Prevalence of Nonadherence to Antihypertensive Medications among Adults Attending Primary Healthcare Clinics in Al-Hasa Region: A Cross-Sectional Study
Peer review under responsibility of the Dr. Sulaiman Al Habib Medical Services Group Company
- DOI
- 10.2991/dsahmj.k.190516.001How to use a DOI?
- Keywords
- Antihypertensive drugs; hypertension; nonadherence; prevalence
- Abstract
To assess the prevalence of nonadherence to antihypertensive medications among adults attending Primary Healthcare Clinics (PHCs) in Al-Hasa Region. This cross-sectional study included participants from a variety of clinics in the region and each of them had been interviewed to complete the questionnaire. The participants were selected by random sampling from eight different PHCs. Data were collected by a structured questionnaire that was adopted from two different scales to determine the association between adherence and socioeconomic and health status characteristics. We included 372 participants with a mean (±standard deviation) age of 53 ± 12.4 years and most of them were male (62%, n = 231). The overall mean adherence based on our adapted scale was 5.3 ± 2.3. Among participants taking more than six medications, the percentage of nonadherent participants was significantly higher than the percentage of adherent participants (85% vs. 15%, p = 0.016). Participants with single comorbidity were more likely to be adherent than patients with multiple comorbidities (odds ratio = 1.52, p = 0.049). In conclusion, we found a high prevalence of nonadherence to antihypertensive medications in the Al-Hasa community and the main association factor was found to be the presence of comorbidity. Such high rate sends alarming messages for the need of potential interventions to improve adherence outcome.
- Copyright
- © 2019 Dr. Sulaiman Al Habib Medical Group. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Hypertension contributes to a huge burden of cardiovascular disease, renal failure, and stroke, leading to early disability and high mortality. There are many people undiagnosed with hypertension because it rarely causes symptoms at an early stage [1].
Hypertension and its treatment is not only a national concern but also an international public health issue that needs more attention. In 2014, the prevalence of hypertension worldwide in adults was around 22%, and that was responsible for 9.4 million deaths [2]. In Saudi Arabia, the prevalence of hypertension in adults was reported to be 21% in 2016 [3]. In addition, cardiovascular diseases account for around 46% of mortality rate in Saudi Arabia, but 24% of this rate is attributed to hypertension [2,4].
Poor adherence to hypertensive medications is a major factor for poor disease control and subsequently poor clinical outcome, including hospitalization and mortality, worldwide and in Saudi Arabia [5–7]. Despite the fact that medical treatments for hypertension are effective, a survey conducted between 2003 and 2004 in the United States (US) showed that only 37% of hypertension cases were reported to have their blood pressure controlled [8]. A systematic review and meta-analysis of the medical literature have shown a significantly higher rate (45.2%) of medication noncompliance, particularly among those with uncontrolled blood pressure (83.7%). Also, the percentage of nonadherence was lower in men (46.2%) than in women (53.9%) [9]. Conducted between 2012 and 2016, other surveys in the Middle East showed that 36.2–50.5% of participants had high adherence rate, 26.8–27.1% had medium adherence rate, and 22.4–36.8% had low adherence rate to hypertensive medications [10,11]. The most common three risk factors for nonadherence to antihypertensive medications are global satisfaction of treatment, effectiveness of therapy, and complexity of medication prescription [5,6]. Age is a crucial factor. According to a survey conducted between 2011 and 2012 in New York City, USA, the prevalence of adherence to antihypertensive medications among older adults (≥60 years, 34%) was higher than in younger adults (<60 years, 24.5%) [12]. Al-Hasa Region represent 24% of the total area of Saudi Arabia and it has a high population. To our knowledge, no study in Al-Hasa Region has investigated the prevalence of adherence to antihypertensive medications among hypertensive patients.
Accordingly, our aim in this study was to assess the rate of nonadherence to antihypertensive medications among adult hypertensive patients attending Primary Healthcare Clinics (PHCs) in the Al-Hasa Region.
2. MATERIALS AND METHODS
2.1. Study Design
Our study was a cross-sectional quantitative study. The study was conducted in a primary healthcare setting in Al-Hasa Region, Saudi Arabia where up-to-date medical care is provided.
Our study population was adult hypertensive patients who attended PHCs in Al-Hasa Region between January and March 2018. Our inclusion criteria were patients who were diagnosed with hypertension, aged ≥18 years, and from any nationality. Our exclusion criteria were prehypertensive patients, pregnant women, and any patients with known mental disorder.
Random sampling was used to select eight different PHCs among around 60 in Al-Hasa Region. The attending general physician identified eligible participants during the study period. After obtaining patient approval, a member of the research team met patients in a private area to obtain consent first then completed the questionnaire. We used the convenient sampling technique to enroll patients in the study and determine the blood pressure control based on the National Institute for Health and Care Excellence Guidelines – 2011, which determine the target blood pressure reading for most hypertension patients to be <140/80 mmHg [13]. The minimum sample size was determined for a single proportion and found to be 310 [14].
2.2. Data Collection and Analysis
Adherence was assessed by self-reporting questionnaire. The questionnaire items were adopted from a questionnaire such as Assessment of Opioid Taking Behaviors and Adherence (AOTBA) scale and Morisky Medications Adherence Scales Eight Questions (MMAS-8), to determine adherence [15,16]. This scale included Yes/No questions, where No = 1 and Yes = 0; however, the fifth question consisted of yes equaling 1 point. The last question included five options from A to E, with A = 1, B = 0.4, C = 0.3, D = 0.1, and E = 0 points. The score of all positive answers (Yes) determined the degree of adherence. It was suggested in this scale that high adherence level scored 8, medium adherence level scored 6 to <8, and low adherence level scored 1 to <6 [16]. However, for the purpose of simplifying the interpretation of the analysis, we divided the degree of adherence into two groups rather than three (high, medium, and low); nonadherent (scored < 6) and adherent or appropriate adherence level (scored ≥ 6). Additionally, we assessed sociodemographic characteristics (gender, age, marital status, residence, level of education, income, and job) and health status characteristics (blood pressure status, number of medications, duration of disease, ≥2 comorbidities, and family history of hypertension). For the characteristic related to the number of comorbidities, we included only chronic disease such as coronary artery diseases, diabetes, thromboembolic disorders, and asthma. Data collection technique was self-report using a structured questionnaire.
Data analysis included determination of sociodemographic and health status information, respondent level of adherence, and factors associated with adherence to hypertensive medications. Descriptive and inferential statistics included mean and standard deviation, t-test for continuous data, and frequencies and χ2-test for categorical data. Crude and multiple logistic regression analysis was used to measure the odds ratio at the level of significance of p ≤ 0.05. Although some variables were clinically highly associated with nonadherence, we only used forward stepwise regression building analysis for the purpose of building a multiple logistic regression model. For all variables, all the data were complete (i.e., there were no missing data). Data were analyzed using SPSS version 25 (SPSS Inc., Chicago, IL, USA).
2.3. Ethical Considerations
The study was approved by the Institutional Review Board at Kind Saud University College of Medicine, Riyadh, Saudi Arabia (Ref. No. 17/0525/IRB). Also, we had approval from the local administration at the Directorate of Health Affairs Al-Hasa Region, Ministry of Health, Saudi Arabia (Ref. No. 41/26/4/925745). All patients consented to participate in the study.
3. RESULTS
3.1. Sociodemographic and Health Status Characteristics
We enrolled 372 patients and the rate of denial to participation was 1%. The overall mean age was 53 ± 12.4 years and most of the population was male (62%, n = 231). The majority of participants in the study were Saudis (98%, n = 363). Most of the patients were married (83%, n = 309), urban (68%, n = 254), primary school or lower (49% n = 182), unemployed (56%, n = 207), and had income ≤ 5000 Saudi riyal (56%, n = 210). Most of the study population had a family history of hypertension (80%, n = 299) and had ≥2 comorbidities (58% n = 215) Table 1.
| Parameters | Total (n = 372)% (n) |
|---|---|
| Gender | |
| Male | 62 (231) |
| Female | 38 (141) |
| Age group (years) | |
| <50 | 38 (141) |
| ≥50 | 62 (231) |
| Nationality | |
| Saudi | 98 (364) |
| Non-Saudi | 2 (8) |
| Level of education | |
| Primary school or lower | 49 (182) |
| Secondary school | 24 (88) |
| Diploma | 6 (24) |
| Bachelor’s degree or above | 21 (78) |
| Marital status | |
| Single | 6 (23) |
| Married | 83 (309) |
| Widowed | 10 (37) |
| Separated | 1 (3) |
| Residency | |
| Rural | 32 (118) |
| Urban | 68 (254) |
| Job status | |
| Employed | 44 (165) |
| Unemployed | 56 (207) |
| Monthly income (Saudi riyal) | |
| ≤5000 | 56 (211) |
| 5001–10,000 | 27 (99) |
| ≥10,000 | 17 (62) |
| Blood pressure status | |
| Controlled | 69 (257) |
| Uncontrolled | 31 (115) |
| Presence of comorbidities (≥2) | |
| Yes | 58 (215) |
| No | 42 (157) |
| Number of medications taken | |
| >6 | 72 (268) |
| (4–6) | 24 (91) |
| ≤3 | 3 (13) |
| Time since diagnosis (years) | |
| >5 | 55 (205) |
| 2–5 | 39 (146) |
| ≤1 | 6 (21) |
| Family history of hypertension | |
| Yes | 80 (299) |
| No | 20 (73) |
Sociodemographic and health status characteristics
3.2. Response to Each Questionnaire Item
The overall mean adherence based on our adapted scale was 5.3 ± 2.3. Although only 23% (n = 87) of the participants were classified as having high adherence, 181 (49%) had low adherence and 104 (28%) had medium adherence. The responses for each item are summarized in Table 2. Based on our dichotomization of adherence level, the rate of nonadherence was 49% (n = 181) while the rate of adherence was 51% (n = 191).
| Questions | Answer | Total % (n) |
|---|---|---|
| 1. Forgetfulness of taking pills | Yes | 42 (156) |
| No | 58 (216) | |
| 2. Missing of taking pills in the last 14 days | Yes | 40 (147) |
| No | 60 (225) | |
| 3. Stop medications when feeling worse | Yes | 29 (107) |
| No | 71 (265) | |
| 4. Forget to take medications when going out | Yes | 44 (165) |
| No | 56 (207) | |
| 5. Taking the pills as prescribed in last 24 h | Yes | 88 (326) |
| No | 12 (47) | |
| 6. Taking less or stopping medications when feeling better | Yes | 31 (116) |
| No | 69 (256) | |
| 7. Taking pills every day is a real burden | Yes | 36 (133) |
| No | 64 (239) | |
| 8. Frequency of having hard time to recall taking all pills | All the time | 1 (4) |
| Usually | 5 (17) | |
| Sometimes | 20 (75) | |
| Once in a while | 15 (57) | |
| Never/rarely | 59 (219) | |
| Adherence scale | Low adherence | 49 (181) |
| Medium adherence | 28 (104) | |
| High adherence | 23 (87) | |
| Dichotomous scale | Adherent | 51 (191) |
| Nonadherent | 49 (181) |
Responses to each question in the scale
As shown in Figure 1, when asked about adherence to the dose from yesterday, a low number of participants (12%, n = 47) responded with a negative answer; nevertheless, 60% (n = 225) of participants responded with a positive answer when asked to report missing medication in the past 2 weeks.
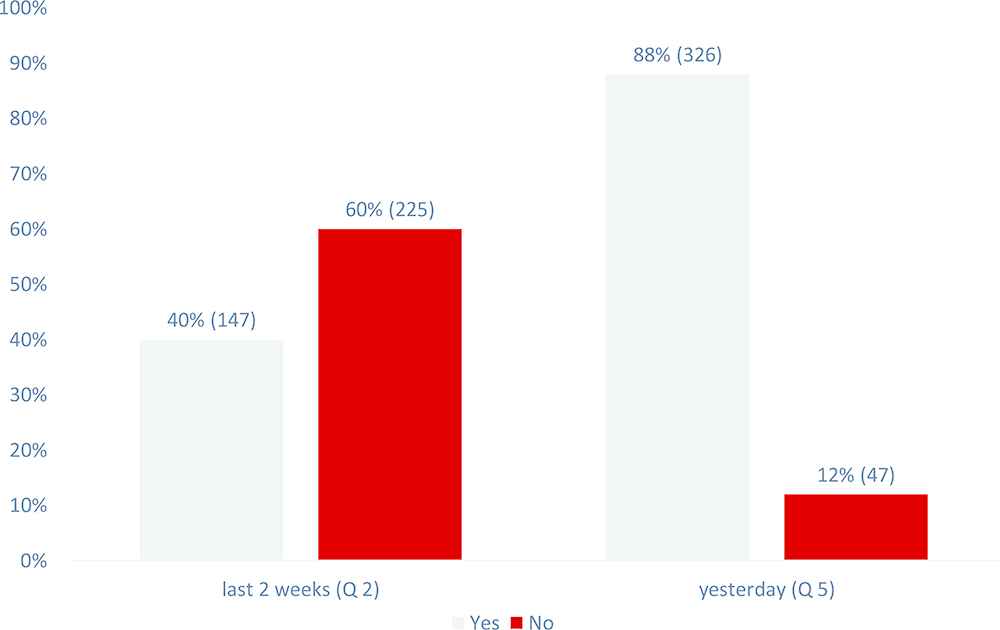
Comparison between reported missing medications doses in the past 2 weeks versus forgetting yesterday’s dose (Q2 vs. Q5) in our scale. Q, question.
The percentage of participants who cut back or stopped their medications when feeling better was similar to the percentage of participants who stopped their medications when feeling worse (31% vs. 29%) Figure 2.
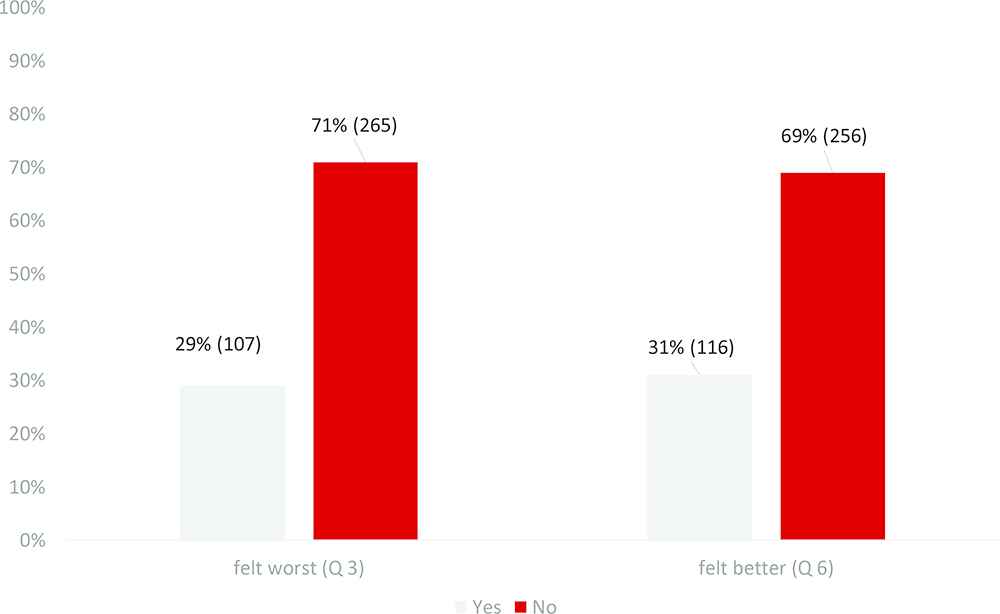
Comparison between stopping medications when feeling worse (Q3) and better (Q6) in our scale. Q, question.
3.3. Crude Analysis of Effect of Predictors of Nonadherence
Crude analysis for predictors of nonadherence is shown in Table 3. There were no significant differences between the adherent and nonadherent groups in the following variables: gender, age, nationality, level of education, marital status, residency, job status, monthly income, long time from diagnosis, and family history of hypertension. However, among participants with uncontrolled blood pressure, the percentage of nonadherent participants was significantly higher than the percentage of adherent participants (63% vs. 37%, p < 0.001). Among patients with single comorbidity, the percentage of adherent participants was significantly higher than the percentage of nonadherent participants. Among participants taking more than six medications, the percentage of nonadherent participants was significantly higher than the percentage of adherent participants (85% vs. 15%, p = 0.016).
| Parameters | Adherent status | OR | 95% CI | p | ||
|---|---|---|---|---|---|---|
| Adherenta % (n) | Nonadherentb % (n) | Lower | Upper | |||
| Gender | ||||||
| Male | 48 (110) | 52 (121) | 1 | |||
| Female | 57 (81) | 42 (60) | 1.485 | 0.974 | 2.265 | 0.066 |
| Age group (years) | ||||||
| <50 | 48 (68) | 52 (73) | 1 | |||
| ≥50 | 53 (123) | 47 (108) | 1.223 | 0.804 | 1.86 | 0.348 |
| Nationality | ||||||
| Saudi | 51 (187) | 49 (177) | 1 | |||
| Non-Saudi | 50 (4) | 50 (4) | 0.947 | 0.233 | 3.842 | 0.939 |
| Level of education | ||||||
| Primary school or lower | 47 (89) | 52 (93) | 1 | |||
| Secondary school | 24 (46) | 23 (42) | 1.284 | 0.754 | 2.187 | 0.358 |
| Diploma | 7 (13) | 6 (11) | 1.122 | 0.609 | 2.068 | 0.713 |
| Bachelor’s degree of above | 22 (43) | 19 (35) | 1.04 | 0.415 | 2.605 | 0.934 |
| Marital status | ||||||
| Single | 39 (9) | 61 (14) | 1 | |||
| Married | 51 (159) | 49 (150) | 3.111 | 0.245 | 39.54 | 0.382 |
| Widowed | 57 (21) | 43 (16) | 1.887 | 0.169 | 21.024 | 0.606 |
| Separated | 67 (2) | 33 (1) | 1.524 | 0.127 | 18.324 | 0.74 |
| Residency | ||||||
| Rural | 53 (62) | 47 (129) | 1 | |||
| Urban | 51 (56) | 49 (125) | 0.932 | 0.602 | 1.443 | 0.753 |
| Job status | ||||||
| Employed | 51 (84) | 49 (81) | 1 | |||
| Unemployed | 52 (107) | 48 (100) | 1.032 | 0.685 | 1.554 | 0.881 |
| Monthly income (Saudi riyal) | ||||||
| ≤5000 | 48 (101) | 52 (110) | 1 | |||
| 5001–10,000 | 58 (57) | 42 (42) | 1.239 | 0.703 | 2.186 | 0.458 |
| ≥10,000 | 53 (33) | 47 (29) | 0.838 | 0.443 | 1.588 | 0.589 |
| Blood pressure status | ||||||
| Controlled | 58 (149) | 42 (108) | 1 | |||
| Uncontrolled | 37 (42) | 63 (73) | 0.417 | 0.265 | 0.656 | <0.001* |
| Presence of ≥2 comorbidities | ||||||
| Yes | 47 (101) | 53 (114) | 1 | |||
| No | 57 (90) | 43 (67) | 1.516 | 1.002 | 2.295 | 0.049* |
| No. of medications taken | ||||||
| ≤3 | 54 (145) | 46 (123) | 1 | |||
| 4–6 | 48 (44) | 52 (47) | 1.259 | 0.782 | 2.027 | 0.343 |
| >6 | 15 (2) | 85 (11) | 6.484 | 1.41 | 29.814 | 0.016* |
| Time of since diagnosis (years) | ||||||
| >5 | 50 (103) | 50 (102) | 1 | |||
| 2–5 | 53 (77) | 47 (69) | 0.986 | 0.394 | 2.463 | 0.975 |
| ≤ 1 | 52 (11) | 48 (10) | 1.089 | 0.443 | 2.677 | 0.852 |
| Family history of hypertension | ||||||
| Yes | 51 (153) | 49 (164) | 1 | |||
| No | 52 (38) | 48 (73) | 1.036 | 0.621 | 1.729 | 0.892 |
Adherent, high and medium adherence;
Nonadherent, low adherence;
Statistically significant.
CI, confidence interval; OR, odds ratio.
Crude analysis of effect of predictors on nonadherence
3.4. Multiple Logistic Regression Analysis for Predictors of Adherence
A multiple logistic regression model was conducted, adjusting for the following covariates: gender, age, blood pressure status, presence of comorbidities, and the number of current medications Table 4.
| Parameters | χ2 | OR | 95% CI | p | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Male gender | 0.778 | 0.817 | 0.522 | 1.279 | 0.378 |
| Age < 50 years | 1.868 | 0.722 | 0.453 | 1.152 | 0.172 |
| Control blood pressure | 12.079 | 2.273 | 1.431 | 3.612 | 0.001* |
| Presence of ≥2 comorbidities | 2.540 | 0.697 | 0.447 | 1.086 | 0.111 |
| ≤3 medications taken | 1.133 | 1.318 | 0.792 | 2.193 | 0.287 |
Statistically significant. CI, confidence interval; OR, odds ratio.
Results of multivariate logistic regression analysis of identifying effective antihypertensive medications
The odds of being adherent were significantly higher among participants with controlled blood pressure than participants with uncontrolled blood pressure. Participants with controlled blood pressure had a twofold increase in the odds of having appropriate adherence level. When compared to probability of being nonadherent, the odds of being adherent were lower among participants with the following characteristics; male gender, aged <50 years, and having ≥2 comorbidities, but the differences were not significant. Participants who had two or more comorbidities had a 30% decrease in the odds of being adherent. Participants who were male had ~20% lower odds of being adherent. Participants who were aged <50 years had 28% lower odds of being adherent. Furthermore, the odds of being adherent were higher among participants having three or less medications than among nonadherent participants, but the difference was not significant. From the logistic regression model, for every increase in the number of current medications (≤3 categories), there was 1.3 greater odds of being adherent.
3.5. Crude and Multiple Logistic Regression Analysis of the Effect of Predictors on Blood Pressure Control
We further analyzed our data considering the status of blood pressure control as an outcome-dependent variable, and a summary of crude analysis for the predictors of blood pressure control are shown in Table 5. Among participants residing in rural areas, the percentage of participants with controlled blood pressure was significantly higher than the percentage of participants with noncontrolled blood pressure (78% vs. 22%, p = 0.019). The proportion of participants with controlled blood pressure was significantly higher in those having the following characteristics: residing in urban area (65% vs. 35%); female gender (77% vs. 23%); earning high income > 5000 Saudi riyal (81% vs. 19%); and taking six or less medications, high level of adherence (70% vs. 30%).
| Parameters | Blood pressure status | OR | 95% CI | p | ||
|---|---|---|---|---|---|---|
| Controlled % (n) | Uncontrolled % (n) | Lower | Upper | |||
| Gender | ||||||
| Male | 64 (149) | 36 (82) | 1 | |||
| Female | 77 (108) | 23 (33) | 1.801 | 1.121 | 2.893 | 0.015* |
| Age group (years) | ||||||
| <50 | 71 (100) | 29 (41) | 1 | |||
| ≥50 | 68 (157) | 32 (74) | 0.87 | 0.551 | 1.373 | 0.55 |
| Nationality | ||||||
| Saudi | 69 (251) | 31 (113) | 1 | |||
| Non-Saudi | 75 (6) | 25 (2) | 1.351 | 0.268 | 6.795 | 0.715 |
| Level of education | ||||||
| Primary school or lower | 67 (122) | 33 (60) | 1 | |||
| Secondary school | 64 (57) | 35 (31) | 1.6 | 0.89 | 3.019 | 0.113 |
| Diploma | 75 (18) | 25 (6) | 1.813 | 0.914 | 3.595 | 0.089 |
| Bachelor’s degree of above | 77 (60) | 23 (18) | 1.111 | 0.384 | 3.218 | 0.846 |
| Residency | ||||||
| Rural | 78 (92) | 22 (26) | 1 | |||
| Urban | 65 (165) | 35 (89) | 0.525 | 0.316 | 0.869 | 0.012* |
| Job status | ||||||
| Employed | 70 (116) | 30 (49) | 1 | |||
| Unemployed | 68 (141) | 32 (66) | 0.902 | 0.579 | 1.407 | 0.65 |
| Monthly income (Saudi riyal) | ||||||
| ≤5000 | 68 (144) | 32 (67) | 1 | |||
| 5001–10,000 | 64 (63) | 36 (36) | 1.939 | 0.969 | 3.879 | 0.061 |
| ≥10,000 | 81 (50) | 19 (12) | 2.381 | 1.123 | 5.048 | 0.024* |
| Level of adherence | ||||||
| Low | 60 (108) | 40 (73) | 1 | |||
| Medium | 81 (84) | 19 (20) | 1.422 | 0.715 | 2.825 | 0.315 |
| High | 75 (65) | 25 (22) | 2.839 | 1.604 | 5.025 | <0.001* |
| Presence of ≥2 comorbidities | ||||||
| Yes | 67 (144) | 33 (71) | 1 | |||
| No | 72 (123) | 28 (44) | 1.266 | 0.808 | 1.985 | 0.303 |
| No. of medications taken | ||||||
| ≤3 | 73 (195) | 27 (73) | 1 | |||
| 4–6 | 61 (56) | 39 (35) | 1.67 | 1.012 | 2.754 | 0.045* |
| >6 | 46 (6) | 54 (7) | 3.116 | 1.014 | 9.581 | 0.047* |
| Time of since diagnosis (years) | ||||||
| >5 | 67 (138) | 33 (67) | 1 | |||
| 2–5 | 71 (104) | 29 (104) | 1.01 | 0.367 | 2.778 | 0.985 |
| ≤1 | 71 (15) | 29 (6) | 1.214 | 0.451 | 3.269 | 0.702 |
| Family history of hypertension | ||||||
| Yes | 67 (201) | 33 (98) | 1 | |||
| No | 77 (56) | 23 (17) | 1.606 | 0.887 | 2.909 | 0.118 |
Statistically significant; CI, confidence interval; OR, odds ratio.
Binary logistic regression analysis identifying effective blood pressure control
A multiple logistic regression model was conducted, adjusting for the following covariates: gender, residency, monthly income, number of medications taken, and adherence Table 6. The odds of having controlled blood pressure was significantly higher among adherent than nonadherent participants. Adherent participants had a twofold increase in the odds of having controlled blood pressure. Participants residing in a rural area were 1.8 times more likely to have controlled blood pressure than participants living in an urban area. From the logistic regression model, for every increase in the number of current medications, there was 1.6 greater odds of having controlled blood pressure. The odds of having controlled blood pressure were lower among participants with the following characteristics: male gender and low monthly income (≤5000 Saudi riyal), but they differences were not significant. Participants who were male had ~40% lower odds of having controlled blood pressure. Among participants who had a low monthly income, there was a 15% reduction in the odds of having controlled blood pressure.
| Parameters | χ2 | OR | 95% CI | p | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Male gender | 3.433 | 0.614 | 0.366 | 1.029 | 0.064 |
| Rural residency | 5.466 | 1.863 | 1.106 | 3.14 | 0.019* |
| Monthly income ≤ 5000 SAR | 0.393 | 0.855 | 0.525 | 1.394 | 0.531 |
| ≤3 medications taken | 3.503 | 1.606 | 0.978 | 2.638 | 0.061 |
| Adherent | 11.246 | 2.221 | 1.393 | 3.542 | 0.001* |
Statistically significant. CI, confidence interval; OR, odds ratio; SAR, Saudi riyal.
Results of multivariate logistic regression analysis of identifying effective blood pressure control
4. DISCUSSION
Noncompliance to medications is considered a major risk factor for disease progression and treatment failure, which subsequently increase hospitalization and mortality [5–7]. The aim of this study was to assess the prevalence of nonadherence to hypertensive medications among adults attending PHCs in Al-Hasa Region, Saudi Arabia. One of the main findings in this study was that the prevalence of nonadherence was 49%, which is consistent with the prevalence rate reported nationally and internationally (54% and 54.2%, respectively) [17–19].
In this study, the level of adherence to antihypertensive medications was positively associated with age, although this association was no longer found after adjusting for other confounding predictors. Similar crude analysis has been reported in other national studies [17,20,21]. For instance, Al-Sowielem and Elzubier [20] in a cross-sectional study conducted in four PHCs in Alkhobar area have reported a lower rate of adherence in those aged < 55 years than in older patients (26.2% vs. 48.5%). Similar findings have also been reported in international studies [17,22–24]. The higher medication adherence among this age group can be explained by the presence of a caregiver who would help them in taking their medications, compared to the younger patients who usually have work-related commitments and other priorities.
Our study has also shown a positive association between the number of medications taken and the adherence score. Similar to the age predictor findings, this was not significant after adjustment. The association of polypharmacy with adherence outcome has been demonstrated [25]. An additional relevant finding was related to the positive association of number of comorbidities with lower adherence level compared to a patient with single comorbidity. In contrast to our findings, there was no significant association between number of medications taken and adherence level in other national studies [9,21]. In a third international study conducted in northwest Ethiopia, Mekonnen et al. [26] showed that participants who had no comorbidity were four times more likely to adhere to antihypertensive medications than their counterparts.
Also, we clearly demonstrated a positive association between high adherence level and control of blood pressure, which conforms with the projected and reasonable clinical outcomes. The same has been reported in previous studies [9,17,18]. Adherence to antihypertensive medications is the cornerstone for achieving hypertension control. Such adherence has a marked effect on the progress and outcomes of hypertension care. Therefore, in order to change patients’ behavior, it is crucial to recognize adherence pattern, and subsequently identify the reasons linked to that observed pattern [27,28].
Although some of the important variables such as age, nationality, and level of education were not statistically associated with nonadherence, our findings should not be generalized to all hypertension populations. This disassociation can be attributed to multiracial background, multiethnicity, and the different lifestyle of the Al-Hasa population [29]. It could be also attributed to differences in prescribing behavior among practitioners.
Our study has several potential implementations and recommendations. The low adherence rate should raise a concern about the immediate need for a variety of multilevel interventions related to decision-making policies, institutions protocols, and individual clinicians’ practices. Those interventions can come in the form of offering training programs for the providers to simplify the dosing regimen, executing interventional educational programs for patients, encouraging the use of adherence toolboxes and electronic apps for self-recording, and offering reminder tags [6].
Such interventions have the potential to increase patients’ and providers’ awareness of the magnitude of the adherence problem and its consequences. Also, planning multichannel awareness campaigns for the local community is a key to spread the knowledge about nonadherence consequences. Also, designing a continuous evaluation program to continually determine the cumulative level of medication compliance is paramount for providing an accurate picture and delivering better care. Furthermore, our findings suggested that specific subgroups of patients (patients with comorbidities, those with a high number of medications, those living in rural areas, low-income groups, and patients younger than 65 years) will probably need more and special attention. Some interventions although not supported by solid evidence have been suggested and might partially help to improve adherence to antihypertensive medications.
Our study had several limitations. The cross-sectional design is subject to unavoidable recall bias [30,31]. However, we tried to minimize this type of bias using a validated scale such as AOTBA and MMAS-8. Many confounding factors (health system and provider related [32]) that were not feasible to collect in our study could have affected the adherence level and outcome. Although we tried to reduce the proportion of error by using random sampling, our inclusion criteria may have introduced selection bias and affected our findings [33]. In addition, our exclusion criteria may impact the external validity and the generalizability of this study. Although we exceeded the calculated sample size for our study, our sample size was still low (n = 372) to generalize our findings to the Al-Hasa population.
5. CONCLUSION
The high level of medication nonadherence (~50%) associated with uncontrolled blood pressure in Al-Hasa Region found in this study should alert decision-makers, institutional administrators, and clinicians to take necessary actions to improve the current situation in healthcare practice. To our knowledge, this is the first study to investigate the prevalence of nonadherence to prescribed antihypertensive medications in Al-Hasa Region.
CONFLICTS OF INTEREST
All authors declare no conflicts of interest.
REFERENCES
Cite this article
TY - JOUR AU - Abdulrahim M. Alkhamis AU - Abdulkhaliq J. Alsalman AU - Mohammed Al Khamis AU - Abdullah Alkhamis AU - Nawaf M. Alotaibi PY - 2019 DA - 2019/06/30 TI - Prevalence of Nonadherence to Antihypertensive Medications among Adults Attending Primary Healthcare Clinics in Al-Hasa Region: A Cross-Sectional Study JO - Dr. Sulaiman Al Habib Medical Journal SP - 36 EP - 43 VL - 1 IS - 1-2 SN - 2590-3349 UR - https://doi.org/10.2991/dsahmj.k.190516.001 DO - 10.2991/dsahmj.k.190516.001 ID - Alkhamis2019 ER -
