Viscoelastic properties of the autologous bypass grafts: A comparative study among the small saphenous vein and internal thoracic artery
- DOI
- 10.1016/j.artres.2017.06.007How to use a DOI?
- Keywords
- Small saphenous vein; Internal thoracic artery; Dynamic mechanical analysis; Viscoelastic properties; Bypass grafts
- Abstract
Internal thoracic artery (ITA) and small saphenous vein (SSV) are two viable conduits for coronary artery bypass grafts. The aim of this study was to investigate the viscoelastic behavior of the small saphenous vein and internal thoracic artery under compressive and tensile loadings at body temperature. The dynamic mechanical analysis was used to measure the viscoelastic properties of the ITA and SSV at both the desired temperature and load frequency range. Storage modulus, loss modulus as well as phase angle of both the blood vessels were measured at the temperature of 37 ± 1 °C and under a sinusoidal load with the frequency range of 1–2 Hz. The mean storage and loss modulus of the SSV were both higher than that of the ITA. Furthermore, the SSV showed a higher stiffness and internal friction compared to those values under the tensile load. While ITA was stiffer under the tensile load, no considerable difference was observed among the compressive and tensile loss modulus. A more intense viscous behavior was observed under the radial direction. The results also revealed that the SSV has much higher stiffness whereas less viscous behavior compared to the ITA, especially in the radial direction. The results may have implications not only for understanding of the viscoelastic time-dependent mechanical behavior of the ITA and SSV but also for tissue engineering applications to make scaffolds according to the real time-dependent viscoelastic mechanical properties of these arteries and veins.
- Copyright
- © 2017 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Introduction
The small saphenous vein (SSV) is a superficial vein of the leg. It originates from the lateral side of the dorsal venous arch and passes behind the distal end of the fibula and up the back of the leg to penetrate deep fascia, and finally join the popliteal vein posterior to the knee.1 The SSV is in danger of becoming distended or having thrombosis.2 The internal thoracic artery (ITA) arises as a major branch of the subclavian artery in the neck. It passes posterior to the clavicle and the large veins in the region and anterior to the pleural cavity. Then, it enters to the posterior side of the thoracic cavity in the ribs and anterior to the transversus thoracis muscle and continues to descend giving off numerous branches.1 Both of these blood vessels are commonly used for treatment of coronary artery disease as bypass graft,3–6 and both are vulnerable to be occluded and lose their patency.4,7
Dynamic mechanical properties refer to the response of a material as it is subjected to a periodic force. These properties may be expressed in terms of a dynamic modulus, a dynamic loss modulus, and a mechanical damping term. Specifically, in dynamic mechanical analysis (DMA), a variable sinusoidal stress is applied, and the resultant sinusoidal strain is measured. If the material being evaluated is purely elastic, the phase difference between the stress and strain sine waves is 0°. If the material is purely viscous, the phase difference is 90°. However, most of the biological materials have viscoelastic material properties and exhibit a phase difference between those extremes. Furthermore, as DMA is a thermal analysis technique, it is well suited to analyze the viscoelastic properties of a biological material under the body temperature.8,9
Autograft for coronary artery bypass graft has been used for a long time. Johnson et al. expanded the application of the saphenous vein autograft by using it as a bypass channel for the left coronary artery.10 Furthermore, Bailey et al. used the internal thoracic artery instead of saphenous vein as a bypass graft for the coronary artery.11,12 Since then coronary artery bypass grafting has grown to become one of the most common operations in the world. Even though these bypass graft had shown a good performance, they can be occluded and fail to provide a suitable channel for the blood to flow. Therefore, understanding the mechanical behavior of these materials can provide important insights into their encounter complications. Several studies have investigated the mechanical properties of SSV and ITA. Compliance and elastic properties of the saphenous vein were investigated by Walden et al.13 Zamboni et al. measured the compliance of the both great saphenous vein and SSV.14 Furthermore, Chamiot-Clerc et al. compared the elastic mechanical properties of the internal mammary artery to the radial artery.15 Pressure–diameter, pressure–axial force, circumferential and axial stress–strain relations, and dimensions of porcine coronary artery and internal mammary were compared by van Andel et al.16 The internal diameter, burst pressure, suture retention, and compliance of the internal mammary artery and saphenous vein in respect to the tissue engineered blood vessels have compared.6
So far, there has not been a study on the viscoelastic properties of either the ITA or SSV. The viscoelastic behavior of the blood vessel can be important for their performance, because unlike the elastic materials the stress at a given point of a viscoelastic body depends on the strain at that time, and on the strain from the past time which affects the stress. Furthermore, if a material has viscoelastic characterization, due to the damping behavior of the viscous part, its stress and strain response to the loading and unloading would be different. However, the stress–strain relationship during the loading and unloading for each cycle is unique.8 Hence, investigating the behavior of the ITA and SSV from a viscoelastic point of view can give us much needed information about these blood vessels. In this study, the viscoelastic characterizations of the ITA and SSV under cyclic load and at body temperature, as two options for being used as graft for coronary artery bypass grafting, have been investigated.
Materials and methods
Specimen preparation and mechanical testing
Four SSVs and four ITAs were collected from two male subjects with healthy respective blood vessel. All subjects who donated blood vessel in this study did so voluntarily after giving informed consent under the ethical rules of Baqiyatallah University of Medical Science (BUMS). Five centimeter of each vessel was cut for further use. The SSVs and ITAs then were immersed in solution of 0.90% w/v of NaCl at 4–5 °C before the test. Afterward, both vessels were transversely cut open using a surgical scalpel. Then, two specimens were cut from each vessel. Thickness, length, and width of each specimen were measured via a digital caliper (Insize, Vienna, Austria). The size of the specimens is listed in Table 1.
| Thickness (cm) | Length (cm) | Width (cm) | |
|---|---|---|---|
| ITA tension specimen | 0.80 | 7.14 | 7.45 |
| ITA compression specimen | 0.70 | 14.20 | 5.00 |
| SSV tension specimen | 0.40 | 7.14 | 7.51 |
| SSV compression specimen | 0.43 | 11.58 | 5.56 |
The dimensions of the specimens.
Both tensile and compressive tests were performed by the TT DMA (Triton Technology, AZ, United States). One specimen from each vessel was used for the tensile test, and similarly one specimen for the compressive test. Specimens were mounted on the tensile and compressive clamps of the TT DMA machine for the tensile and compressive tests. Since the mechanical behavior of a vessel in radial direction usually is the subject of the mechanical analysis,17,18 its mechanical properties in that direction are of extra importance. Material properties of the SSV and ITA in the circumferential and axial directions were assumed to be the same. However, the SSV and ITA are considered to have different material properties in the radial direction. As a result, a tensile test, where the specimen was positioned at 45° angle, was performed to determine its material properties in both the circumferential and axial directions, and a compressive test was performed to obtain the viscoelastic properties of each blood vessel in the radial direction. For the tensile test, the jaws of the device were 5 cm apart. In both tests, a sinusoidal dynamic force with a base static force as well as a peak dynamic force was applied to the specimens. All tests were performed at the temperature of 37 ± 1 °C and under varying frequencies from 1 to 2 Hz. Variations of the frequency with time for each test are illustrated in Fig. 1.
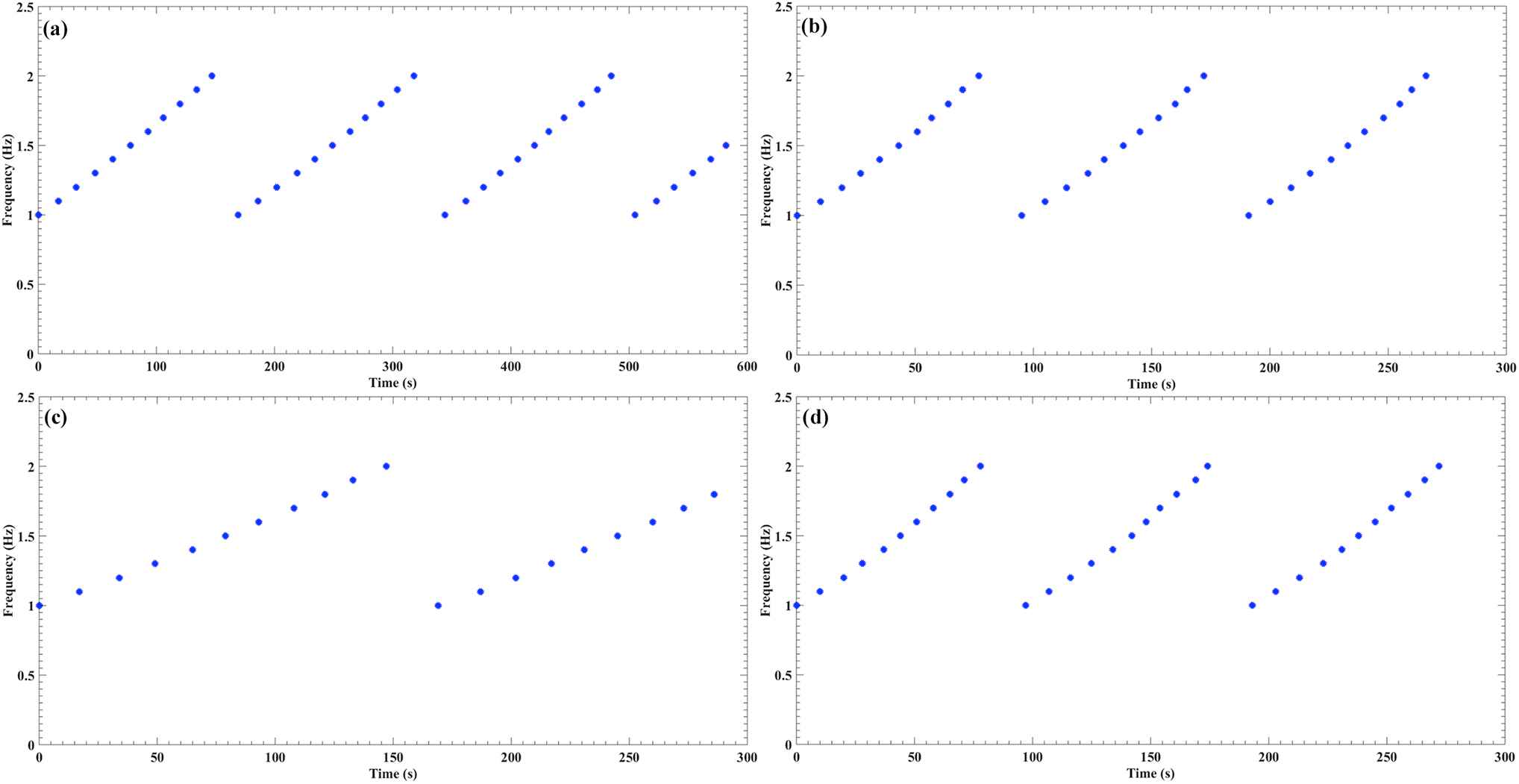
Alterations of the loading frequency versus the time in all tests, including the (a) ITA tension, (b) ITA compression, (c) SSV tension, and (d) SSV compression.
Viscoelastic model
Most biological materials show viscoelastic behavior. Viscoelastic materials have an elastic component and a viscous component. Upon application of a periodic load, the viscoelastic material will respond with a periodic strain. The strain of a viscoelastic body is out of phase with the applied stress, by the phase angle of δ. This phase lag is due to the excess time necessary for molecular motions and relaxations to occur. Therefore, relation between stress and strain can be described as Equation (1). Where σ, ε, E′, and E″ are, respectively, define as the stress, strain, storage modulus, and loss modulus. Equations (2) and (3) display the relation of the storage and loss modulus with the stress and strain, respectively.8,19
The storage modulus usually describes stiffness of a material and loss modulus associates with the internal friction of a material. In the viscoelastic materials, the modulus is a function of the time at a constant temperature, meanwhile at a given time the modulus varies with temperature.
Results
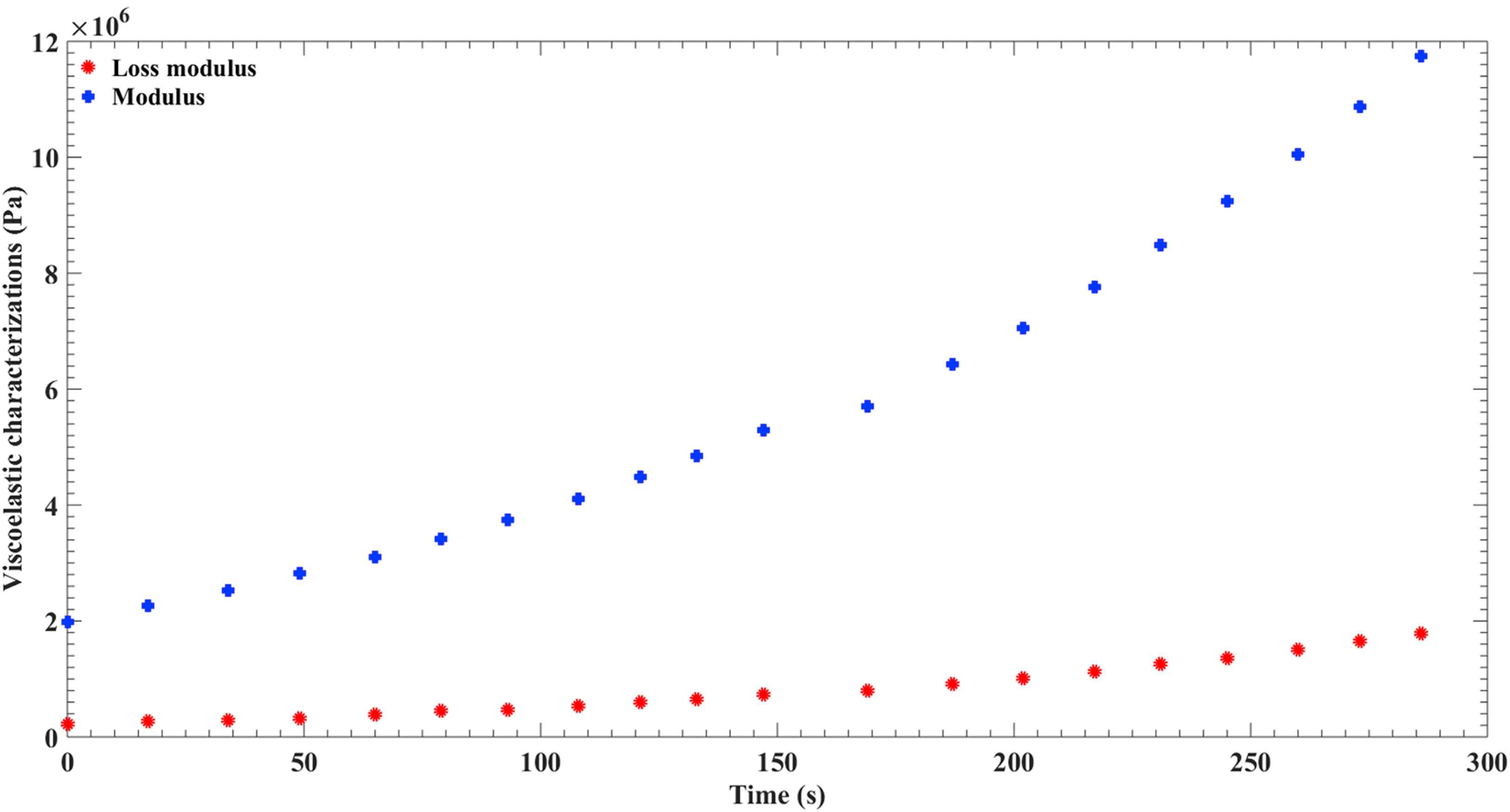
The result of the viscoelasticity is to convert the pulsatile ejection of the heart into a continuous flow, storing a part of the energy of propulsion in systole and restoring it to the circulation during diastole.20 Therefore, the viscoelasticity is important in energy transfer and dissipation. Figure 2 exhibits the shear modulus and loss modulus of the ITA in compression while modulus and loss modulus of this artery in tension is plotted in Fig. 3. ITA had higher shear modulus in tension, while loss modulus of tension and compression were not considerably different, this leads to a lower phase different of the ITA in the radial direction in comparison to the other directions.
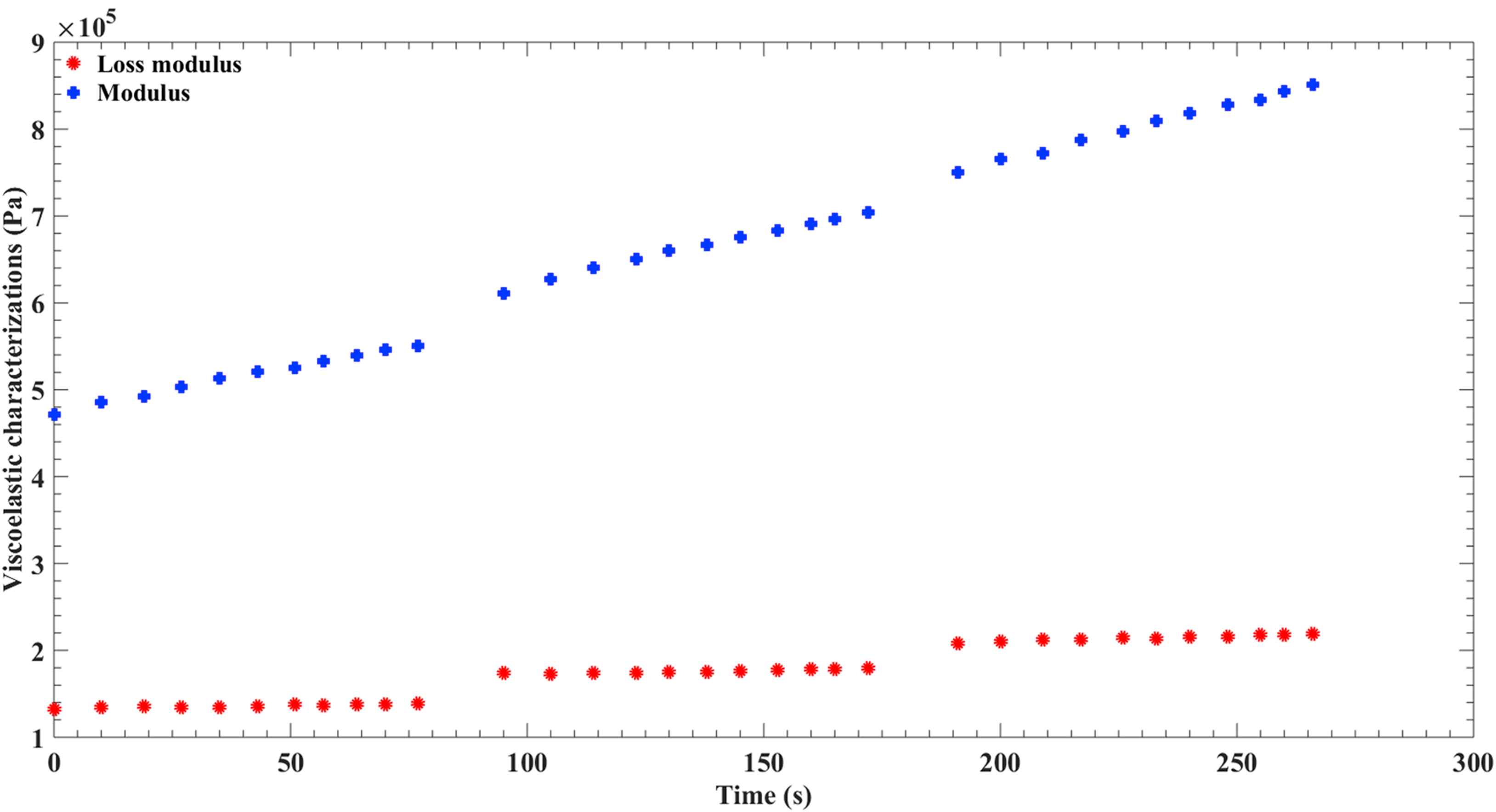
Alterations of the loss modulus and modulus of the ITA versus the time in compression.
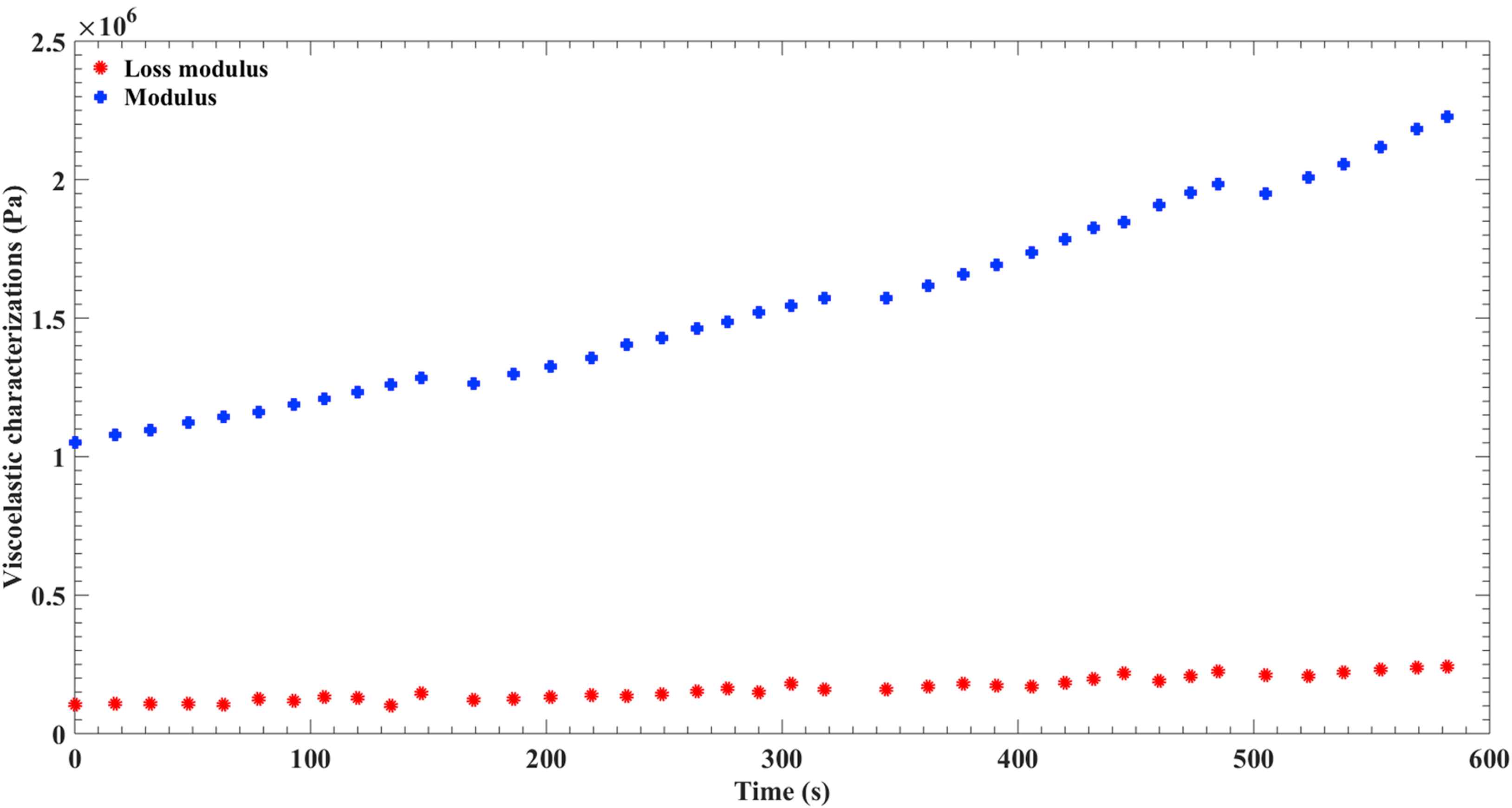
Alterations of the loss modulus and modulus of the ITA versus the time in tension.
Modulus and loss modulus of the SSV in compression and tension are demonstrated in Figs. 4 and 5, respectively. While both modulus and loss modulus of the SSV were meaningfully higher in compression, phase different between the stress and strain was not pointedly different, in the different directions. Furthermore, while SSV showed higher modulus and loss modulus compared to the ITA, the difference in the radial direction was much more than the difference in the other directions.
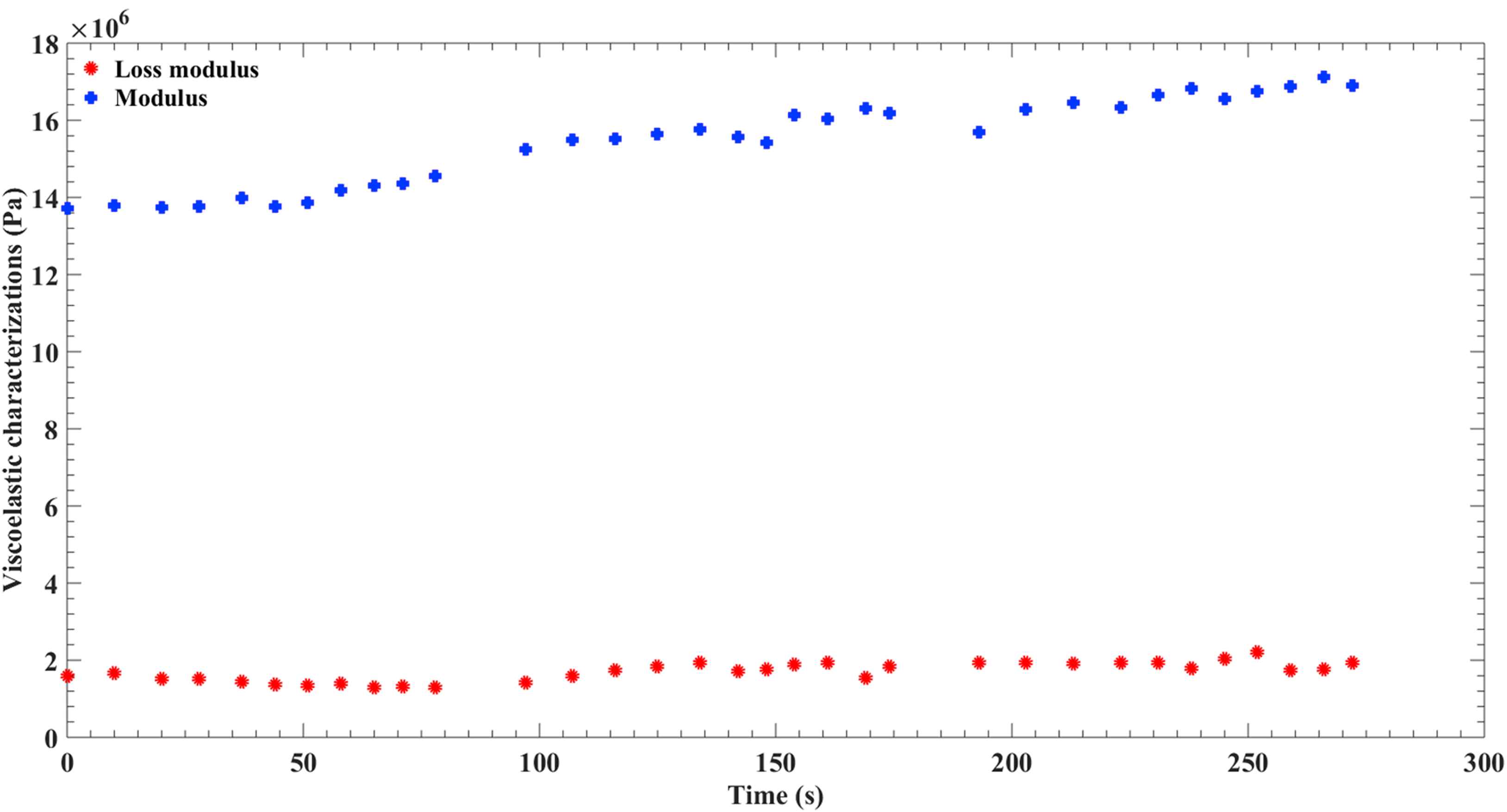
Alterations of the loss modulus and modulus of the SSV versus the time in compression.
Alterations of the loss modulus and modulus of the SSV versus the time in tension.
For the practical use of these information for simulation purposes, one storage modulus and one loss modulus at any given direction for each blood vessel are needed. Therefore, values of storage and loss modulus in form of Mean ± SD for both blood vessels have been shown in Table 2.
| Storage modulus (MPa) | Loss modulus (MPa) | tan(δ) | |
|---|---|---|---|
| ITA tension | 1.55 ± 0.34 | 0.16 ± 0.04 | 0.10 ± 0.01 |
| ITA compression | 0.66 ± 0.12 | 0.17 ± 0.03 | 0.26 ± 0.01 |
| SSV tension | 5.79 ± 2.94 | 0.82 ± 0.48 | 0.13 ± 0.01 |
| SSV compression | 15.45 ± 1.12 | 1.7 ± 0.24 | 1.10 ± 0.01 |
Average values of the storage modulus, loss modulus, and tan(δ).
Discussion
Coronary artery disease is the leading cause of the death in the world, accounting for more than 7 million deaths per year, which is more than 13% of whole deaths worldwide.21–24 One of the most effective treatments against coronary artery disease is bypass grafting.25,26 In coronary artery bypass grafting, flow of blood would be redirected from the diseased part of its original path to a bypassing channel. The bypass graft itself can be affected by common blood vessel diseases. Furthermore, undesirable mechanical properties of the bypass graft can lead to an inadequate performance or even failure of the graft. Therefore, understanding of the bypass graft can be useful in coronary artery management.
There are several options for the bypass channel in the coronary artery bypass grafting. The most common bypass grafts are autologous grafts, where one blood vessel from a person is used as the bypass channel for the same person. Another type is the bypass grafts that are made of synthetic materials, such as Dacron or PTFE. These grafts have been widely used, however, they have shown a lower patency compared to the biological ones.20 Even though there are a lot of researches and promises in that area, so far there is no viable bypass graft that can be used in the coronary artery bypass grafting.6,20 Due to these conditions autologous grafts are gold standard in coronary artery bypass surgery. A few blood vessels have been used as channel to bypass the diseased part of the coronary artery. One of them is ITA, otherwise known as mammary artery. This artery has been one of the first blood vessels to be used as a coronary artery bypass graft and has shown excellent long term patency.27,28 Another blood vessel that has been used as a bypass channel for coronary artery is the SSV. Although this vein is not used as widely as the great (long) saphenous vein but nevertheless is a viable candidate for coronary artery bypass grafting.3,4,29
Arteries have to deal with higher pressure than veins, therefore they have lower stiffness which is a result of the higher collagen to elastin ratio.30 Furthermore, veins have much lesser smooth muscle than arteries which usually leads to a lower wall thickness in comparison to an artery with similar diameter.31 SSV and ITA are not an exception from this. Results of the current study showed that the modulus of the ITA is two order of magnitude lower than that of the SSV, while its thickness is about twice as much. Furthermore, while the loss modulus of SSV was higher than ITA, the difference was not as high, which means that SSV is much stiffer than ITA and has lesser viscous properties. Viscoelastic properties of the ITA and SSV were closer in tension. While still ITA was less stiff and more viscous, their difference phase angle was 1.77°, down from 8.59° and the shear modulus of the SSV was 3.73 times lower than that of the shear modulus of the ITA down from being more than 23 times in compression. It is interesting to notice that the SSV was stiffer and more elastic in the radial direction while the ITA showed a lower stiffness and a more viscous behavior in the same direction. Even though the SSV reported to have a higher compliance than that of the great saphenous vein,32 but still is much stiffer than ITA.
Conclusion
In this study the viscoelastic behavior of the SSV and ITA under the periodic load and body temperature has been investigated. Results of this study showed that the SSV has much higher stiffness and less viscous behavior than that of the ITA, and even more so in radial direction. Even though mechanical behavior of the SSV is far from a rigid tube, but from a mechanical point of view it is much closer to a rigid tube than ITA. Results of this study can be used as the input for the numerical or analytical analysis of these blood vessels, either in their original place, as a bypass graft or any other simulation purposes. Due to the lack of data on the viscoelastic behavior of the blood vessels or difficulties in the numerical simulations, most of the mechanical simulations of the blood vessels assume whether elastic or rigid in their modeling and ignore the viscous behavior of the blood vessels.33–35 While this assumption can be sufficient in some studies on the less viscous blood vessels but it is not valid for the arteries, such as the ITA that have a significant viscoelastic behavior.
Conflicts of interest
None declared.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethical issues
The application of the human tissue was confirmed by the ethical committee of the Baqiyatallah University of Medical Science (BUMS) under the supervision of the Iranian Ministry of Health with the letter number of 2597/1395. The medical approval is adhered to declaration of Helsinki.
References
Cite this article
TY - JOUR AU - Arezoo Khosravi AU - Milad Salimi Bani AU - Hossein Bahreinizad AU - Alireza Karimi PY - 2017 DA - 2017/07/22 TI - Viscoelastic properties of the autologous bypass grafts: A comparative study among the small saphenous vein and internal thoracic artery JO - Artery Research SP - 65 EP - 71 VL - 19 IS - C SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2017.06.007 DO - 10.1016/j.artres.2017.06.007 ID - Khosravi2017 ER -
