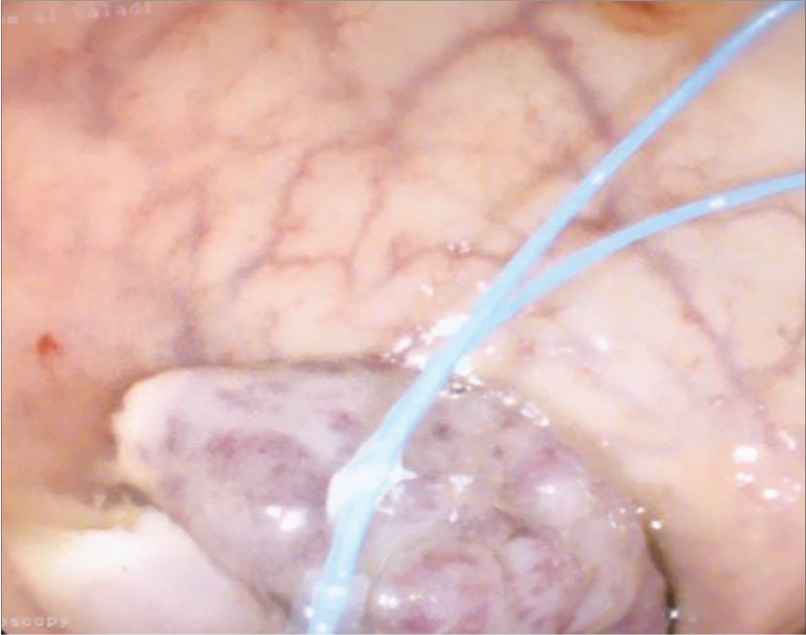
Endoloop snare polypectomy performed on the pedunculated polyp
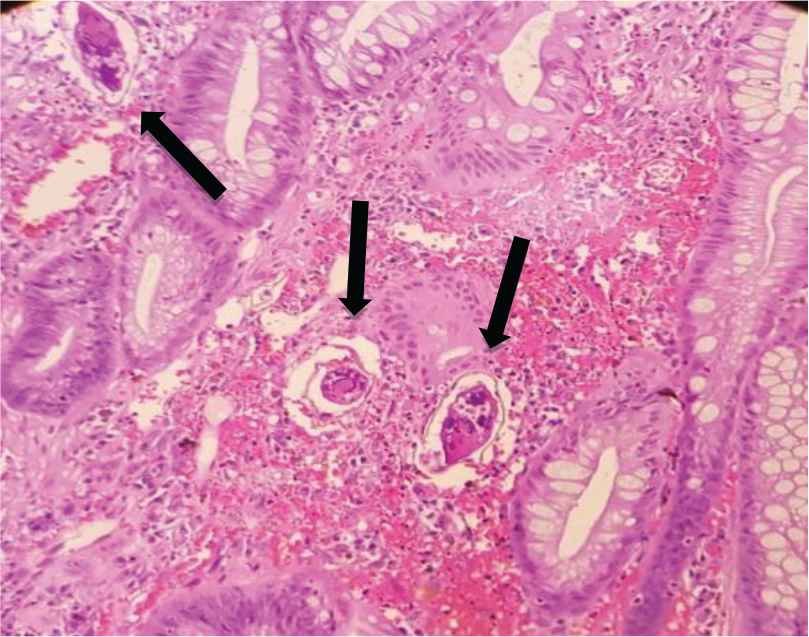
Calcified Schistosoma eggs surrounded by inflammatory cells
2.2. Case 2
The second patient was a 39-year-old Saudi male who presented with altered bowl habits for 2 years. Even though the patient resides in Riyadh, he revealed that he has frequent work-related trips to the southern region of Saudi Arabia near the country’s boarder with Yemen. The patient complained of constipation, intermittent abdominal pain that is more focused on the right and left lower abdomen, bloating, gasses, and fatigue. But he denied having any blood in the stool, fever, weight loss, or straining during defecation. He was not on any specific diet, but his regular meals were composed of traditional Saudi food that consisted of rice, meat, and broth with minimal water intake.
He is known to have type 2 diabetes (and was on glyburide), hypertension (not on any regular medications), and Helicobacter pylori-related gastritis, which was eradicated 2 years ago. He is also a smoker with a 2.5 pack-year history. At presentation, the patient had a blood pressure of 144/88; the rest of his vital signs and physical examination were otherwise unremarkable. He was initially diagnosed in another dispensary as a case of irritable bowel syndrome and was managed conservatively with dietary modification for 2 years with no improvement in his symptoms. Laboratory investigations revealed positive fecal occult blood test, but normal thyroid-stimulating hormone level, lipid profile, erythrocyte sedimentation rate, and liver and renal profile. Abdominal ultrasound showed mild fatty liver, and stool analysis showed no ova or parasites.
Because of the positive fecal occult blood test, a colonoscopy was carried out and revealed nonspecific erythema at the sigmoid colon (Figure 4). Biopsies were taken from the erythematous area and showed schistosoma ova surrounded by inflammatory reactions and embedded within the submucosa of the sigmoid colon (Figure 5).
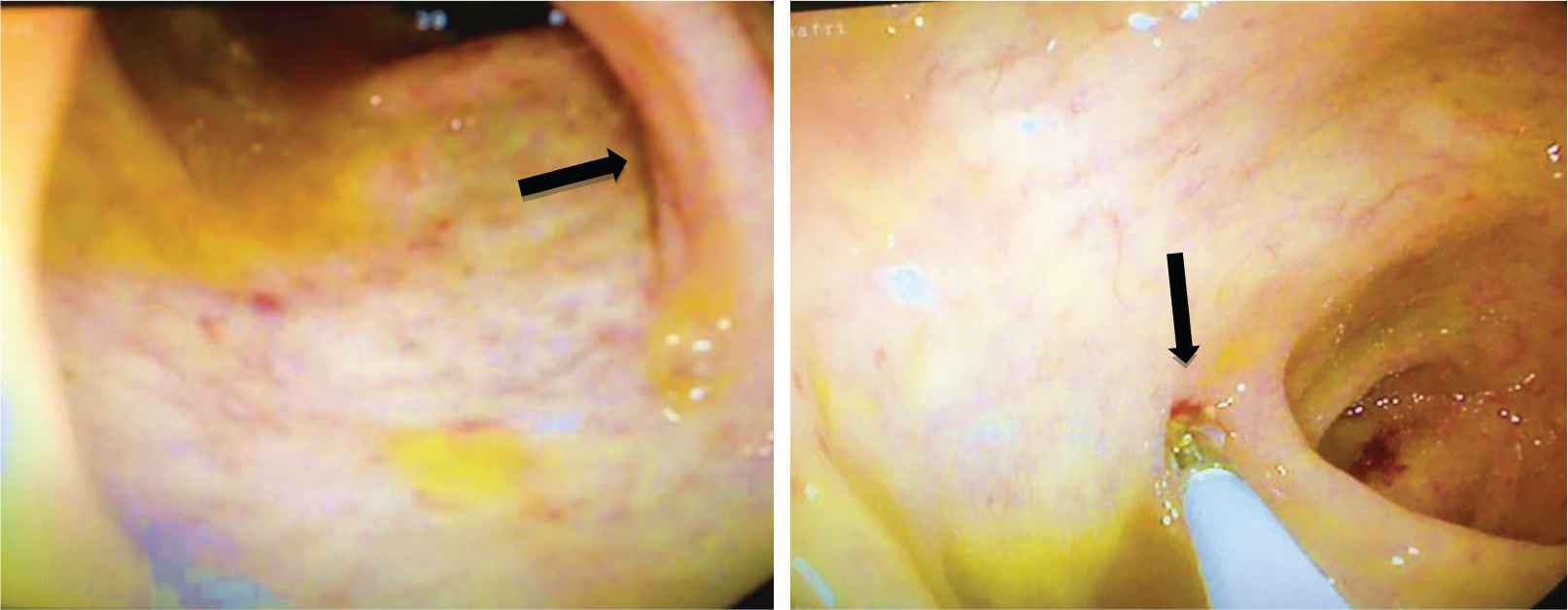
Nonspecific mild erythema found at the sigmoid colon
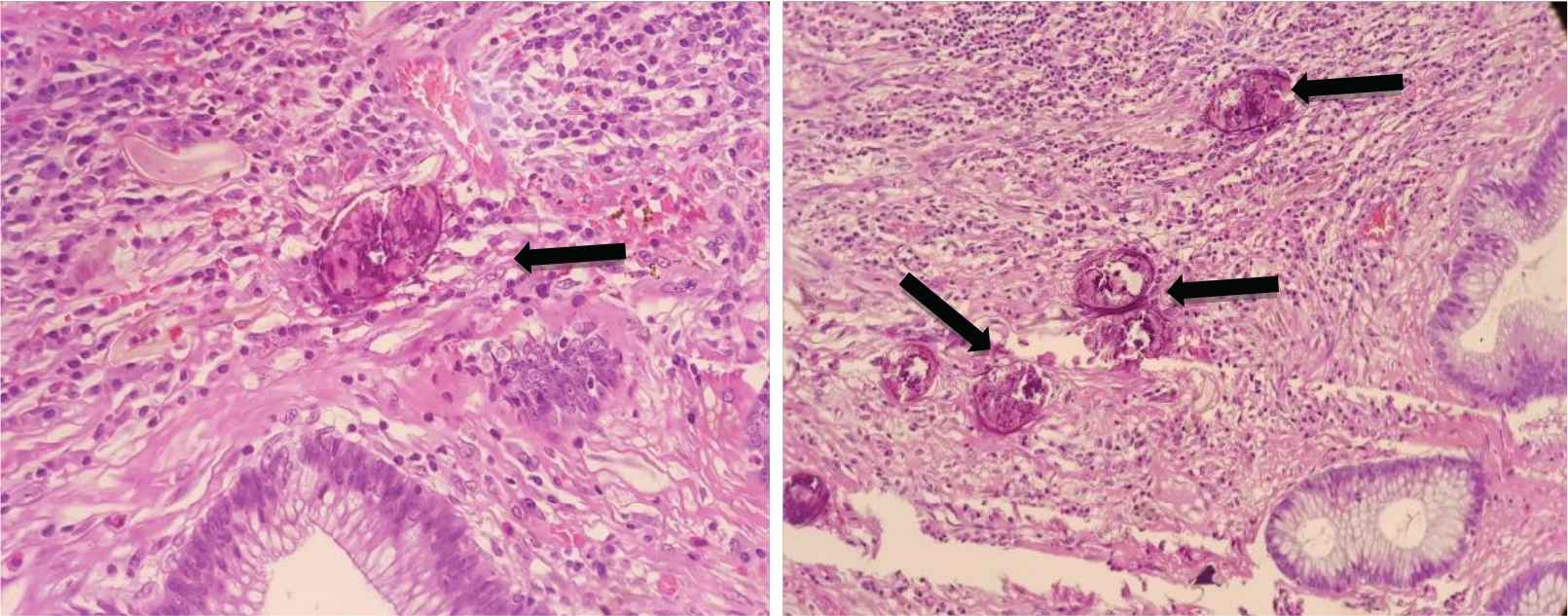
Embedded Schistosoma eggs surrounded by inflammatory cells
Both patients denied any relevant history or a positive family history of bilharziasis. They also denied exposure to water resources that may increase the risk of infection. The patients were referred to the infectious disease team, and received medical treatment with praziquantel at a dose of 40 mg/kg body weight in two divided doses. The therapy course was uneventful, and symptoms completely resolved after treatment with no apparent complications. Regarding the follow-up for both patients, the first patient attended four follow-up visits with the gastroenterology and infectious disease teams after treatment (each visit was 3 weeks apart). Afterward, he was lost to follow-up (he returned to Yemen). Meanwhile, the second patient completed 12 months of follow-up and continues to follow up with the outpatient facility to this day. No repeated colonoscopy has been performed. The patient remained asymptomatic throughout the course of his follow-up.
3. DISCUSSION
In this article we have described atypical presentations of intestinal schistosomiasis. The first patient presented with a rectal polyp but was otherwise asymptomatic. In the second patient, there were altered bowel habits and a picture that resembled irritable bowel syndrome. We performed an extensive Online Literature search involving four databases: Medline Complete, PubMed, Global Health Library, and Annals of Saudi Medicine. They were examined for the presence of any published article that portrays patients with schistosomiasis who presented with colonic polyps in Saudi Arabia. The search yielded 23 case reports in total. The same search yielded 535 reported cases worldwide. The word filters used in this search included: Schistosomiasis, Bilharzia, Polyp, colonic, intestinal, and Saudi.
Both patients appeared to have either resided in Yemen or in the southern region of Saudi Arabia (near its border with Yemen) at one point in their lives. The southern region of Saudi Arabia (especially Jizan) and Yemen are known to be major endemic areas for both urinary and intestinal schistosomiasis. This has sparked the launching of many control programs. However, despite the extensive efforts to reduce the prevalence of the disease, about 3 million people are still known to be infected with schistosomiasis according to the World Health Organization [10]. As for the second patient, owing to the nonspecific nature of the presentation and the lack of ova or parasite in the stool analysis, he was initially diagnosed with irritable bowel syndrome in another dispensary and was managed with conservative therapy for 2 years. It is known that the most specific method for diagnosing a Schistosoma infection is through detection of eggs within the urine, feces, or tissue biopsy [11]. Even though schistosoma eggs can be passed in stool for some time after the infection, a negative egg screening in the stool analysis does not rule out an active infection. This parasitological test may yield negative results during acute infections and low-intensity chronic infections [12]. Thus, it is important to not rule out schistosomiasis by means of stool egg screening alone. Serological tests for anti-schistosoma antibodies can also be done to help with diagnosis. This test is both sensitive and specific; however, it cannot differentiate between a past infection and a currently active infection. In addition, 3 months is needed for the serological screening to become positive. Therefore, those with acute Schistosoma infection may yield negative serological results [13]. There are other recently developed tests that are designed to detect schistosomal DNA or RNA with reportedly high accuracy rates. However, the accessibility of these tests remains an issue as they are not commonly available in all healthcare facilities [9].
Despite the low yield of reported cases, it remains important to keep schistosomiasis as a differential diagnosis when dealing with vague or unclear intestinal signs and symptoms. Untreated intestinal schistosomiasis can lead to many complications such as bowel obstruction, portal hypertension, esophageal varices, anemia, recurrent salmonella bacteremia, and malnutrition and growth retardation in children [14–17]. There is also weak evidence that supports an association between intestinal schistosomiasis (especially S. japonicum) and the development of colorectal cancer [18–20]. Therefore, one must be cautious prior to ruling out Schistosoma infection in a patient with probable suggestive history.
4. CONCLUSION
It is important to recognize Schistosoma infestation as early as possible to prevent the development of future devastating complications as well as alleviate the patient’s symptoms. We have described two patients: one who presented with a rectal polyp and the other with altered bowel habits. In endemic areas, it remains important to keep intestinal schistosomiasis in the differentials when dealing with vague intestinal signs and symptoms such as those mentioned in this article. In addition, it is important not to rule out schistosomiasis from a negative stool egg screening alone as this tool tends to yield false negative results during acute infections and low-intensity chronic infections.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
FB study design, manuscript writing, literature search, and data analysis. AE manuscript writing, literature search, and data analysis. SA study design, manuscript writing, and supervisor. OEY and MA study design. MT histopathological analysis of biopsy slides and data interpretation.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The two patients signed a consent form to participate in our study.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Salah Ahmed AU - Fatima Babiker AU - Areej Elshafie AU - Mogbil Alhedaithy AU - Omer Elfarouq Yousif AU - Maher Toulaymat PY - 2020 DA - 2020/05/20 TI - Unusual Presentations of Intestinal Schistosomiasis JO - Dr. Sulaiman Al Habib Medical Journal SP - 33 EP - 37 VL - 2 IS - 2 SN - 2590-3349 UR - https://doi.org/10.2991/dsahmj.k.200514.001 DO - 10.2991/dsahmj.k.200514.001 ID - Ahmed2020 ER -
