A Large Solitary Fibrous Tumor of the Pleura Associated with Massive Pleural Effusion: A Case Report and Review of the Literature
Peer review under responsibility of the Dr. Sulaiman Al Habib Medical Services Group Company
- DOI
- 10.2991/dsahmj.k.190527.001How to use a DOI?
- Keywords
- Doege–Potter syndrome; pleural effusion; pleural neoplasm; solitary fibrous tumor
- Abstract
Solitary fibrous tumor of the pleura (SFTP) is one of those rare thoracic tumors, especially large tumors occupying most of the thoracic cavity. We report a case of a 45-year-old female who presented with progressive shortness of breath, cough, and palpitation with minimal exertion. The patient was diagnosed to have pulmonary tuberculosis and was given treatment over 6 months before she was referred to our hospital with increasing dyspnea and high output pleural drainage via a thoracostomy tube. Pleural fluid analysis and true cut needle biopsy failed to confirm both previous and current diagnoses. Computed tomography (CT) of the chest showed a large left intrathoracic mass pushing the mediastinal structures to the right side of the chest. A bronchoscopy and explorative thoracotomy showed that the left pleural cavity was occupied by a large mass with multiple adhesions to the chest wall and the diaphragm. The patient underwent a successful removal of a tumor having a mass of 2.3 kg, with an uneventful postoperative recovery; the final histopathology confirmed a solitary fibrous tumor. We are reporting this case because of its rarity and benign histopathology despite the large tumor size. Only a few cases of tumor with such a large size and unexplained high output pleural effusion have been reported so far.
- Copyright
- © 2019 Dr. Sulaiman Al Habib Medical Group. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Solitary Fibrous Tumor of the Pleura (SFTP) is a very rare mesenchymal tumor; it was first described by Wagner in 1870, and was subsequently classified in 1930 as a new disease affecting the pleura. SFTP can affect both pleural layers, but the visceral pleura is the most common site [1].
The tumor, which can vary in size, rarely occupies most of the pleural cavity and could be localized or diffuse [2]. The onset of illness can be completely asymptomatic, and the tumor is usually discovered incidentally; more commonly, however, patients present with respiratory symptoms, including severe respiratory distress. In rare cases, the tumor can present with significant metabolic derangement such as hypokalemia and hypoglycemia, collectively known as Doege–Potter syndrome [3,4]. Most solitary fibrous tumors are benign, and only 20% are not [5]. En bloc resection is the standard treatment for both benign and malignant SFTPs; however, close follow-up is mandatory in all cases, especially when dealing with large tumors.
2. CASE REPORT
A 45-year-old female patient was referred to our institution with a 4-month history of progressive dyspnea and a high output pleural effusion draining (700–1000 ml/day) of serous fluid through the thoracostomy tube. She was recently diagnosed as having pulmonary tuberculosis and has been undergoing treatment for the past 6 months. Her medical and social history did not reveal any significant detail.
On physical examination the patient was dyspneic, with distended neck veins and no palpable cervical lymphadenopathy. Her vital signs were as follows: blood pressure, 130/80 mmHg; heart rate, 100 beats/min; respiratory rate, 33 breaths/min; and temperature, 37°C. The respiratory system examination revealed a deviated trachea to the right, and absence of air entry on the left side of the chest. Results of the hematological analysis showed normal findings and her Erythrocyte Sedimentation Rate (ESR) was 17 mm/h. The pleural fluid analysis suggested an exudative effusion with lymphocytes predominance. Pleural fluid acid fast bacilli staining and cytology yielded negative results.
The chest X-ray scan showed a homogenous opacity occupying the left hemithorax pushing the trachea and meditational structure to the right Figure 1. Chest computed tomography (CT) revealed a large heterogeneous mass occupying the left thoracic cavity Figure 2a, displacing the surrounding meditational structures and the trachea to the right, and pushing the diaphragm down Figure 2b, and a collapsed left lung.
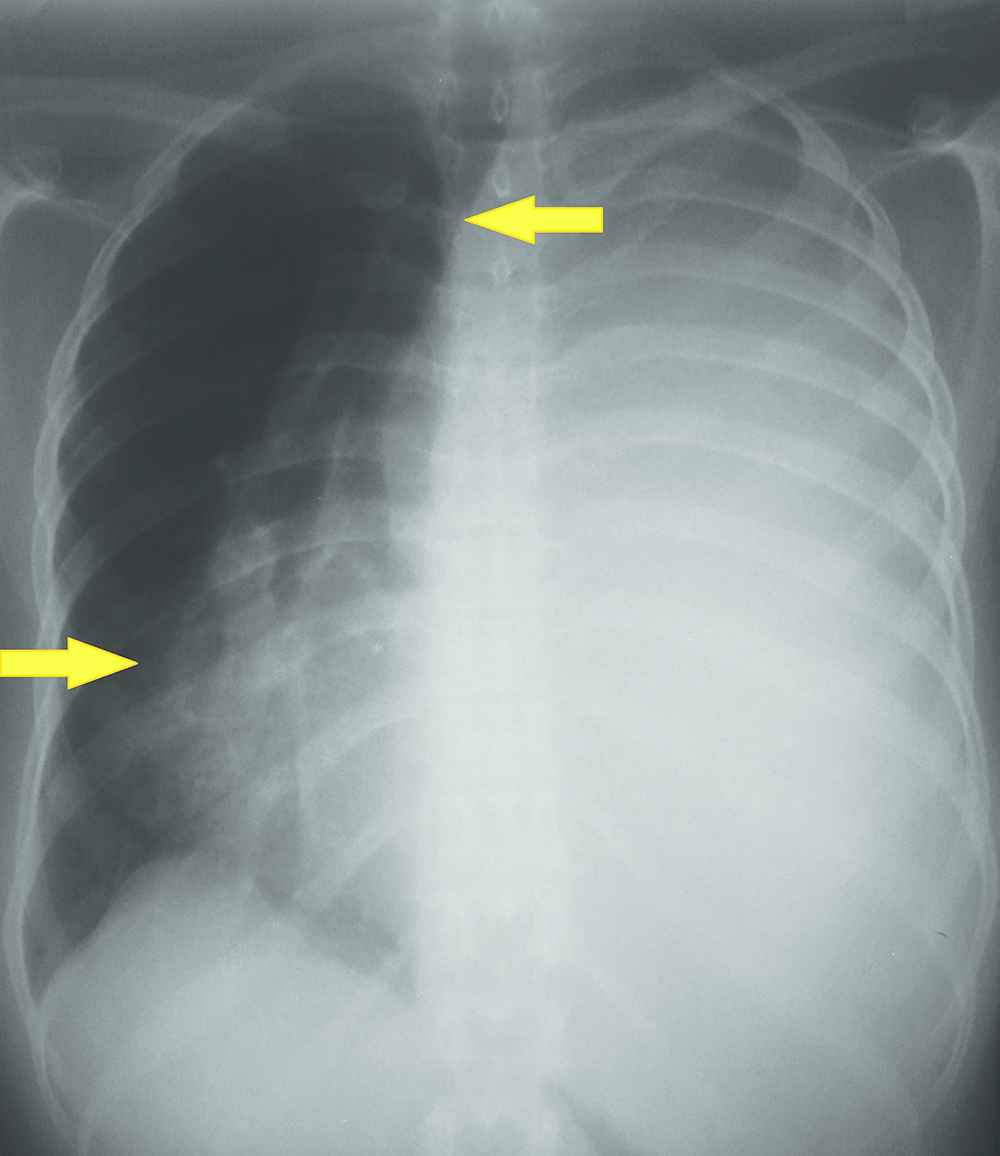
On admission chest X-ray (CXR) showing homogenous opacity occupying left hemithorax with tracheal and mediastinal right shifting (arrows).
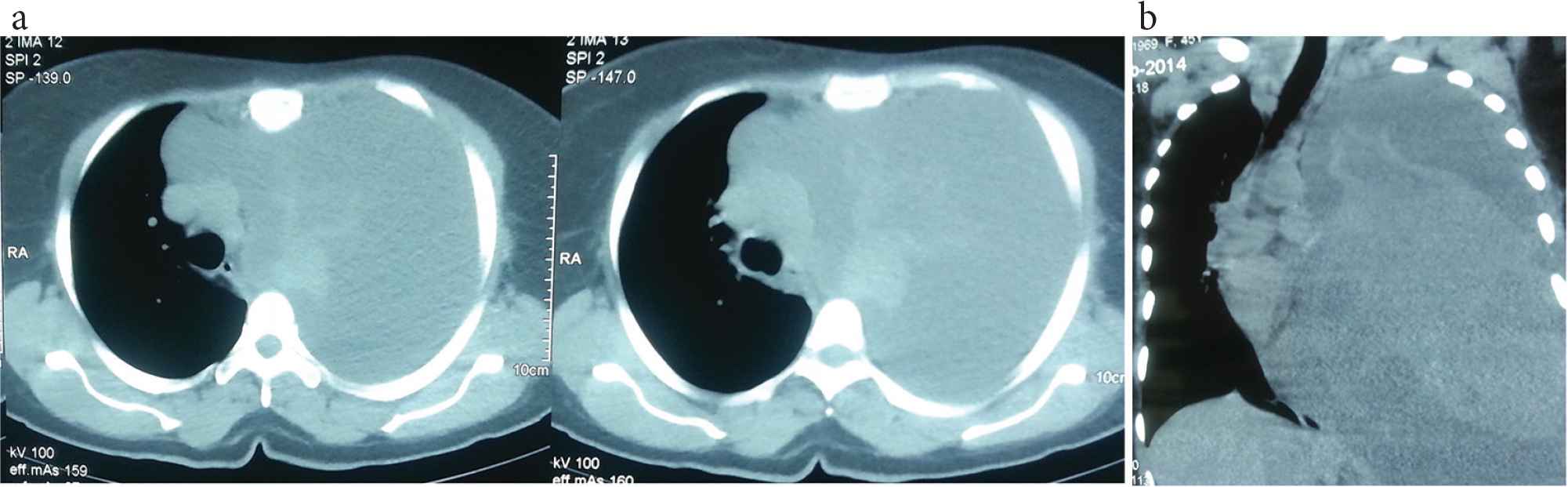
Chest computed tomography (CT). (a) Plane chest CT reveals a huge heterogeneous mass occupying the left pleural cavity. (b) Coronal view shows displaced mediastinal structures and compressed left hemidiaphragm.
Abdominal and pelvic ultrasonography result was normal. Fiber-optic bronchoscopy confirmed the absence of endobronchial lesion, and showed externally compressed left main and segmental bronchus. Bronchial wash and brush cytology was negative for malignant cells. A CT-guided biopsy was performed on two different sites of the mass. The histopathology revealed fibromyxoid tissue with area of hyalinization with inflammatory infiltration and no malignant or atypical cells, with no clear diagnosis.
The patient was prepared for explorative thoracotomy with a double-lumen endotracheal tube; while the patient was placed in the right lateral decubitus position, a sudden drop in blood pressure took place which necessitated adjusting the position and the use of vasoactive drugs to support blood pressure. This hypotension could have been caused by impaired venous inflow, a result of mass effect on the superior and inferior vena cava. Through a classical left posteriolateral thoracotomy and via the fifth intercostal space, we identified the large mass occupying the thoracic cavity from the apex to the diaphragm. A blunt dissection of the anterior surface of the mass was performed, but there was no room to release the mass from the apex, diaphragm, and mediastinal surface; therefore, we performed a partial excision of the mass from its lower part to gain more room to mobilize the mass completely and release all the adhesions. This allowed us to identify the tumor’s origin from the mediastinal visceral pleura. After the total excision of the tumor mass (19 × 18 × 27 cm3), which weighed 2.3 kg, we were able to gradually inflate the lung. Two chest drains were left in the pleural cavity, and the patient received mechanical ventilation in the intensive care unit for 24 h to allow complete expansion of the lung. On the following day, the patient’ was extubated, and the chest X-ray showed a fully expanded left lung Figure 3.
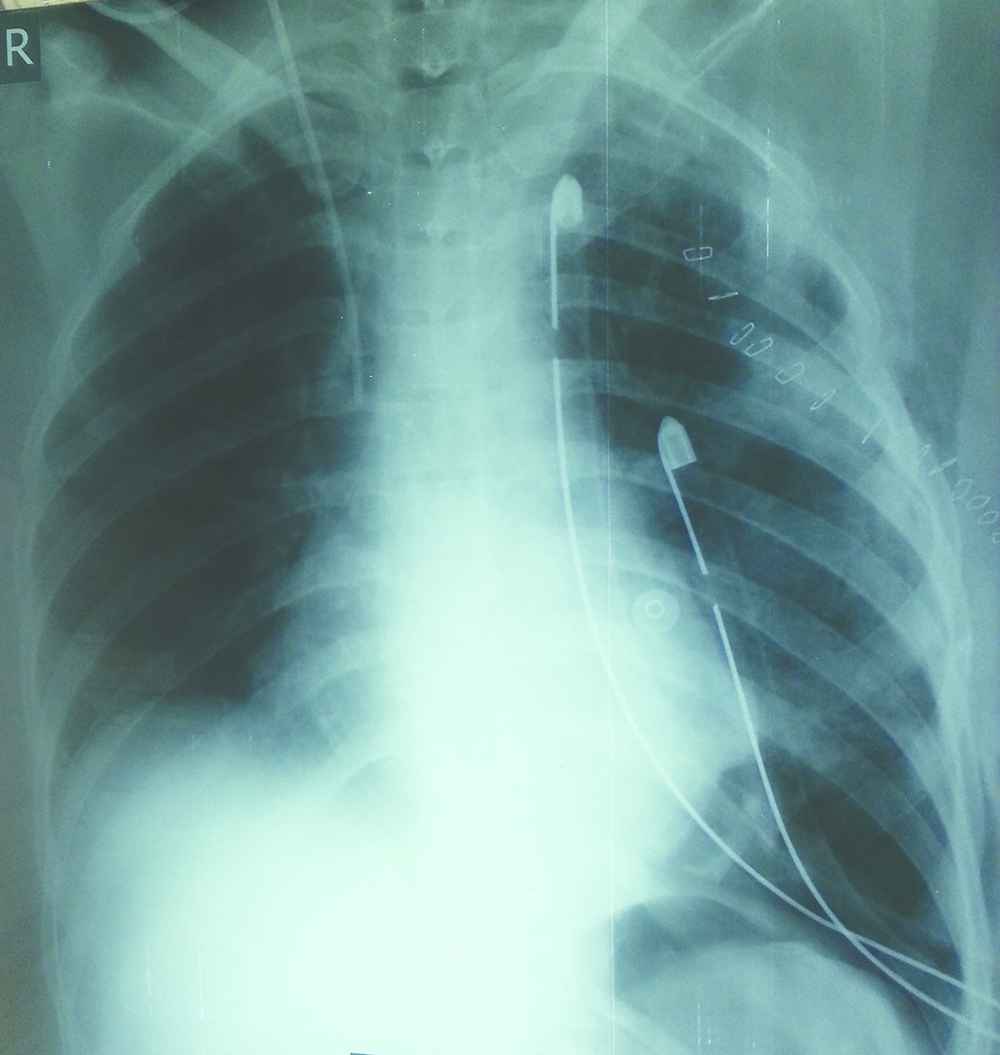
Chest X-ray (CXR). Twenty-four hours post-operation CXR shows full expanded left lung with two chest tubes.
The postoperative period was uneventful, and the patient was discharged home on the 5th postoperative day after the removal of both chest tubes.
The histopathology report confirmed the diagnosis of benign SFTP Figure 4. During the 4-year follow-up, the patient was asymptomatic, and the chest X-ray scan was normal. The patient was then scheduled to undergo chest X-ray and CT scan of the chest every 2 years to screen for late recurrence.
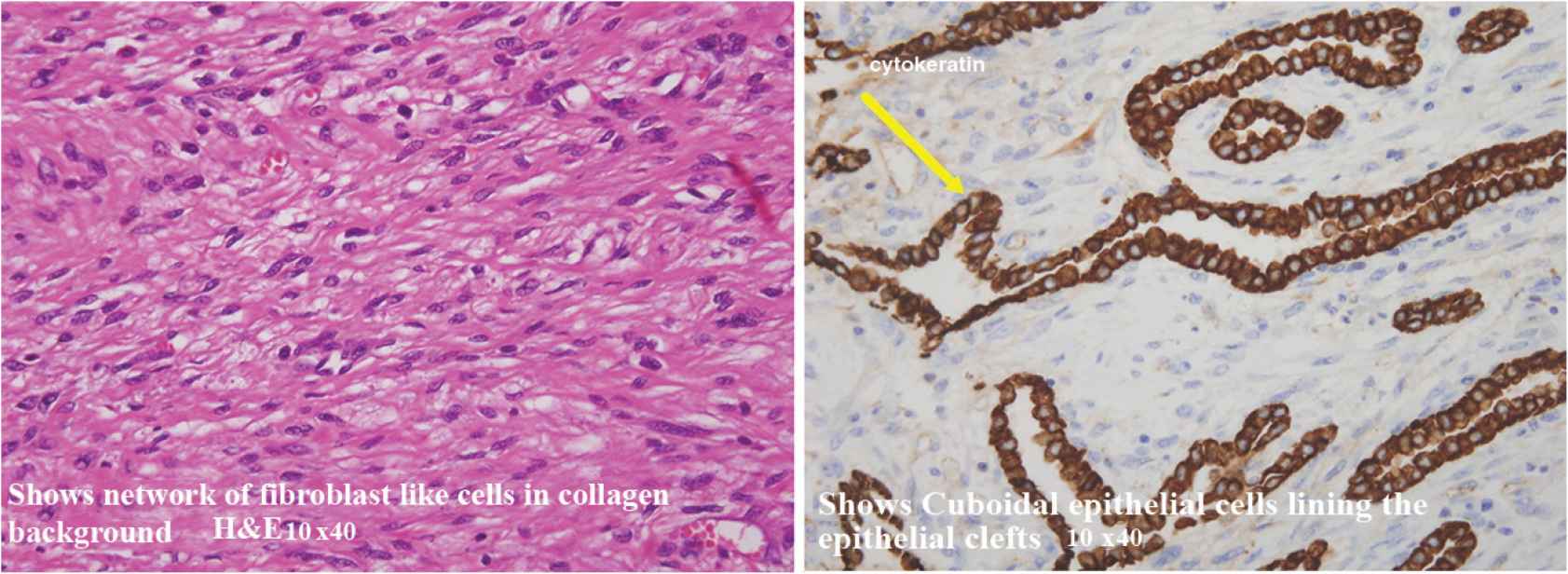
Pathology slides. Two pictures show the pathological findings of the tumor confirming the diagnosis as solitary fibrous tumor of pleura.
3. DISCUSSION
Solitary fibrous tumor of the pleura is a rare neoplasm; it was originally named fibrous mesothelioma, pleural fibroma, and localized mesothelioma [6].
There are no known occupational or environmental factors associated with SFTP, but genetic components have been reported in one case [7]. Out of 800 reported cases, the tumor was benign in 80% of cases; the remaining 20% were malignant or undifferentiated [6,8,9].
There are several criteria used to confirm the malignant potential of the tumor: abundant cellularity, increased mitotic activity (>4 mitotic figures/10 high power fields), cytonuclear atypia, and a tumor size greater than 10 cm [8,10]. In our case report, despite the large size of the tumor (19 × 18 × 27 cm3) and the large pleural effusion, the histopathology report confirmed the diagnosis of benign SFTP. However, the patient will require long-term follow-up because of the unpredictable behavior of the SFTP. To date, there are no certain morphological characteristics that predict a poor prognosis of SFTP [11–13]. The usual age at diagnosis is 60 or 70 years, and it occurs in similar frequency in both sexes [3]. Our patient is a female in her forties with a large amount of serous pleural effusion, although existing case series report pleural effusion in less than 10% of cases; furthermore, some studies suggest an association with malignant potential [5,14]. Usually patients with SFTP are a symptomatic, especially those with small tumors. Respiratory symptoms are the most common presenting symptoms. Other rare features include osteoarthropathy, clubbing, and hypoglycemia, which is caused by the release of insulin-like growth factor 2 [15–17].
The tumor is usually discovered incidentally on chest X-ray or CT scan of the chest. The radiological feature on CT scan is usually a well-circumscribed mass with homogenous density; however, it could also be of heterogeneous density in very large tumors similar to that in our patient, and usually shows adhesions and tumor infiltration. Positron emission tomography adds little to the evaluation of this tumor; for example, in three cases, two had no fluorodeoxyglucose (FDG) uptake whereas one had a minimal uptake [18]. CT-guided biopsy is controversial because, as shown in this case report, the accuracy is questionable as SFTPs involves varying degrees of cellular areas [19,20]. Surgical resection with histological free margins is the standard treatment for SFTP including different types of resection, which could be achieved by video-assisted thoracic surgery for small tumors and by open thoracotomy for large tumors [21]. Redo surgery for local recurrence for more than one time after complete resection can occur and after variable lengths of time such as up to 20 years after the primary excision [22,23].
Adjuvant and neoadjuvant modality of treatment had been used in a limited number of cases in local recurrence using chemotherapy, radiotherapy, or a combination of both [22].
4. CONCLUSION
Although SFTP is a rare type of tumor, there have been a few cases reported involving large SFTPs similar to that found in our patient. The tumor has variable presentations and radiological findings, and needle biopsy is not always with positive results for diagnosis. Surgical excision is the mainstay of treatment. The unpredictable behavior of these tumors (even if they are benign) mandates a regular follow-up for all patients with SFTP to ensure early detection and treatment of the recurrence of the tumor.
CONFLICTS OF INTEREST
The authors report no conflicts of interest, and no funding was received to support this work.
REFERENCES
Cite this article
TY - JOUR AU - Hussein Ahmed Lateef AU - Mutaz I.K. Fakhry Al-Khateeb PY - 2019 DA - 2019/06/30 TI - A Large Solitary Fibrous Tumor of the Pleura Associated with Massive Pleural Effusion: A Case Report and Review of the Literature JO - Dr. Sulaiman Al Habib Medical Journal SP - 8 EP - 11 VL - 1 IS - 1-2 SN - 2590-3349 UR - https://doi.org/10.2991/dsahmj.k.190527.001 DO - 10.2991/dsahmj.k.190527.001 ID - Lateef2019 ER -
