Cardiovascular aging: Insights from local and regional measures of aortic stiffness using magnetic resonance imaging
- DOI
- 10.1016/j.artres.2014.01.005How to use a DOI?
- Keywords
- Cardiovascular aging; Magnetic resonance imaging; Aortic stiffness; Distensibility; Pulse wave velocity
- Abstract
Aortic stiffness is now established as an independent marker of cardiovascular aging and cardiovascular risk. However, the specific role of the proximal aorta, specifically the ascending aorta, remains understudied. Magnetic resonance imaging (MRI), a non-invasive technique has recently been proposed to measure new local and regional imaging biomarkers of stiffness in the thoracic aorta. We will here review recent data on aortic stiffness assessed by MRI. We will discuss the methodological advantages and challenges of MRI, combined with applanation tonometry, to evaluate local aortic distensibility and pulse wave velocity (PWV) and summarize available results concerning the age related distribution of such parameters.
Aortic distensibility has been shown to be an early subclinical marker of vascular target organ damage in the general population and expected ranges for ascending aortic distensibility and aortic arch pulse wave velocity assessed in MRI have been described. Changes in aortic distensibility and arch PWV have been related to age-related geometric changes, specifically lengthening, enlargement and unfolding of the thoracic aorta. Increased proximal aortic stiffness measured by MRI has also been related to decreased systolic and diastolic function and concentric remodeling of the left ventricule in healthy individuals.
- Copyright
- © 2014 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Background
The increasing burden of cardiovascular disease in aging world populations associated with increased systolic and pulse pressures has been related to two main factors: arterial stiffness and wave reflections. Aortic stiffness has emerged clinically as an important integrated marker of large arterial vessel damage over a lifetime, whereas measures such as blood pressure or biological markers are indirect and instantaneous measures of aortic stiffness furthermore highly modifiable by drugs.1 Furthermore, age-related changes in blood pressure which are only indirect measures of aortic stiffness appear to be significant only later in life.
Along the arterial tree, the proximal aorta is responsible for most of the buffering and immediate conduit function of the pulsatile systolic flow from the heart to the peripheral vasculature and end organs. Alterations of these two components of aortic function lead to inefficiency of the circulatory system and potential vascular–ventricular uncoupling eventually deleterious to the heart through increased workload.
One of the great challenges in this field of research is to untangle the relative effects of age and disease including cardiovascular risk factors when both the age-driven vascular alterations and atheroslcerosis-driven disease continuum share similar mechanisms such as hypertrophy, remodeling, ischemia, fibrosis and generate the same complications such as heart failure and sudden death. However, this overlap between age-related alterations and disease may differ along the arterial tree which is highly heterogenous regarding its viscoelastic properties. Indeed, the ascending aorta differs from the descending aorta both embryologically and in its natural history as it is less prone to atheroma, thrombus and calcification but more to dilatation secondary to fragmentation and alteration of its important elastic component.2 Consequently, local and direct indices of aortic stiffness may have increased relevance as they may be more specifically related to aging vs. a disease process and also because they may be more sensitive to early infra clinical alterations than more global or surrogate markers of arterial stiffness.
However, the challenge is to determine the robustness of such markers, their distribution and correlates in the general population and in patients with cardiovascular disease and finally their predictive value for adverse events beyond the available and established indices of aortic stiffness.
The non-invasive assessment of aortic stiffness schematically relies on the assessment of either pulse wave velocity or local cross sectional changes in vessel area driven by local pulse pressure (distensibility). The reference method to assess global aortic stiffness is the measurement of carotid to femoral pulse wave velocity by applanation tonometry (cf-PWV). This technique benefits from a large experience, wide cohort applications and reported distribution in the general population and patients, particularly in hypertension. Furthermore, cf-PWV is a recognized independent risk factor for mortality and hard cardiovascular events in the general population. More recently, magnetic resonance imaging (MRI) has been proposed to provide a comprehensive non-invasive study of the aorta. One of the strengths of this method is indeed to provide simultaneously a thorough three-dimensional exploration of aortic anatomy as well as local wall dynamics and flow. Assessment of cardiac structure and function or peripheral arteries and organs can also be performed in the same setting. We will here discuss the methodological advantages and challenges of MRI, combined with applanation tonometry, to evaluate aortic biomechanics and geometry and summarize available data concerning the age-related distribution of such parameters compared with established measures of aortic stiffness.
Assessing structure and function of the thoracic aorta using MRI: methods and results in cardiovascular aging
MRI, a reference technique to evaluate cardiac structure and function also uniquely provides non-invasive depiction of aortic anatomy, wall motion and flow in any given anatomical localization or spatial direction. Electrocardiogram gating and segmented acquisition techniques over several heartbeats are used to generate anatomic images corresponding to different phases of the cardiac cycle. The resulting cine acquisitions can be used to track aortic wall motion with high spatial (0.7 mm) and temporal resolution (10 ms–30 ms) depending on the heart rate and breath holding ability. Moreover, the intrinsic sensitivity of magnetic resonance to motion and flow can be used to produce velocity and flow maps using phase-contrast acquisition sequences (Fig. 1).
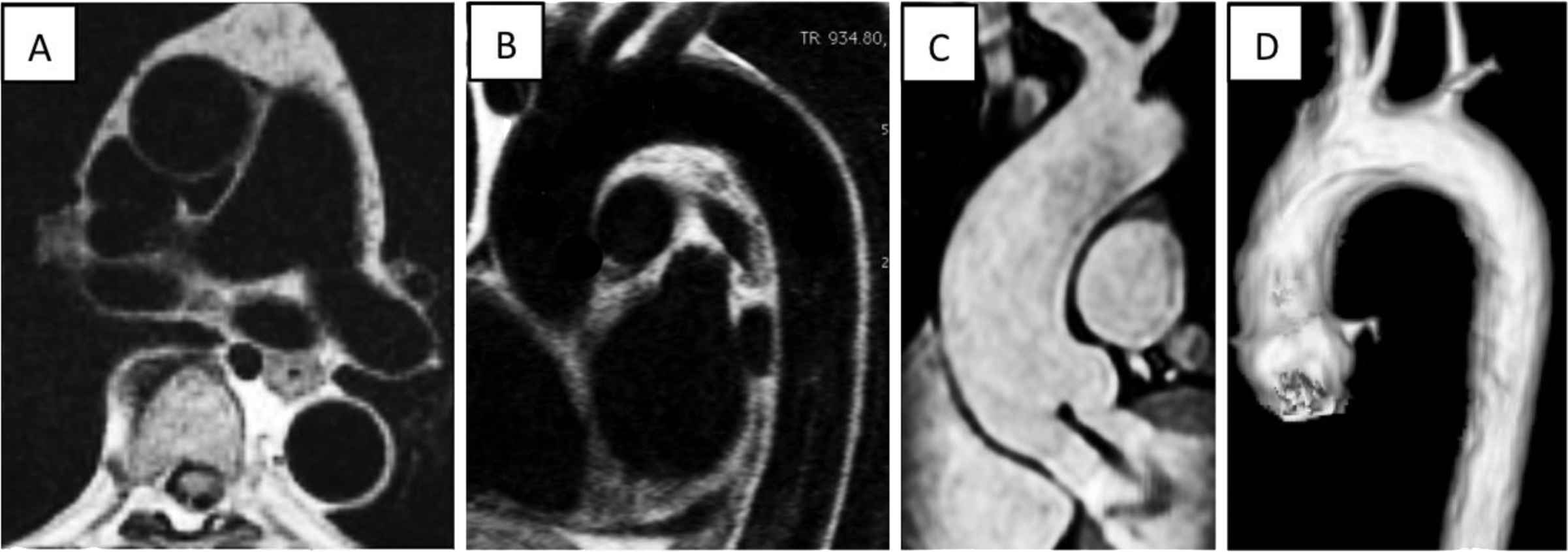
Anatomy and geometry of the thoracic aorta in MRI. Cross sectional (panel A) and longitudinal sagittal oblique (panel B) views of the aorta in diastole in ECG-gated black-blood spin echo sequences allowing good depiction of the vessel wall. These sequences can be acquired prior to and after contrast injection. Reformat of a non-contrast 3-SSFP sequence (panel C) showing the ascending aorta and aortic root with central aortic regurgitation (linear signal void). Volume rendering of contrast enhanced 3D magnetic resonance angiography showing a normal “Roman” shaped aortic arch.
Aortic structure and geometry
Aortic wall thickness
MRI allows to visualize the aortic wall in any plane orientation (Fig. 1). Most studies are based on black-blood spin echo T1-weighted acquisitions which generate a sharp contrast between the signal from the wall and the blood. An age-related increase in average wall thickness of the descending aorta was reported in 1053 general population individuals aged 45–85 years (average 2.35 ± 0.5 mm) but was not found for the ascending aorta (average 2.8 mm).3,4 In this study SBP and hypertension were also independent correlates of increased wall thickness. Good reproducibility for this measurement has been reported.5,6 However, the spatial resolution of most acquisitions (0.7–1 mm) being about half of the expected thickness for the aortic wall (1.5–2.5 mm) we believe that partial volume remains a major drawback that will require higher spatial resolution and refined automated quantification methods to be accurate. No large MRI studies are available on the wall thickness of young and healthy individuals.
Static cross sectional aortic dimensions
Numerous MRI methods allow to measure aortic size. We will not review them here extensively. One of the strengths of MRI is to provide a 2D or 3D approach allowing to accurately measure aortic area or volume instead of relying on a 1D measure of diameter prone to higher measurement bias. Cross-sectional area of the aorta can also be used to calculate a mean diameter value. Recently, the distribution of the mean diameter of the ascending aorta was reported according to age and gender in 3573 general population individuals aged 45–85 years according to age and gender.3 In this study the median value of AA luminal diameter increased by 1.1 mm per each decade for both men and women. Overall, age was the strongest associate of increased ascending aortic diameter along with gender and body surface area. The subgroup study of the 1612 « healthy » individuals without risk factors showed a mean and 95th percentile (upper limit) of AA diameter of 31 mm (38 mm) vs. 32 mm (39 mm) in the global cohort. The inter-reader intraclass correlation for the measurement of mean ascending aortic area on modulus images of MRI phase contrast acquisitions on 100 individuals was 0.98 (95%CI: 0.98–0.99) with a mean difference of 0.14 mm (limits of agreement −1.1–1.4 mm). Interestingly, in the Dallas Heart study, increased abdominal aortic wall thickness was associated with a high lifetime predicted risk of cardiovascular disease in individuals from 30 to 50 years with a low short-term risk.7
The constitutional decrease in aortic diameter along the aorta or aortic tapering has been well documented by MRI.8,9 However, the age-related widening of the aortic lumen and rate of diameter increase for each respective location is not homogeneous along the aorta. Indeed, the progression of aortic diameters markedly predominates in the ascending compared to descending aorta. Secondly, the thoracic aorta elongates with increasing age.9,10 We have recently shown that the age-related elongation of the aorta is also much more marked in the ascending aorta and associated with widening of the arch and unfolding of the aorta9 as illustrated on Fig. 2. Reasons for this inhomogeneity in regional structural alterations likely include the relative content in elastin fibers, higher in the ascending aorta and decreasing along the aorta leading to the more muscular and resistive peripheral arteries. This constitutional difference between the ascending aorta and more peripheral locations is well known but not often functionally explored. We have shown Aortic arch unfolding due to widening and elongation with increased tortuosity to be independently related to increased peripheral and central blood pressure components as well as to cardiac hypertrophic remodeling i.e. increased left ventricular mass and mass to volume ratio in healthy individuals.
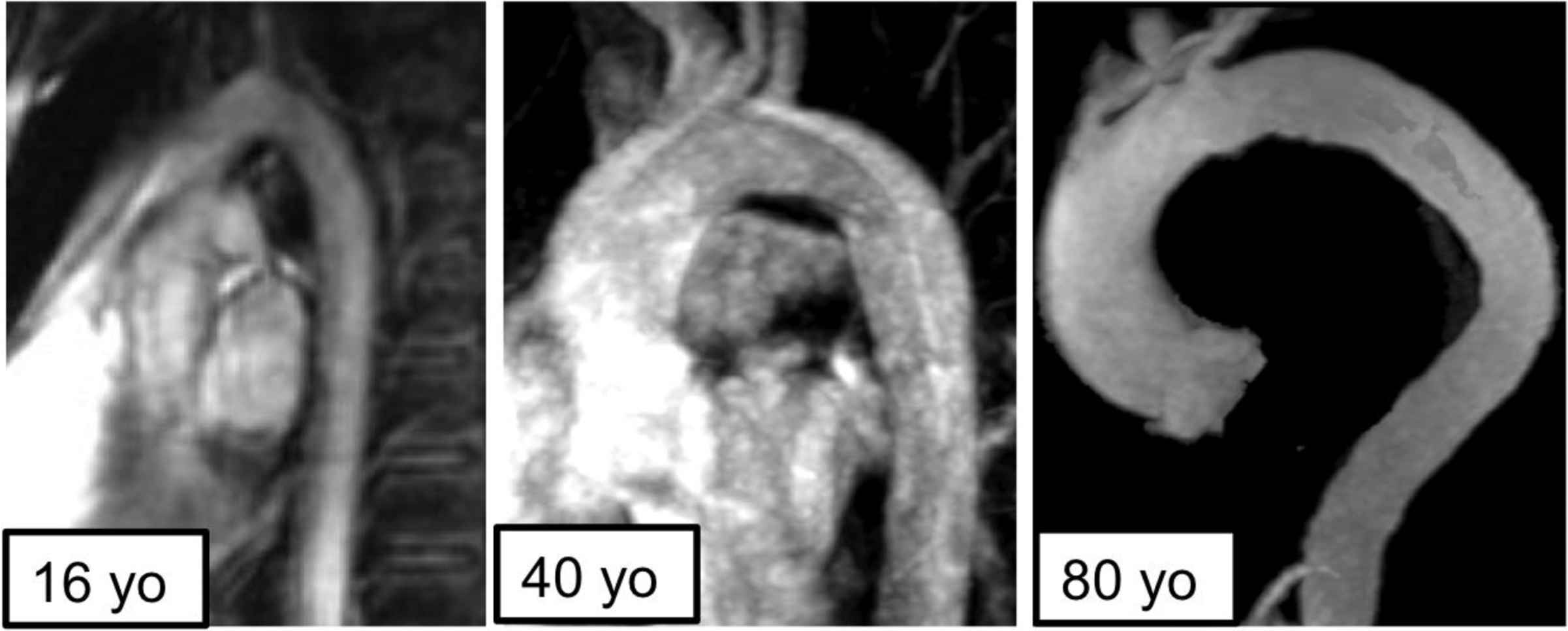
Age-related unfolding of the aortic arch. Comparison of aortic arch morphologies between 16, 40 and 80 year old asymptomatic individuals demonstrating the transversal and longitudinal enlargement of the aortic lumen and lengthening of the arch with progressive unfolding and increased tortuosity.
Aortic wall dynamics: strain and distensibility (Fig. 3)
One of the strengths of MRI is to allow the complete dynamic exploration of the thoracic aorta in any given orientation. Most static cross sectional aortic area measures are done in diastole and therefore only represent the « post-recoil » state of the aorta. We believe that dynamic acquisitions providing circumferential aortic lumen area changes across the cardiac cycle may have greater value as they quantify the buffer component of aortic function dampening pulsatile flow from the heart. Circumferential aortic strain may be defined as the relative change in aortic area during the cardiac cycle, expressed in percent (AS = ΔA/A min). Where the local central pressure curve available in the ascending aorta during the strain acquisition the full compliance curve of the aorta could be generated. However, available data are based on a simplified linear estimate of the compliance curve using the maximum and minimum aortic lumen area and corresponding pressures. Aortic distensibility can be measured as AD = AS/PP, PP being the pulse pressure driving the aortic area changes.
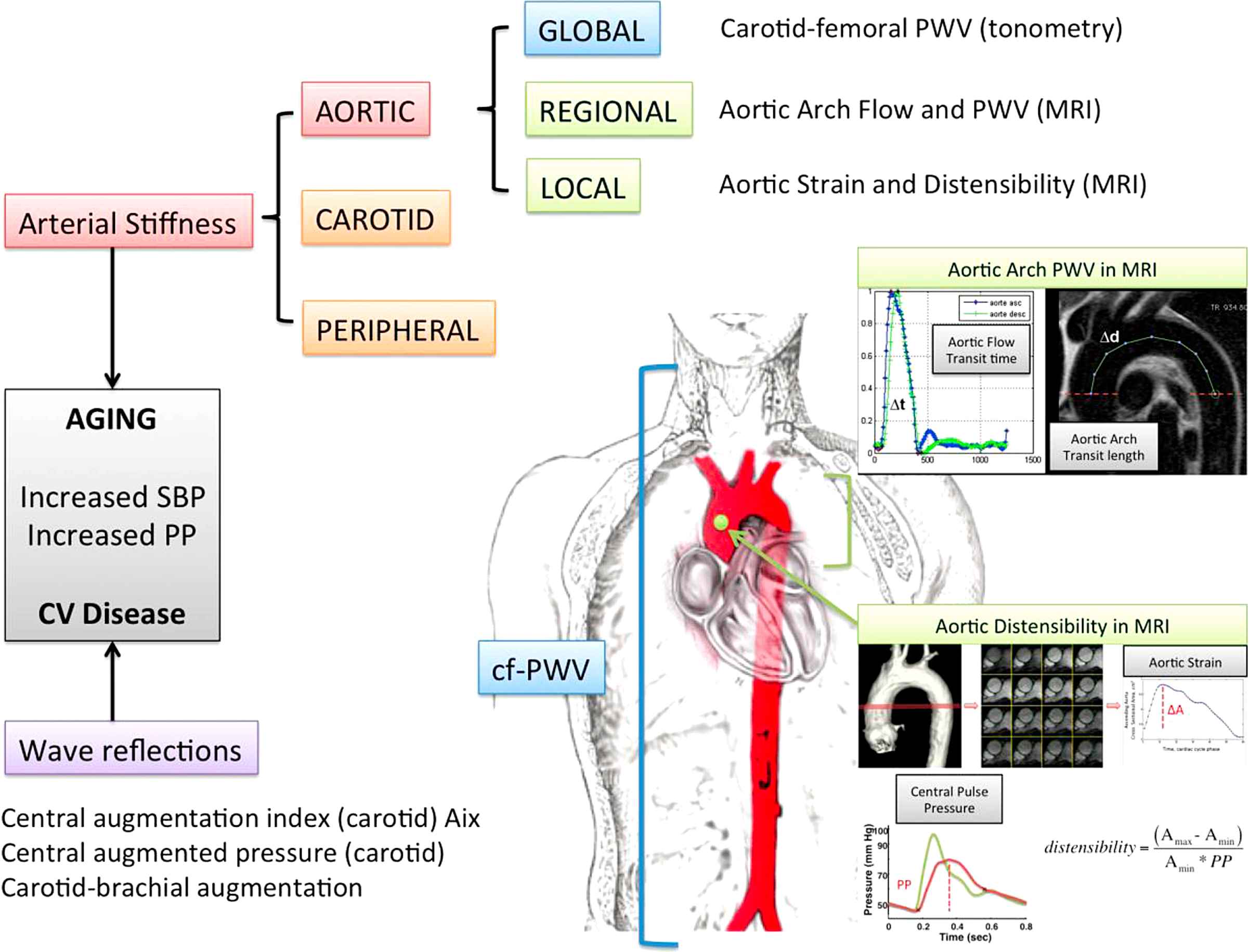
Assessment of local and regional aortic stiffness using MRI.
Which MRI method should be used to measure aortic strain?
Accurate measurement of aortic strain requires high spatial, temporal and contrast resolution. These features are achieved by current SSFP (steady state free precession) cine acquisitions which can achieve 0.7 mm of spatial resolution, less than 10 ms of temporal resolution and high contrast between wall and blood with constant signal. Such images allow to perform robust automated segmentation of the aortic wall.11,12 Herment et al. validated an automated (2D + t) snake method to measure circumferential area to time curves in the aorta from either SSFP or phase contrast images with comparable results and good accuracy when compared to a compliant phantom.13 However, interobserver agreement was better with SSFP compared to phase-contrast images. The dependency of the segmentation methods on signal variations at the wall/blood interface favors the use of flow compensated SSFP images rather than gradient echo or phase-contrast modulus images where near wall signal is greatly influenced by local flow with lower near wall velocities generating lower signal. This phenomenon may be aggravated at higher magnet field strengths. Spatial resolution in phase contrast is also typically lower than in SSFP imaging. Consequently, we recommend using high spatial and temporal resolution SSFP cine images to measure aortic strain.
Which pressures should be used to calculate distensibility?
Most aortic distensibility studies rely on brachial cuff pressure measured during the MRI exam to normalize aortic strain. However, because of the amplification phenomenon in the periphery this may lead to overestimate central PP and therefore underestimate distensibility, especially in younger individuals. Accordingly, we proposed to use central PP instead of brachial PP to calculate distensibility. Central pressures can be estimated either using carotid tonometry or radial tonometry and a transfer function. Ideally pressure and strain should be measured simultaneously. However, tonometry devices are not MRI compatible and measurements have to be performed immediately after the MRI exam and can be normalized by the brachial diastolic pressure measured during the strain acquisitions to approximate similar pressure conditions. As an alternative, we have shown that using central pressures estimated by the vicorder™ device during the MRI exam to calculate distensibility was feasible and resulted in higher correlations with age, cfPWV and augmentation index than using carotid or brachial pressures.14
Aortic wall dynamics and age
Aortic distensibility decreases non-linearly with advancing age. Marked age-related decrease in aortic distensibility has been shown to occur in asymptomatic general population individuals from 20 to 50 years of age with a continued decrease thereafter albeit at a slower pace.15 Ascending aortic distensibility measured using central pulse pressure is on average 74 ± 23 kPa−1 10−3 between 20 and 30 years, 18 ± 7 kPa−1 10−3 between 50 and 60 and 10 ± 6 kPa−1 10−3 after 70 years with an average decrease of 14 ± 1 kPa−1 10−3 per decade. Importantly, this change is due to a decline in aortic strain as pulse pressure is not significantly increased in this age group. In multivariate analysis including cf-PWV, carotid distensibility and Aix, ascending aortic distensibility was the strongest correlate of age making it a powerful independent and early infraclinical marker of functional aortic dysfunction. Regional heterogeneity is also found for functional indices such as distensibility as only the youngest individuals before the age of 30 have ascending aorta distensibility exceeding descending aorta distensibility.15,16 This early reversal in proximal to distal distensibility in healthy individuals could be modified by early onset cardiovascular disease. Through aortic–ventricular coupling, age-related changes in aortic distensibility is positively related to left ventricular elastance and total arterial elastance and to infraclinical changes in systolic cardiac strain and diastolic function.
Aortic flow
Regional aortic pulse wave velocity (Fig. 2)
Phase contrast MRI allows to acquire spatially registered velocities simultaneously with morphological data throughout the cardiac cycle thus allowing to obtain local flow values in any aortic location. Velocity mapping is usually performed in one through-plane direction (perpendicular to the vessel of interest) but can also be performed in-plane16 or in 3D at the cost of lower spatial and temporal resolutions and higher scanning and post-processing times.17,18 A single acquisition plane, typically placed perpendicular to the ascending aorta at the level of the mid right pulmonary artery simultaneously provides flow in the ascending and descending thoracic aorta during the same heartbeats. Pulse wave velocity is measured as the transit vascular length divided by the blood flow transit time. Flow curves should be generated using a robust automated vascular segmentation method reducing manual bias. Transit time measurement also requires caution as the temporal resolutions used in most 2D-MRI phase contrast methods (<10–20 ms) are not as resolved as in tonometry (2 ms) making the foot-to-foot measurements hazardous. Several solutions have been proposed including using a least squares minimization of the full upslope of normalized mean velocity curves corresponding to the two aortic locations of interest. The advantage of using the full upslope is to rely on several instead of one data points in the initial portion of the flow curve when flow is unidirectional and reflectionless.
Aortic PWV and distensibility, non-linearly related through the Bramwell Hill equations,19,20 are not interchangeable measures of stiffness. Indeed, when distensibility varies most in young to middle aged individuals, aortic arch PWV rises with advancing age although more rapidly after 50 years.15 Arch PWV is on average 3.5 ± 0.5 m/s between 20 and 30 years, 7.2 ± 2.3 m/s between 50 and 60 and 11.1 ± 4.6 m/s after 70 years with an average decrease of 1.6 ± 0.1 m/s per decade. Arch PWV is strongly and independently related to age as its strongest determinant. In particular it is not related to BMI and body morphology such as cf-PWV as it does not require surface approximation of aortic length.10 Arch PWV values are lower than gold standard cf-PWV values for several reasons including potential over estimation of vessel length with surface measurements and exclusion of the ascending aorta with low PWV and inclusion of peripheral arteries with higher PWV values with cf-PWV. Further potential benefits of arch PWV lie in not requiring central pressure measurement to be assessed and in being a valuable marker of proximal aortic stiffness in studies including older individuals, when distensibility may be less relevant.
Regional differences have also been described for aortic PWV, in particular by Hickson et al. showing a lower rate of age-related increase in PWV in the ascending aorta as compared to more distal locations on the aorta.8 Taken together, the aforementioned changes in aortic geometry and function probably explain most of this difference. The relatively contained age-related increase in ascending aorta PWV is probably offset in part by an increased capacitance through elongation and dilation of the proximal aorta. Subsequently, cardiovascular disease and specifically atheroma with an increased distal prevalence across the arterial tree also play an important role in explaining such regional heterogeneity. Through aortic–ventricular coupling, increased arch PWV is related to impaired diastolic function and increased left ventricular filling pressures.
Backward and forward flow components (Fig. 4)
MRI mapping of flow in 4D in the thoracic aorta can illustrate the combined effects of altered local aortic geometry, compliance and pressure on age-related flow pattern changes. In young healthy individuals, backward flow has a late onset, appearing o nly in diastole when pressure reversal due to the end of ejection and closure of the aortic valve leads to physiological local flow reversal (Fig. 4) which predominates in the inner portion of the aortic arch curvature21 (Bensalah et al. in press). Hence, even in the absence of aortic disease, the curved shape of the aorta determines in great part the flow patterns along the proximal aorta. Age-related alterations of geometry such as dilation, elongation leading to unfolding of the aorta or disease such as aneurysms, stenosis or severe atheroma will further alter blood flow patterns in the aorta potentially leading to aggravated disease in a vicious circle. In addition to these alterations of the conduit function of the aorta, functional impairment in particular the loss of the cushioning function of pulsatile flow (distension and recoil) evidenced by the loss of aortic distensibility may participate in the creation of major flow dispersion and disorganization in the proximal aorta. These processes lead to increased left ventricular afterload and result in hypertrophy to normalize wall stress and loss of cardiovascular efficiency as cardiac work will increase to maintain a constant output and vascular–ventricular coupling.
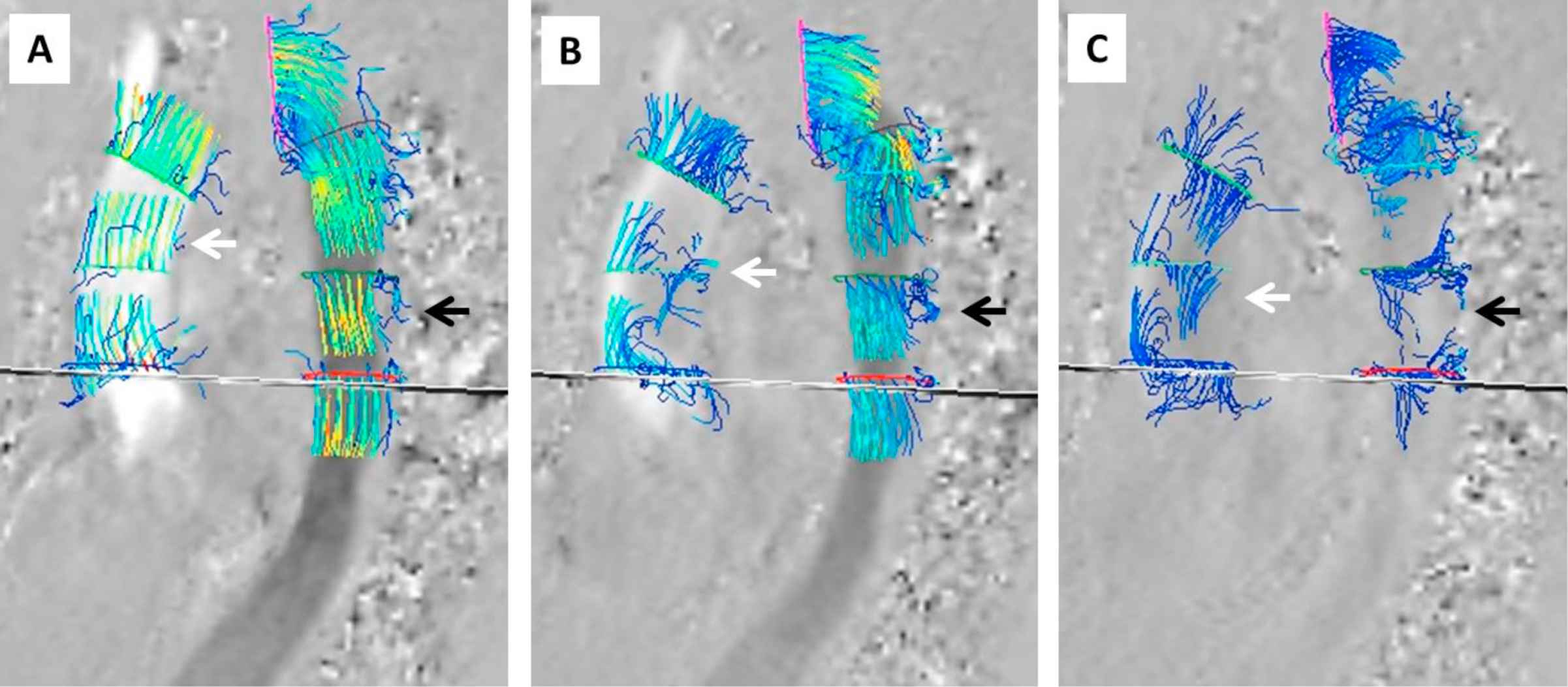
4D-MRI mapping of backward and forward flow components. Streamlines of flow in multiple locations across the thoracic aorta (ascending aorta: white arrow, descending aorta: black arrow) in a middle aged healthy individual (Gyrotools™ software). Panel A: during the early systolic phase (flow curve upslope) flow is well organized with a predominant forward component and characterized by high velocities except at the very edges where velocities are lower. Panel B: during late systole (after peak flow and pressure) we can observe flow reversal corresponding to local pressure reversal and lower velocities in the inner portion of the arch curvature preceding a similar process in the descending aorta towards the posterior wall. Panel C: during early diastole we see a marked and organized backward flow component near the inner portion of the arch curvature with relatively low velocities and disorganized flow in the descending aorta with almost nulled net instantaneous flow.
Combining pressure and flow curves
R>elating temporally normalized flow curves from MRI and pressure curves from tonometry allows to non-invasively measure other indices of aortic biomechanics. Aortic reflection indices such as the time difference between flow and pressure peaks increasing with age as been recently described. Furthermore, reflection magnitude as the ratio between backward and forward flow components can be calculated as well as the characteristic impedance, a measure of pulsatility22 (Bollache et al. Artery 2013). Further studies will determine the added value of such indices in comparison to established markers of aortic biomechanics.
Conclusions
Magnetic resonance imaging allows for a comprehensive and quantitative non-invasive and in vivo assessment of aortic structure, dynamics and flow. In combination with central pressures it provides unique and relevant markers of infra clinical aortic alterations such as strain, distensibility and PWV as well as cross sectional, longitudinal and volumetric measurements of arterial geometry. Simultaneous assessment of cardiac remodeling and function ideally provides the setting to explore vascular–ventricular coupling. Knowledge of age-related alterations remain an important prerequisite to the understanding of pathophysiological pathways in cardiovascular disease. In the intricate relationship between aging and disease recent data suggest that the proximal aorta may play an important and early role potentially determining susceptibility to hypertension and cardiovascular morbidity and mortality over a lifetime. However, numerous questions including its potential reversibility and clinical value remain to be answered.
References
Cite this article
TY - JOUR AU - Alban Redheuil PY - 2014 DA - 2014/03/14 TI - Cardiovascular aging: Insights from local and regional measures of aortic stiffness using magnetic resonance imaging JO - Artery Research SP - 66 EP - 72 VL - 8 IS - 2 SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2014.01.005 DO - 10.1016/j.artres.2014.01.005 ID - Redheuil2014 ER -
