Modification of the Superomedial Pedicle in Wise-pattern Breast Reduction: New Sling Suspension Technique to Prevent (Pseudo)ptosis
- DOI
- 10.2991/dsahmj.k.190916.001How to use a DOI?
- Keywords
- Breast reduction; reduction mammaplasty; pedicle
- Abstract
The combination of the superomedial pedicle with the traditional Wise-pattern skin resection has gained increasing popularity for its versatility and ability to achieve significant reduction of breast parenchyma and skin envelope. In this report, a reproducible new dermal suspension technique is described for cranial stabilization and fixation of the superomedial pedicle in Wise inverted T breast reductions to prevent pseudoptosis.
- Copyright
- © 2019 Dr. Sulaiman Al Habib Medical Group. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
The combination of the superomedial pedicle with the traditional Wise-pattern skin resection has gained increasing popularity for its versatility and ability to achieve significant reduction of breast parenchyma and skin envelope with improved contour and lasting results. The superomedial pedicle brings improved upper pole fullness and breast shape, whereas the Wise-pattern skin resection allows for its reproducible, standardized markings and elimination of excess skin in both vertical and horizontal dimensions [1]. Pseudoptotis has been reported in inverted T-skin excisions especially when the inferior pedicle technique is used [2]. The superomedial pedicle may reduce the risk of (pseudo)ptosis; nevertheless, the weight of the pedicle is only supported by the superior skin flaps and breast parenchyma in case no additional suspension techniques are used. Recurrent breast ptosis may occur especially in patients with poor skin quality. This report describes a new dermal suspension technique for cranial stabilization and fixation of the superomedial pedicle in Wise-pattern inverted T breast reductions.
2. MATERIALS AND METHODS
2.1. Surgical Technique (Author Preference)
2.1.1. Preoperative markings
The preoperative markings were as follows (Figure 1a and b).
- 1.
Inframammary fold (IMF) marking
The final medial and lateral IMF incision is approximately 2 cm shorter than the total IMF length.
- 2.
Breast meridian marking
- 3.
New nipple position
The new nipple position is at the most projecting part of the breast, most likely at the IMF. The nipple position should not be higher than the IMF in case of a concave upper pole of the breast. The average suprasternal notch–nipple distance is more caudal in the ptotic breast with reduced upper pole volume. This prevents excessive resection of breast parenchyma with difficulties in natural shaping of the breast. In addition, this prevents the nipples from being placed too high (too cranial).
- 4.
Areola opening
The final position of the nipple–areola position is made intraoperatively with the patient in a sitting position. This prevents the nipple–areola complex from being placed too high (too cranial) compared with a preoperative planned nipple position.
- 5.
Skin resection pattern
A 7-cm point from the new nipple position in the direction of the IMF is marked. A point is marked 5.5 cm medial and lateral from this point. The medial and lateral vertical limb is drawn connecting these dots. The final vertical limbs are approximately 8.5 cm (planned IMF–nipple distance) in length with a base of 11 cm. The caudal ends of the limbs are approximated with the surgeon’s hands to simulate the reduction. The nipple position and base width can be adjusted based on this maneuver. The final inframammary incisions are planned a few centimeters shorter than the pre-existing IMF length, as long as care is taken to resect the breast tissue that would otherwise remain in that area. The suture for the inverted T marking is placed cranially on a “hilltop” position to prevent extensive traction on the inverted T suture. The medial and lateral incisions are curved to extend the length of the medial and lateral incisions, which provide additional tension reduction on the inverted T suture (Figure 1b).
- 6.
Liposuction marking
Additional liposuction of the lateral breast and axilla area is performed in case of lipoaccumulation in these anatomical areas. The liposuction procedure reduces the length of the lateral IMF incision. The lateral marking of the IMF is 2 cm shorter than the actual IMF as described above.
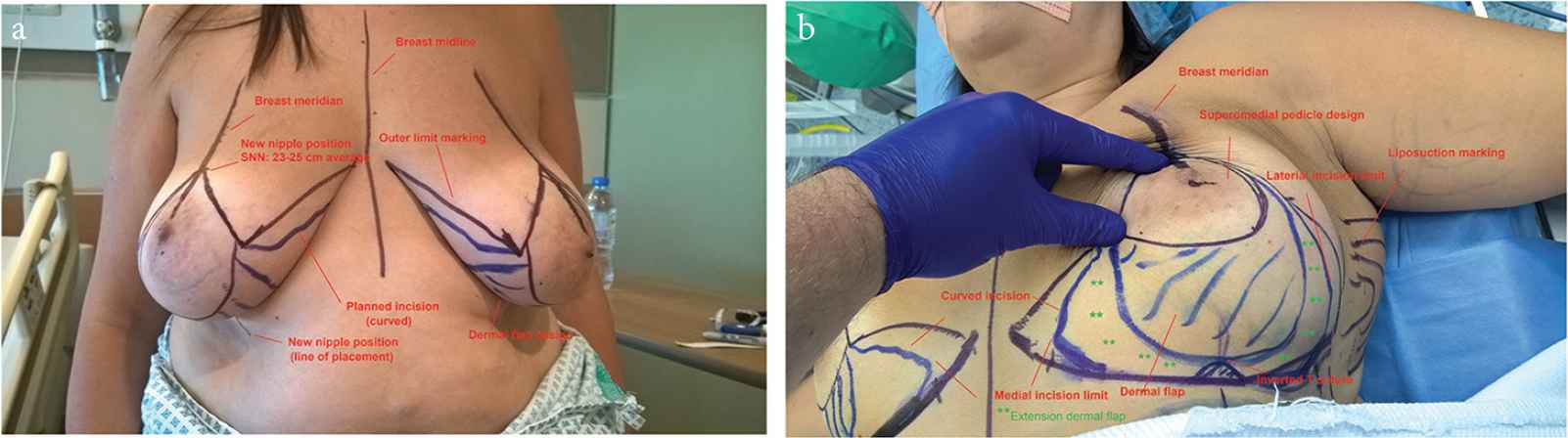
(a and b) Preoperative markings. Note that the dermal flap design can be extended medially and laterally.
2.2. Operative Technique
The patient is placed in supine position.
Subcutaneous infiltration with a solution of 500 ml NaCl 0.9%/25 ml lidocaine 1%/6 ml 8.4% sodium bicarbonate (1 mEq/ml) with 0.5 ml 1:1000 adrenaline at the skin resection patterns and the liposuction areas but not in the pedicle area (author preference). Nipple–areola complex marking has a diameter of 4.5 cm. De-epithelialization of the superomedial pedicle with preservation of the nipple–areola complex. Incision of the skin resection lines. Prepectoral fascia dissection in a Lotus flap pattern without dissection at the medial side of the pedicle.
Marking of the hammock suspension flap pattern on the skin. De-epithelialization and preparation of an adipodermal suspension flap. Excision of excessive glandular–adipose tissue below the suspension flap. Dissection of the superomedial pedicle.
Medial and lateral adipocutaneous-glandular excision according to the Wise-pattern.
Folding of the suspension flap around the pedicle to form a hammock (Figure 2a). Patient in half sitting position. Approximation of the inverted T adipocutaneous flaps. Positioning of the pedicle central on the thoracic wall until the desired breast shaped has been formed. Fixation of the dermal sling to the pectoralis fascia (Figure 2b) with non-absorbable Prolene 3–0 sutures.
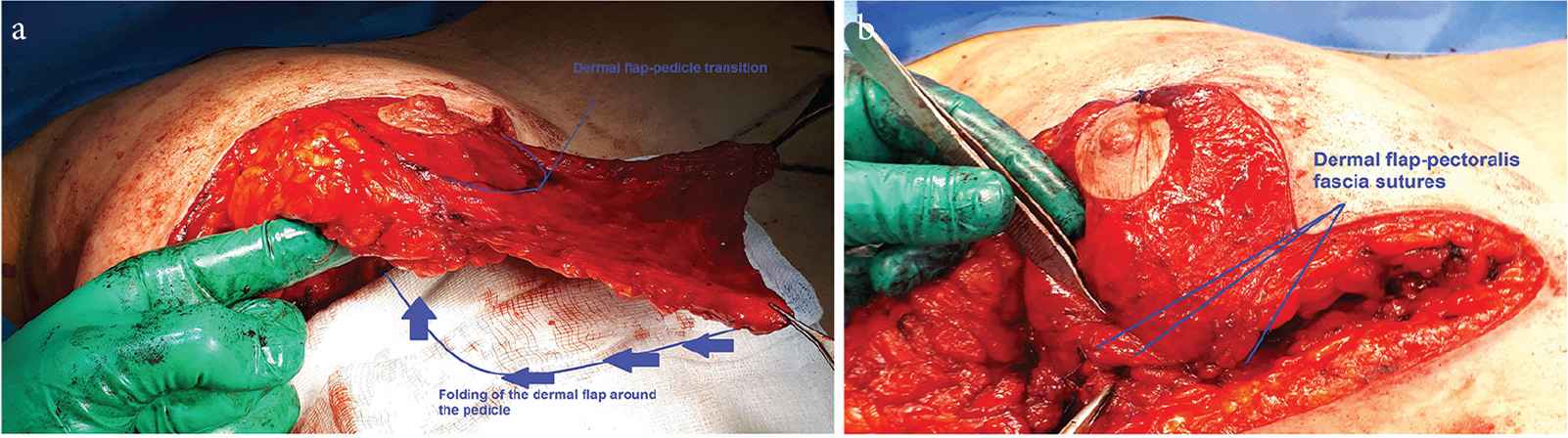
(a) Perioperative. The dermal flap dissection has been completed and will be folded around the pedicle to provide a hammock type suspension flap. (b) Perioperative. The dermal flap is folded around the pedicle. The dermal flap has been sutured to the pectoralis fascia with non-absorbable sutures.
Fixation of the inverted T adipocutaneous flaps to the pectoralis fascia with Prolene 2–0 suture.
Scarpa fascia–pectoralis fascia sutures with Prolene 3–0 at the level of the IMF. Liposuction at the lateral and axilla areas. Deep dermal sutures with PDS 3–0 and 4–0. Intradermal sutures with Monocryl 4–0.
Marking of the desired nipple position. Marking of the new nipple–areola complex with a circular diameter of 4.5 cm.
Medial de-epithelialization of the new circular areola and full-thickness excision of the lateral circular area.
Cranial transposition of the pedicle and transposition of the nipple into the circular defect. Circular deep dermal sutures with PDS 4/0 and an intradermal suture with Monocryl 5–0.
Application of 3M Steri-Strips, Fucidin intertulle gauze, and Tegaderm with pad dressings at the sutured areas with an opening at the nipple–areola complex to evaluate the vascularity. Fixation of the breasts with supportive 3M Microfoam tape.
3. RESULTS
We used the dermal suspension technique of the superomedial pedicle technique in three surgical cases (Figures 3 and 4). All dermal suspension flaps and pedicles were vital. One patient had a small dermal skin abscess caudal from the right areola as a tissue reaction on the remaining suture. The other peri and postoperative cases were uncomplicated. The dressings and supportive foam tape were removed 5 days after the operation. Postoperative histopathology evaluation of the resected breast tissue was performed for all operated cases. Two patients experienced 2-week postoperative pain in the areas treated by liposuction. There was no reduced or increased sensibility of the nipple–areola complex. A supportive breast garment was advised for 6 weeks. The mean follow-up time was 3 months. Meanwhile, no signs of (pseudo)ptosis were seen. Patient satisfaction rate was high, and all patients indicated that they would recommend the procedure to their relatives or friends. One patient had only a telephone consultation follow-up as she left the country without a postoperative picture.
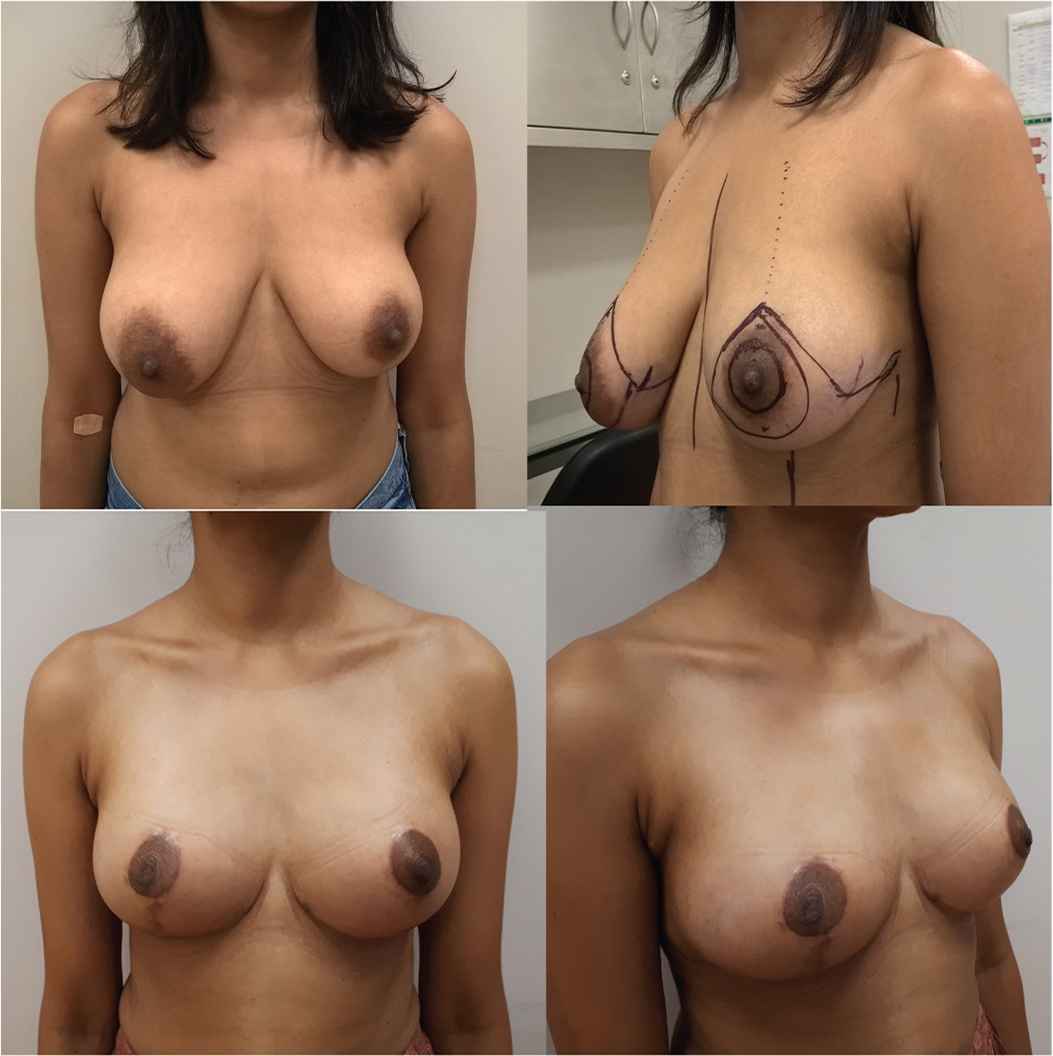
Pre and postoperative evaluation, patient 1. A 32-year-old patient with prominent breast asymmetry and volume difference. At 3 months after operation, some breast edema is still present at the left breast. The patient had a small dermal skin abscess caudal from the right areola as a tissue reaction on the remaining suture.

Pre and postoperative evaluation, patient 2. A 51-year-old obese patient with prominent breast ptosis and asymmetry. At 4 months after operation, small medial dog ears (which retract in most cases within 6 months after the surgery) were noted. The patient did not request any additional corrections.
4. DISCUSSION
Ptosis of the breasts in the postoperative phase after a breast reduction is associated with caudal displacement of the breast tissue below the IMF (bottoming out) with a prominent cranial appearance of the nipple–areola complex on the breast.
The development of (pseudo)ptosis is explained by the skin-only support of the adipose–glandular tissue after a Wise-pattern breast reduction.
Additional techniques that can be used to support the adipose–glandular tissue and prevent further postoperative ptosis consist of the following:
- •
Scarpa fascia sutures to the pectoralis fascia at the IMF.
- •
Fixation of the inverted T point to the pectoralis fascia or rib periosteum. The latter technique is associated with more postoperative pain.
- •
Dermal straps to the pectoralis muscle [3].
- •
Glandular-subcutaneous sutures [4].
- •
Pedicle suspension and plication in the pectoral fascia [5].
- •
Circular non-absorbable dermal sutures with glandular shaping [6].
- •
- •
Dermal suspension flaps.
Bottoming out has been described in the literature especially for the inferior pedicle technique. By using the inferior pedicle, the surgeon relies on the skin envelope to hold up the weight of the breast tissue and pedicle. Many surgeons create a short, tight lower pole to help prevent early bottoming-out [1].
A prominent superomedial pedicle in a Wise-pattern breast reduction forms a prominent weight on the surrounding superior skin and breast tissue. The first two additional techniques described above are based on skin support only of the pedicle. Pedicles with a substantial amount of adipose tissue may lack supportive tissue to be fixated to the pectoralis fascia with gradual loss of support.
Dermal flaps form an additional supportive structure for the adipose–glandular tissue.
Dermal suspension flaps in breast reduction have been described for the inferior pedicle technique and for the superomedial pedicle technique [9,10]. A laterally dermal fascial flap has been described for the superomedial pedicle, independent from the pedicle with caudal support of the pedicle [10]. The lateral dermal fascial flap technique showed higher patient satisfaction for patients who underwent dermo-fascial suspension to the chest wall compared with a classic superomedial pedicle without suspension. Significant differences in terms of suprasternal notch–nipple and nipple–IMF distances were seen among both groups [10].
Our technique describes a direct support of the pedicle using a non-interrupted dermal suspension flap that continues with the pedicle. The suspension flap has a medial, caudal, and lateral support of the pedicle. The dermal sling reduces the anterior force generated by the pedicle. The pedicle enfolded by the dermal flap forms a vital basis for ingrowth in the surrounding tissue.
Our study was limited to three surgical cases. An additional analysis between a control group (without the dermal suspension) and the dermal suspension group is necessary to evaluate potential significant statistical differences. A longer follow-up time is necessary to evaluate the long-term effects as our study had an average follow-up period of 3 months.
5. CONCLUSION
The hammock dermal suspension for the superomedial pedicle in a Wise-pattern breast reduction is a reproducible and promising technique to prevent (pseudo)ptosis of the operated breasts.
CONFLICTS OF INTEREST
The author declares they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
ML was responsible for the development of the described technique, writing of the original manuscript and has performed the procedures mentioned in the manuscript. AT evaluated and peer reviewed the manuscript.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Martain Loonen AU - Adnan Tahir PY - 2019 DA - 2019/09/27 TI - Modification of the Superomedial Pedicle in Wise-pattern Breast Reduction: New Sling Suspension Technique to Prevent (Pseudo)ptosis JO - Dr. Sulaiman Al Habib Medical Journal SP - 77 EP - 80 VL - 1 IS - 3-4 SN - 2590-3349 UR - https://doi.org/10.2991/dsahmj.k.190916.001 DO - 10.2991/dsahmj.k.190916.001 ID - Loonen2019 ER -
