Neonatal Mortality in a Tertiary Care Private Set Up in Saudi Arabia
Peer review under responsibility of the Dr. Sulaiman Al Habib Medical Services Group Company
- DOI
- 10.2991/dsahmj.k.190521.002How to use a DOI?
- Keywords
- Congenital anomalies; neonatal mortality; private medical care; Saudi Arabia; sociodemographic index
- Abstract
To ascertain Neonatal Mortality Rate (NMR), Early NMR (ENMR), Late NMR (LNMR), Corrected NMR (cNMR), and causes of neonatal mortality in a major tertiary care private maternity and Neonatal Intensive Care Unit (NICU) set up in Saudi Arabia. This was a retrospective analysis of hospital data. We ascertained 1-year data (from January 1, 2017 to December 31, 2017) from the electronic patient medical records database as well as the annual reports of four tertiary care labor and delivery rooms and NICU’s of Sulaiman Al Habib Medical Group (HMG). We obtained the total number of deliveries and neonatal outcomes and calculated overall NMR, ENMR, and LNMR rates per 1000 live births and stratified them by Sociodemographic Index (SDI). We analyzed the data using Microsoft Excel. The electronic patient records included data on 14,339 deliveries and 14,543 births (including twins and multiple births). We observed a total of 51 neonatal deaths (30: early, 21: late) resulting in NMR of 3.5/1000, ENMR of 2.06/1000, and LNMR of 1.44/1000. The deaths due to futility were 24 (47%), giving a cNMR of 1.8/1000. We found complications of extreme prematurity and congenital anomalies incompatible with life as the two major causes of death in our dataset. There was no death due to perinatal asphyxia. The NMR and cNMR were comparable to the most recent global, regional, and national data. The cNMR of a select population with high SDI served by a major private tertiary care set up was lower than the NMR of the global high SDI group. The high incidence of major and futile congenital anomalies warrants further study.
- Copyright
- © 2019 Dr. Sulaiman Al Habib Medical Group. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Childhood mortality (number of deaths among children younger than 5 years, including neonatal deaths) has declined substantially between 1970 and 2016 [1]. Sustainable Development Goals (SDGs), the new global initiative of the World Health Organization, has set a target of under five mortality rate ≤25 deaths per 1000 live births and a Neonatal Mortality Rate (NMR) ≤ 12 deaths per 1000 live births [2]. All United Nations Member States are expected to achieve these SDG targets between 2016 and 2030 [2]. The countries with high Sociodemographic Index (SDI) had already achieved their target NMR before the launch of the SDG program [1]. This includes six Gulf Cooperation Council countries in the Middle East: Saudi Arabia, Kuwait, Bahrain, Qatar, United Arab Emirates, and Oman. Saudi Arabia has a well-developed healthcare system; both in the public and private sectors. Saudi Arabia’s published national neonatal mortality data are cumulative countrywide data from both public and private hospitals. The country does not have formal and exclusive research-based neonatal mortality data from its private sector. We conducted this research study to fill this gap in knowledge. In addition, we wanted to analyze the contribution of birth defects to NMR in the high SDI population of Saudi Arabia because, along with all other Arab countries, Saudi Arabia is classified as one of the Red Zone countries with highest incidence of birth defects in the world [3].
2. MATERIALS AND METHODS
We conducted this retrospective epidemiological study in four tertiary care maternity units and Neonatal Intensive Care Unit (NICU) of Dr. Sulaiman Al Habib Medical Group (HMG) of hospitals (Al Rayyan Hospital Riyadh, Olaya Hospital Riyadh, Sweidi Hospital Riyadh, and HMG Hospital Al Qassim). HMG is a major tertiary care private sector maternity and NICU set up, accredited by Joint Commission International USA. The Olaya, Al Rayyan, and Al Qassim hospitals have active assisted reproductive units as well. Apart from inborn babies, the HMG NICU also admits outborn babies referred by public and other private hospitals for tertiary care services. Most of our patients are financially sponsored by insurance companies or the Ministry of Health (MOH). Some patients are self-sponsored. Overall, the SDI of the population catered for by HMG is high.
Our study was approved by the HMG Institutional Review Board (Approval No: RC 18.04.02). The data collection was exempted by the IRB from taking individual patient consent. Data for one calendar year (January–December 2017) was collected on preapproved data collection forms from the hospital electronic patient record system (called VIDA, V-0.1) as well as from the monthly and annual reports of the Department of Obstetrics and NICU. All pregnant women admitted in four HMG hospitals and all newborn babies (aged 0–27 days, including twins and multiples), admitted in four HMG NICUs were included in the study. For preterm babies, the Perinatal Neonatal Outcomes Research Study (PEARL Study) criteria of neonatal age adjusted for prematurity were used [4]. Term babies more than 28 days PMA (postmenstrual age) were excluded. None of the deliveries were excluded from the study.
We collected and analyzed our data on Microsoft Office Excel 2010 (Microsoft Corporation, Redmond, WA, USA) and calculated NMR, Early NMR (ENMR), Late NMR (LNMR) and Corrected NMR (cNMR). We compared mortality outcomes with the most recent global, regional, and national neonatal mortality data published by the Global Burden of Disease (GBD) study in 2017 [1].
3. RESULTS
During 2017, the four HMG hospitals conducted a total of 14,339 deliveries and 14,543 births (including twins and multiple births). The electronic patient records of all deliveries and births were analyzed and none was excluded. Deliveries by hospital were: Al Rayyan Hospital, 5471; Olaya Hospital, 3902; Sweidi Hospital, 1608; and Al Qassim Hospital, 3358. The mode of delivery was recorded as 9222 (64.2%) vaginal deliveries and 5117 (35.8%) cesarean section deliveries, including both elective and emergency C-Sections. The total number of births were 14,543 including twins and multiples. Births by hospital were: Al Rayyan Hospital, 5555; Olaya Hospital, 3902; Sweidi Hospital, 1632; and Al Qassim Hospital, 3454. A total of 2884 babies were admitted to the NICU; of these 2457 (85.2%) were inborn while 427 (14.8%) were outborn. Among the inborn deliveries, 16.89% required NICU admission.
We observed a total of 51 neonatal deaths. Deaths by hospital were; Al Rayyan Hospital, 22; Olaya Hospital, 10; Sweidi Hospital, 2; and Al Qassim Hospital, 15. Early neonatal deaths (Days 0–6) were 30 (58.8%) and late neonatal deaths (Days 7–27) were 21 (41.2%). The NMR was 3.5/1000, ENMR 2.06/1000, and LNMR 1.44/1000. The deaths due to futility were 24 (47%); thus, cNMR was 1.8/1000. Among the 24 futile cases, 19 (79% of futile and 37.3 % of all deaths) were on do not resuscitate order. The order was placed in action either ante- or postnatally. The futile cases included trisomies (18 and 13), renal agenesis, Potter’s syndrome, complex congenital heart disease, anencephaly, lissencephaly, complex multisystem dysmorphism, and complications of extreme prematurity (bilateral Grade 4 intraventricular hemorrhage, unventilatable respiratory insufficiency, severe sepsis, and necrotizing enterocolitis).
The NMR and cNMR of our study were comparable to the most recent global, regional, and national data Figure 1. There were 80.4% of deaths among preterm babies (<37 weeks), and 49% of total deaths were among extremely preterm (<28 weeks gestation) babies Table 1. There were 90% of deaths among low birth weight babies (<2500 g), and 43% of total deaths were among extremely low birth weight (≤1000 g) Table 1. Complications of extreme prematurity and congenital anomalies incompatible with life were the two major causes of death Table 1. There was no death due to perinatal asphyxia.
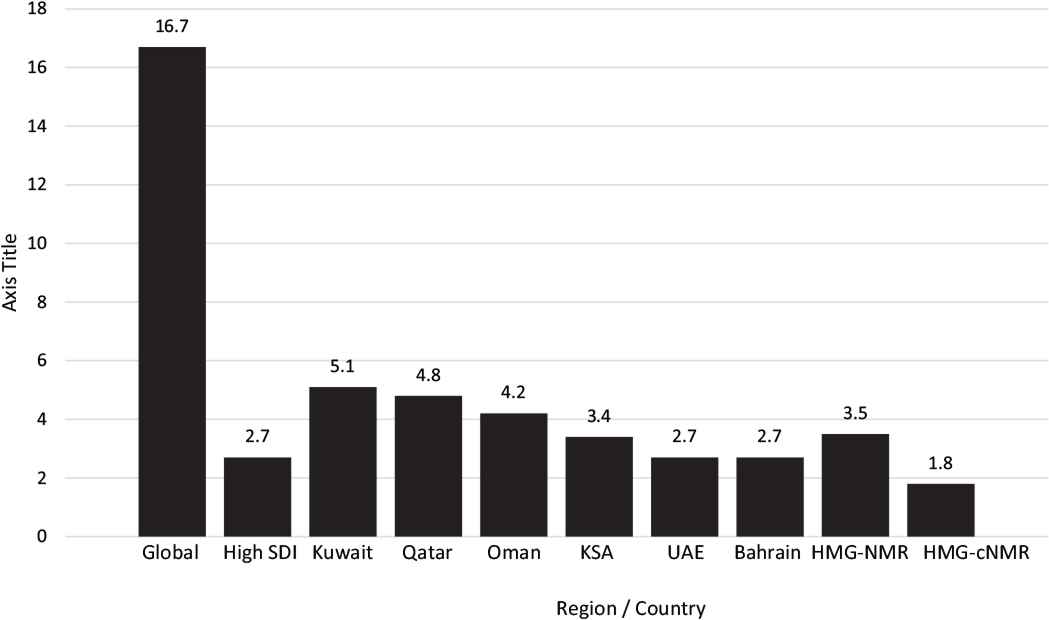
Neonatal Mortality Rates Global*, Regional Countries* and HMG**. *Data Source: GBD 2016 Mortality Collaborators. Lancet 2017; 390: 1084–150. **HMG Data.
| All births (n = 14,543) | Neonatal deaths (n) | Neonatal deaths (%) |
|---|---|---|
| By gestational age (weeks) | ||
| ≤28 | 25 | 49 |
| 29–32 | 11 | 21.6 |
| 33–36 | 5 | 9.8 |
| ≥37 | 10 | 21.6 |
| By birth weight (g) | ||
| ≤1000 | 22 | 43.2 |
| 1001–1500 | 12 | 23.5 |
| 1501–2500 | 12 | 23.5 |
| >2500 | 5 | 9.8 |
| By cause of death | ||
| Prematurity | 24 | 47 |
| Congenital anomalies | 18 | 35.3 |
| Sepsis | 6 | 11.8 |
| Other | 3 | 5.9 |
Distribution of neonatal mortality by gestational age, birth weight, and cause; Al Habib Group of Hospitals, Saudi Arabia, 2017
4. DISCUSSION
Our study reflects that very low NMRs comparable to those in well-developed countries can be achieved in transitional countries as well. The study also supports the notion that establishing electronic health records systems in healthcare facilities provides opportunities to conduct reliable perinatal epidemiological studies. The change from paper-based to electronic health records may be reflective of high standards of care and a good justification of public and private spending on health systems.
Saudi Arabia is the largest oil-producing country in the world, with a high socioeconomic index and gross domestic product per capita of 45,489.83 PPP$. The healthcare system in the country has improved rapidly over recent years [5]. This may be attributed to the increased wealth in the country and the high priority of providing its citizens with high-quality healthcare. The country spends 4.7% of its gross domestic product on health. Government expenditure as a percentage of all healthcare spending is 62.9%, while the remaining is nongovernmental expenditure. The infant mortality rate in Saudi Arabia is 12.5/1000 live births and childhood vaccination coverage (diphtheria–tetanus–pertussis, measles, and Haemophilus influenzae B) is 98% [5]. Due to increasing population size and demands coupled with uncertainty about oil-dependent economies, the government has implemented a new phased plan, which includes the introduction of a cooperative health insurance scheme, closely followed by privatization of the national hospitals [6]. This will increase the size as well as the responsibility of the private sector in sustaining a high-quality healthcare system. HMG [7] is a major private sector healthcare organization in Saudi Arabia that provides comprehensive high-quality tertiary care maternity and NICU services. HMG hospitals are often used by the Ministry of Health (MoH) as an outsource to take over critical patients when the public sector hospitals start running a high census. HMG also caters for patients sponsored by insurance companies as well as rich private patients with high SDI.
Saudi Arabia is one of the 118 countries that have achieved their SDG target of NMR ≤12/1000 [1,8]. The national NMR in Saudi Arabia was 3.4/1000 live births in 2016 Figure 1 [1]. This is comparable to the NMR of high SDI countries (2.7/1000 live births during 2016). The situation is similar in other Gulf Cooperation Council countries: Kuwait, 5.1/1000; Bahrain, 2.7/1000; Qatar, 4.8/1000; United Arab Emirates, 2.7/1000, and Oman, 4.2/1000 [1]. The NMR in our institution (HMG) was 3.5/1000, which is the same as the national NMR in Saudi Arabia. However, 40% of neonatal deaths in our institution were due to futility, which included ante- and postnatally diagnosed chromosomal and congenital anomalies incompatible with life. In High SDI countries, most of these anomalous fetuses would have been terminated antenatally. However, elective antenatal termination is not a common practice in Saudi Arabia due to strict religious and to cultural believes. We estimated NMR after correction for futility. cNMR was 1.65/1000, which is comparable to many countries with the best NMRs (e.g., Scandinavian countries, Japan, and Singapore) [1].
Sociodemographic index is a composite indicator of development status created by the GBD group of researchers and is used to produce health-related outcomes estimates. SDI is the geometric mean of 0–1 indices of total fertility rate under the age of 25 years (TFU25), mean education for those aged ≥15 years (EDU15+), and log distributed income per capita [9]. As a composite, a location with an SDI of 0 would have a theoretical minimum level of development relevant to health, while a location with an SDI of 1 would have a theoretical maximum level [9]. Based on the SDI, GBD classifies regions in development quantiles; high, high middle, middle, low middle, and low SDI regions. SDI, as used by the GBD study 2016, has emerged as a good predictor of the health-related SDG index (r² = 0.88) [1]. High SDI regions and countries had achieved their SDG targets even before the start of the SDG era. The NMR in 2016 was lowest in high-SDI regions (2.7/1000 UI 2.5–29/1000). The SDI of Saudi Arabia is 0.77, which is in the high quantile. According to our study, the NMR in a single major private group of hospitals in Saudi Arabia was 3.5/1000 and cNMR was 1.8/1000 live births in 2017. Patients attending private hospitals in Saudi Arabia are either wealthy and from high-socioeconomic-status families, or they are high-profile employees sponsored by good insurance companies or MoH. There is an inverse relationship between socioeconomic status and NMR [10]. Therefore, it is not a surprise that the NMR of high-standard private hospitals in Saudi Arabia is comparable to that of some high-SDI countries.
Neonatal mortality increases with decreasing gestational age at birth and decreasing weight at birth. The lower the gestational age and birth weight, the higher is the mortality [11,12]. Babies weighing <1500 g have a mortality risk at least 100-fold higher than those with an optimal weight (weight associated with lowest mortality) [13]. Our study confirmed the same pattern of neonatal mortality with respect to birth weight and gestational age Table 1: 80% of deaths were in preterm babies (<37 weeks gestation) and 49% of total deaths occurred in extremely preterm babies (≤28 weeks gestation). With regards to birth weight, 90% of deaths occurred in low birth weight babies (<2500 g) and 43% occurred in extremely low birth weight babies (≤1000 g). The association between birth weight and mortality is the strongest in epidemiology [13].
Worldwide prematurity, intrapartum asphyxia, and sepsis are responsible for 13.7%, 11.2%, and 5.3% of mortality in children aged <5 years, respectively [14]. Similarly in the Middle East and North Africa, the figures are 21.9%, 12.5%, and 6.9%, respectively [14]. Another recent study on NMR in the Eastern Mediterranean Region [10] also estimated prematurity (34%), asphyxia (24%), and sepsis (18%) as the three major causes of neonatal mortality, and congenital anomalies as the fourth most common cause (10%). However, the pattern of cause of neonatal mortality in our data was different Table 1. Prematurity was the number one cause of neonatal mortality, responsible for 47% of neonatal deaths, and sepsis the third most common cause of neonatal mortality, responsible for 11.8% of neonatal deaths. However, we did not have any deaths due to intrapartum asphyxia. Instead, congenital anomalies were the second most common cause of neonatal mortality, responsible for 35.3% of neonatal deaths. The pattern of neonatal deaths was similar in a recent study from Qatar [11]. The first four most common causes of neonatal mortality were prematurity (44.78%), lethal congenital malformations (26.5%), sepsis (19.15%), and asphyxia (3.25%) [11].
Arab countries including Saudi Arabia have some of the highest incidences of birth defects in the world and are placed among the red zone countries [3]. Sudan with a birth defects rate of 82/1000 is top of the red zone countries followed by Saudi Arabia (81.3/1000), United Arab Emirates (75.9/1000), Kuwait (74.9/1000), Bahrain (73.4/1000), and Qatar (73.4/1000). One possible reason for this high incidence of lethal congenital anomalies may be a high incidence of inbreeding, which is a norm in the tribal style Arab world. Consanguinity, with its known association with preterm births, congenital anomalies, and reproductive wastage, has an incidence of 40–70% in the Arab region [15,16]. The issue of high incidence of congenital anomalies is an important topic for future perinatal research in the Arab region. Our study data also reveals that despite being in the red zone for birth defects, NMR in Saudi Arabia is at par with other populations with similar SDI; underscoring the success of the healthcare system in Saudi Arabia.
Neonatal mortality rate and cNMR of a select high-income, socially well-placed population seeking healthcare in a major high standard private tertiary care set up in Saudi Arabia are comparable with the NMR of high-SDI countries. A strong well-funded equitable healthcare system can achieve low NMRs when deaths due to futility are disregarded. The high incidence of major and futile congenital anomalies as a major cause of neonatal deaths warrants a well-designed and well-funded perinatal study at the national and regional level. The results of our study represent the outcomes of a socioeconomically wealthy population that can afford healthcare in a high-profile private hospital. The results do not represent the population in general and may not be extrapolated as the national data.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
ACKNOWLEDGMENTS
We are grateful to the data collection team: Olaya, Mary Grace; Al Rayyan, Mohamed Kamal; Sweidi, Reinne Maatouk and Konstantinos Mousafeiris; Qassim, Muhammad Hasan Abdulghani; and Jasim Anabrees for critical analysis of the data and manuscript.
REFERENCES
Cite this article
TY - JOUR AU - Sajjad Ur Rahman AU - Muhammad Hasan Abdulghani AU - Khalid Al Faleh AU - Jasim Anabrees AU - Mohammad Khalil AU - Konstantinos Mousafeiris AU - Mustafa Mohammad Mustafa AU - Maha Yassin Mansour AU - Adnan Mirza AU - Mohammad Mubarak AU - Mohamed Kamal PY - 2019 DA - 2019/06/30 TI - Neonatal Mortality in a Tertiary Care Private Set Up in Saudi Arabia JO - Dr. Sulaiman Al Habib Medical Journal SP - 16 EP - 19 VL - 1 IS - 1-2 SN - 2590-3349 UR - https://doi.org/10.2991/dsahmj.k.190521.002 DO - 10.2991/dsahmj.k.190521.002 ID - UrRahman2019 ER -
