Transcranial Doppler evaluation of cerebral hemodynamic alteration in preterms with early onset neonatal sepsis
- DOI
- 10.1016/j.artres.2017.06.004How to use a DOI?
- Keywords
- Transcranial Doppler; Cerebral hemodynamics; Preterm; Early-onset neonatal sepsis
- Abstract
Objective: To evaluate the cerebral blood flow and the cerebral hemodynamic alteration by Doppler ultrasound in preterms with early onset-neonatal sepsis.
Method: Total forty two preterms divided into two groups whether with clinical and laboratory diagnosis of early onset neonatal sepsis (EONS) or not. Both groups assessed with Doppler Ultrasound of the anterior (ACA) and middle (MCA) cerebral arteries, with the peak systolic velocity (PSV), end diastolic velocity (EDV), resistivity index (RI) and pulsatility index (PI) calculation and recording.
Results: Statistically significant lower RI (p: .0001), lower PI (p: .0001) in both the ACA and MCA in the group with neonatal sepsis, in comparison with the group with no clinical evidence of neonatal sepsis.
Conclusion: Study results showed vasodilatation and reduced resistance in the cerebral arteries in preterms with early onset neonatal sepsis.
- Copyright
- © 2017 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Introduction
Worldwide annual 1 million neonatal deaths is attributed to neonatal sepsis alone.1
Neonatal sepsis is defined classically as a clinical syndrome characterized by systemic signs of infection frequently accompanied by bacteremia.2
Two types of neonatal sepsis have been observed: early-onset disease, when features of sepsis appear during the first 72 h of birth; and late-onset disease, where the disease manifests beyond 72 h. Early-onset neonatal sepsis is acquired in utero resulting in chorioamnionitis.3
Hospital-born babies in developing countries are at increased risk of neonatal infections because of poor intrapartum and postnatal infection-control practices. The reported rates of neonatal infections in developing countries were 3–20 times higher than those reported for hospital-born babies in industrial countries.4
Cerebral blood flow (CBF), as measured by Doppler Ultrasound, has been studied mainly to help determine whether alterations have occurred in the neonatal cerebral circulation that could result in brain damage and adverse developmental outcomes. Establishment of the predictive validity of the cerebral blood flow measured by Doppler ultrasound is essential to ensure their usefulness in the early assessment and interpretation of hemodynamic changes.5
Studying the cerebral blood flow in neonatal sepsis is of concern because, the brain of the newborn is highly susceptible to blood flow fluctuations. Moderately elevated CBF can increase the risk of cerebral hemorrhage whereas moderate hypoperfusion can expose the brain to ischemic damage.6
Previous studies on EONS were performed giving results of significantly lower resistance, vasodilatation, and higher blood flow were noted in all the cerebral arteries of the sepsis group.7
In our study we aimed to evaluate the cerebral hemodynamic of the preterms with early onset neonatal sepsis using Doppler ultrasound.
Methods
Patient population
Forty-two patients from the Neonatal intensive care unit (NICU) were enrolled in this cross-sectional study. They were eligible if they had a gestational age less than 37 weeks.
An informed oral consent was obtained from all patients’ parents – the guardians – before involving them in the study as no interventional process was done and there was no perceived risk. The steps of the study, the aims and the procedure were discussed with the parents of the study group. Confidentiality of all data was ensured. All the human studies have been approved by the ethics committee of the university Hospital and have therefore been performed in accordance with the ethical standards laid down in the Helsinki Declaration of 1975 and its late amendment.
Inclusion criteria
We included neonates with presence of foul smelling liquor or two of the following risk factors as those are high-risk factors – preterm is already a risk factor – which have been associated with an increased risk of early onset sepsis
- •
Foul smelling and/or meconium stained liquor
- •
Prolonged rupture of membranes >24 h.
- •
More than 3 vaginal examinations during labor
- •
Prolonged and difficult delivery with instrumentation
Two laboratory criteria (WBC <5000 or <20,000 ×109 cells/L; I/T ratio > 0.2; platelet count <100,000 × 109/L.8
And who showed clinical symptoms & signs of the following:
- •
Respiratory compromise: tachypnea, increased apnea and increased desaturations.
- •
Metabolic changes: hypothermia, hyperthermia, feeding intolerance, glucose instability, metabolic acidosis.
- •
Neurological changes: lethargy, hypotonia, decreased activity.
Exclusion criteria
Perinatal asphyxia, Congenital infections, Respiratory distress syndrome, Meconium aspiration syndrome, Congenital heart disease, Hemolytic anemia, Metabolic disorders, Surgical disorders, Gross congenital malformations, small for gestational age.
Neonates with altered arterial blood gas (ABG) parameters, hemodynamic instability, mechanical ventilation, at the time of CBF assessment.
Our patients were divided into 2 groups whether having early onset neonatal sepsis or not; group 1: 28 neonates with clinically and laboratory diagnosis of early onset neonatal sepsis (Sepsis group), group 2: 14 with no signs of early onset neonatal sepsis (Control group).
Clinical and laboratory examination
Full perinatal history was taken to assess for the risk factors for EONS, clinical examination was made at birth to exclude any systemic disease or congenital malformation, laboratory estimation of blood glucose, serum electrolytes, coagulation profile, liver and kidney function tests, ABG, tests to exclude inborn errors of metabolism were recorded.
Around the third day, enrolled subjects were checked for development of clinical signs of neonatal sepsis, and blood culture was taken.
Those who developed the clinical criteria for EONS were enrolled for the sepsis group & those who didn’t were enrolled for the control group.
Transcranial ultrasound and Doppler examination of the brain
Transcranial ultrasound (TCU) was performed and cerebral blood flow (CBF) was assessed by Transcranial Doppler (TCD) ultrasound.
All ultrasound examinations were performed by the same single sonographer, performed with Toshiba Nemio Power vision software 6000 SSA-370A (Toshiba Corporation, Tokyo, Japan) with a 2–4 MHZ sector probe.
The TCU and TCD were performed through the window of the incubator to keep the normothermal condition, the neonate lies supine with lateral tilting of the head to either side during the examination. Small amount of gel was applied during examination, with rapid removal after the examination to avoid hypothermia.
The Middle cerebral artery was insonated using a trans-temporal approach, the probe was placed on the temporal aspect of the head, cephalad to the zygomatic arch and immediately anterior & slightly superior to the tragus of the ear in a transverse position. By using that trans-temporal approach, the beam was angulated anteriorly. The anterior orientation of the beam allowed for the insonation of the first and second segments of the MCA (M1 & M2). When the midbrain was observed, color Doppler was applied and the circle of Willis becomes evident, the MCA is the internal carotid artery branch that is not sharing in it & directed laterally into the Sylvian fissure.
The Anterior cerebral artery was insonated using the trans-fontanelle approach, the probe was placed on the anterior fontanel in a longitudinal position (sagittal position). By using the trans-fontanelle approach, the beam was angulated anteriorly. The anterior orientation of the beam allowed the insonation of the first and second segments of the ACA segments (A1 & A2). When the corpus callosum is observed, color Doppler was applied, the ACA is the branch of the internal carotid artery (ICA) which continues with it and course around the corpus callosum.
The spectral wave analysis was done with an angle of 60°. Sample volume, gain and power were kept constant during the investigation. The peak systolic and end diastolic velocities were manually located on the displayed waves, the resistivity and the pulsatility indices as well as the mean velocity were calculated manually.
Statistical analysis
Data were statistically described in terms of mean standard deviation (SD), median and range, or frequencies (number of cases) and percentages when appropriate. Comparison of numerical variables between the study groups was done using Student t test for independent samples in comparing 2 groups when normally distributed and Mann Whitney U test for independent samples when not normally distributed. For comparing categorical data, Chi square test was performed. Exact test was used instead when the expected frequency is less than 5. p Values less than 0.05 was considered statistically significant. All statistical calculations were done using computer program SPSS (Statistical Package for the Social Science; SPSS Inc., Chicago, IL, USA) release 15 for Microsoft Windows.
Results
Patients
A total of 42 preterm neonates who were delivered and admitted to the NICU, were enrolled in this study after they met the inclusion and exclusion criteria. 28 were included in the case group (sepsis group), where all of them had clinical signs and symptoms of EONS and 14 were included in the control group (non-sepsis group) as they didn’t have clinical signs or symptoms of EONS.
Risk factors for EONS development are demonstrated in Table 1.
| Risk factor | Cases (n: 28) | Percentage (%) | Control (n: 14) | Percentage (%) |
|---|---|---|---|---|
| Vaginal delivery | 20 | 71.4% | 10 | 71.4% |
| Prolonged delivery | 3 | 10.7% | – | 0% |
| >3 vaginal examination | 24 | 85.7% | 12 | 85.7% |
| PMRM | 8 | 28.6% | – | 0% |
| Meconium stained liquor | 3 | 10.7% | – | 0% |
PMRM, premature rupture of membranes.
Risk factors for EONS among the case and control groups.
Absence of clinical or laboratory signs of meningitis or encephalitis in all patients.
In the sepsis group, blood culture was positive in only 5 cases (17.8%).
The patient’s gestational age, clinical and laboratory characteristics of the enrolled neonates are shown in Table 2.
| Clinical/laboratory data | Cases (n: 28) | Control (n: 14) | ||
|---|---|---|---|---|
| Mean ± SD | Median | Mean ± SD | Median | |
| Gestational age | 30.75 ± 1.75 | 30 | 31 ± 1.71 | 31 |
| Apgar score | 8.04 ± 0.96 | 8 | 8.07 ± 0.99 | 8 |
| PO2 | 72.5 ± 1.59 | 72.50 | 72.5 ± 1.65 | 72.50 |
| PCO2 | 38.64 ± 2.00 | 38 | 38.2 ± 2.22 | 38 |
| HCO3 | 18.74 ± 0.40 | 18.70 | 18.7 ± 0.35 | 18.7 |
PO2, pressure oxygen; PCO, pressure carbon dioxide; HCO3, serum bicarbonate.
Clinical and laboratory data of the case and control groups.
Transcranial ultrasound and Doppler examination findings
Transcranial Doppler evaluation of the ACA and MCA among the case and control group reveled statistically significant reduction of the RI and PI in both arteries in the septic cases; whereas the PSV was increased but not statistically significant (Table 3).
| Doppler data | Cases (n: 28) | Control (n: 14) | p Value | |||
|---|---|---|---|---|---|---|
| Mean ± SD | Median | Mean ± SD | Median | |||
| MCA | PSV | 69.2 ± 4.2 | 67.7 | 66.8 ± 4.0 | 67.5 | 0.88 |
| RI | 0.52 ± 0.09 | 0.54 | 0.79 ± 0.05 | 0.80 | 0.0001 | |
| PI | 0.81 ± 0.21 | 0.84 | 1.76 ± 0.26 | 1.72 | 0.0001 | |
| ACA | PSV | 67.5 ± 3.4 | 68.15 | 65.3 ± 3.61 | 67.00 | 0.67 |
| RI | 0.54 ± 0.08 | 0.56 | 0.80 ± 0.04 | 0.80 | 0.0001 | |
| PI | 0.85 ± 0.19 | 0.89 | 1.74 ± 0.24 | 1.70 | 0.0001 | |
MCA, middle cerebral artery; PSV, peak systolic velocity; RI, resistivity index; PI, pulsatility index; ACA, anterior cerebral artery.
Doppler data of the case and control groups.
Outcome
Among the sepsis group, five patients (17.9%) showed signs of intraventricular hemorrhage (IVH) in cranial ultrasonography during their hospital stay & three of them (60%) (10.7% of total no. of cases) died during their hospital stay.
Table 4 is showing prospective data from two cases.
| Case 1 | Case 2 | |
|---|---|---|
| Sex | Female | Male |
| GA (weeks) | 30 | 31 |
| Birth weight (kg) | 1.385 | 1.4 |
| Mode of delivery | Vaginal delivery | Vaginal delivery |
| Risk factors |
|
|
| Evidence of sepsis | Clinical blood culture | Clinical |
| ACA PSV (cm/s) | 72.2 | 62.2 |
| ACA RI | 0.52 | 0.65 |
| ACA PI | 0.79 | 1.15 |
| MCA PSV (cm/s) | 69.5 | 64.2 |
| MCA RI | 0.59 | 0.65 |
| MCA PI | 0.97 | 1.14 |
| Outcome | At day 7, IVH (grade 4) and death | At day 11, IVH (grade 3) |
GA, gestational age; PMRM, premature rupture of membranes; ACA, anterior cerebral artery; PSV, peak systolic velocity; RI, resistivity index; PI, pulsatility index; MCA, middle cerebral artery; IVH, intraventricular hemorrhage.
Prospective data obtained from two cases.
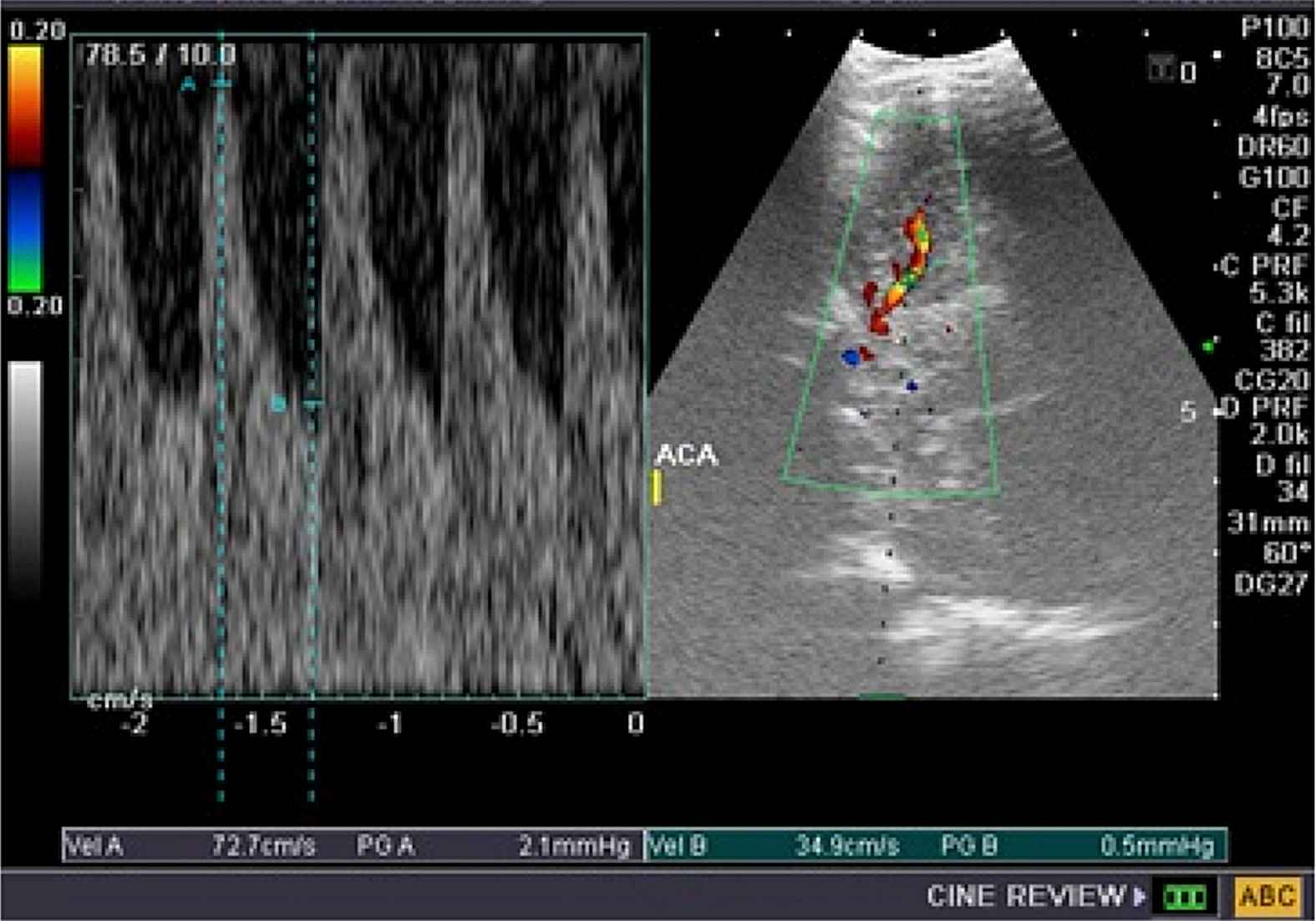
Doppler parameters in the ACA in case 1.
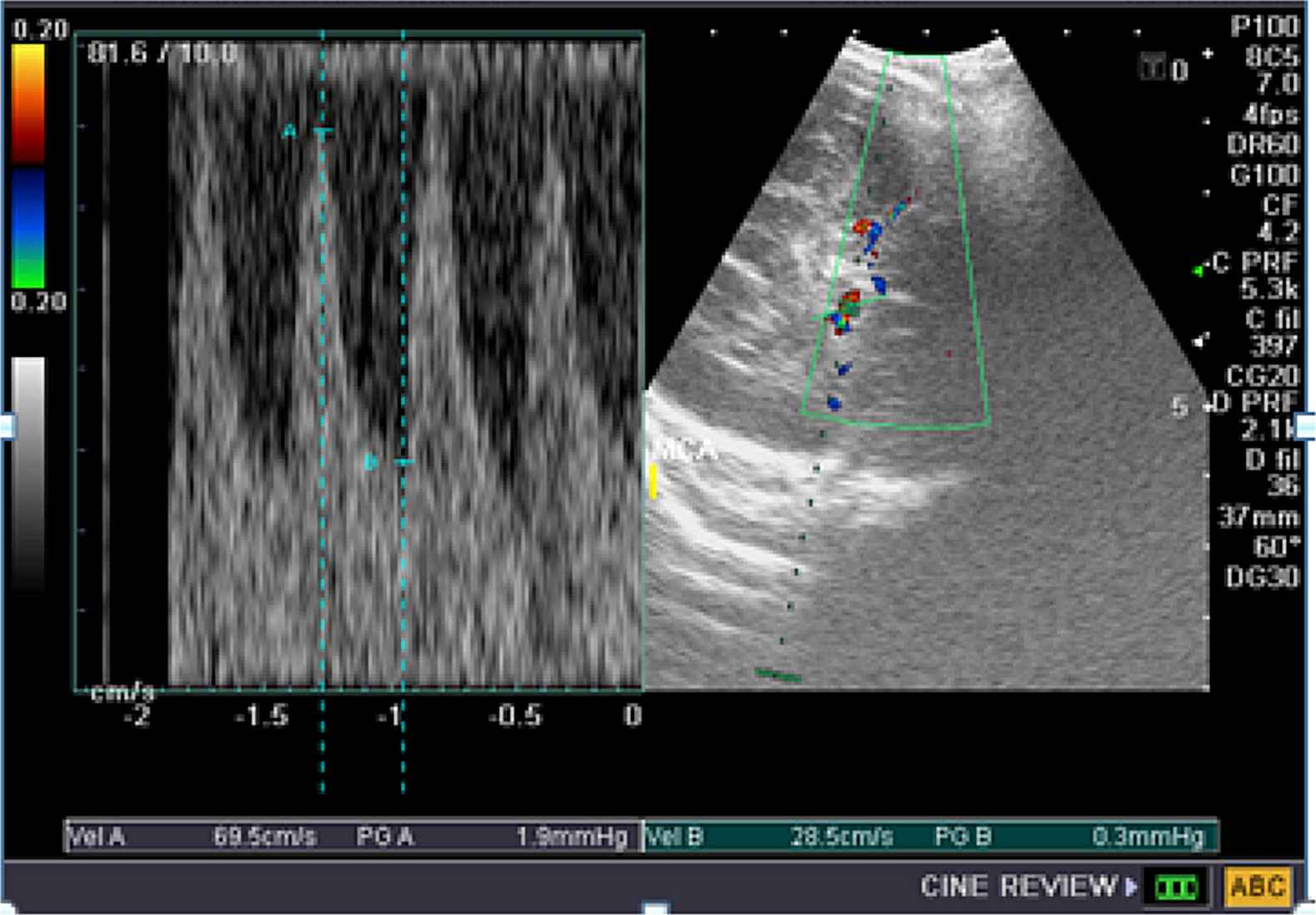
Doppler parameters in the MCA in case 1.
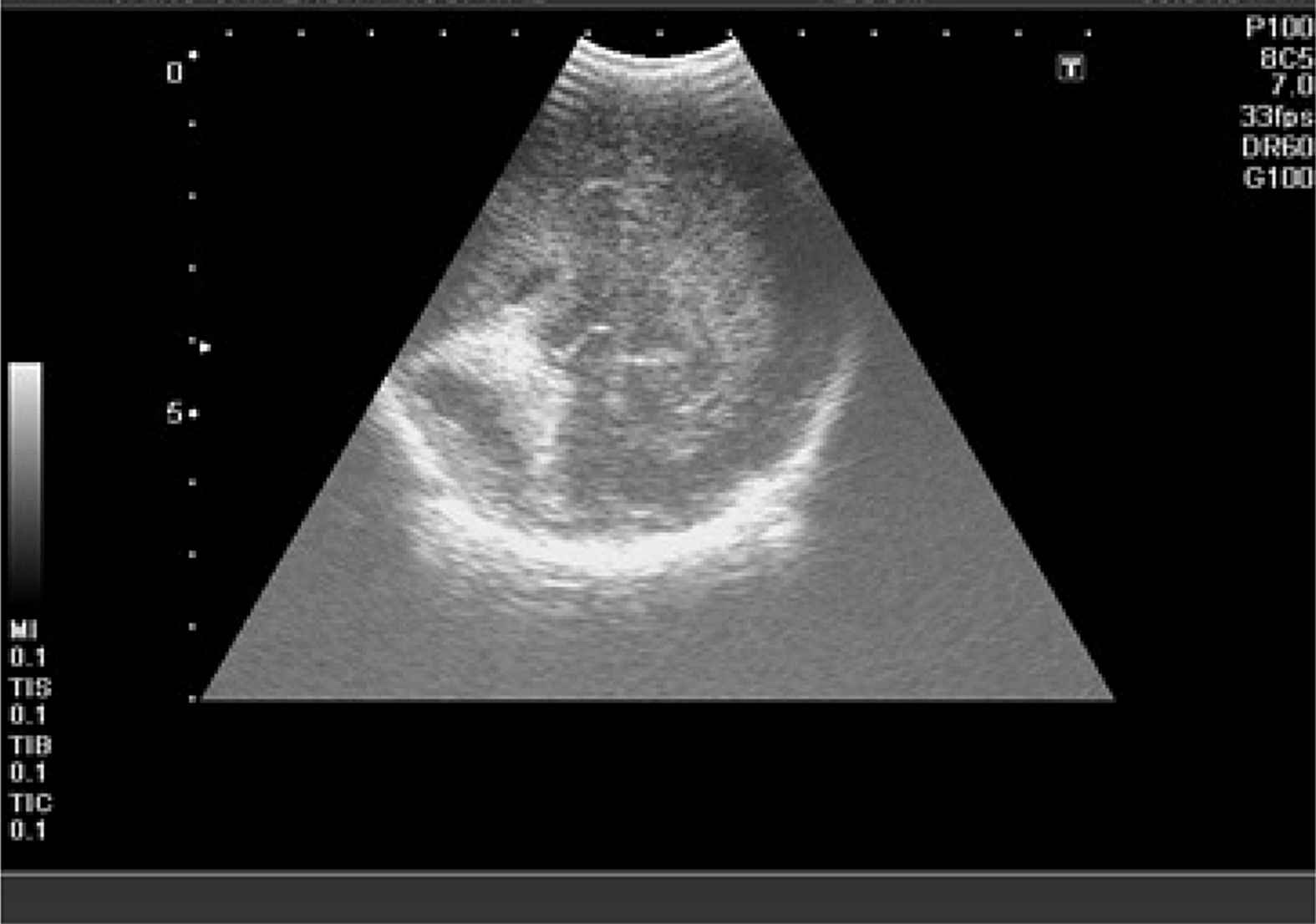
Intraventricular hemorrhage 4th grade in case 1.
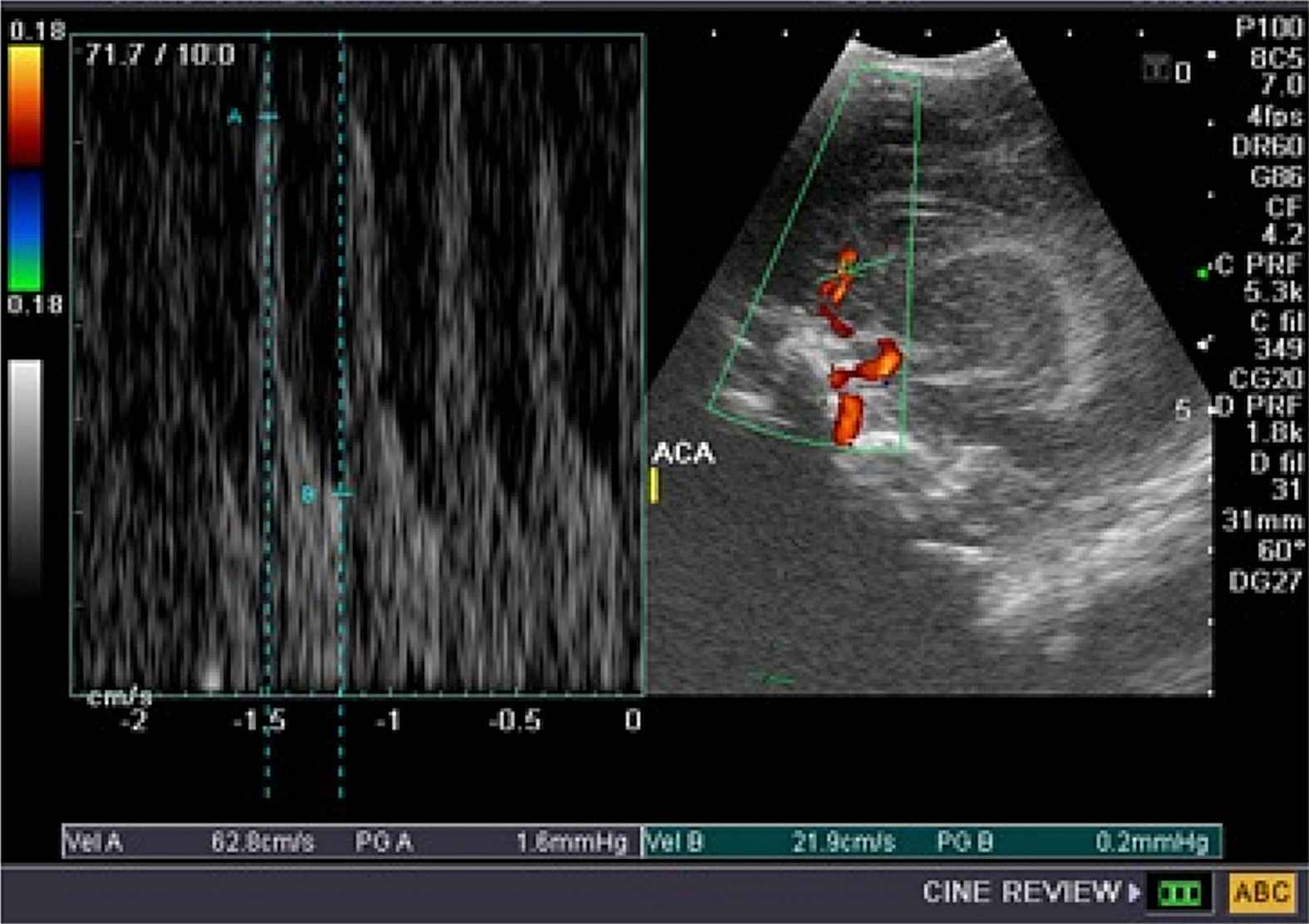
Doppler parameters in the ACA in case 2.
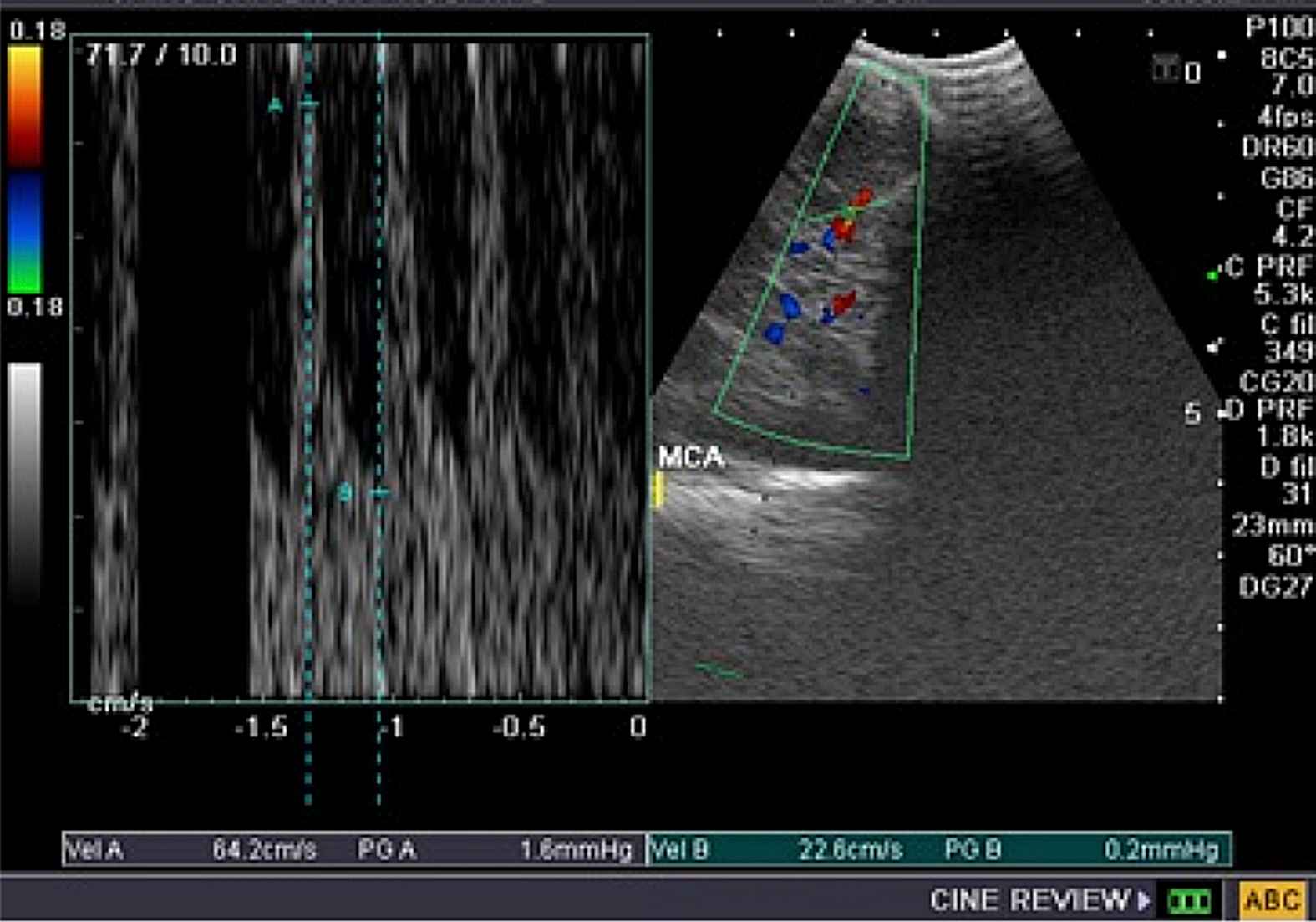
Doppler parameters in the MCA in case 2.

Intraventricular hemorrhage 3rd grade in case 2.
Discussion
Neonatal sepsis is a clinical syndrome characterized by signs and symptoms of infection with or without accompanying bacteremia in the first month of life. It encompasses various systemic infections of the newborn such as septicemia, meningitis, pneumonia, arthritis, osteomyelitis, and urinary tract infections.9 It is classified into two major categories depending upon the onset of symptoms, EON which presents in the first 72 h of life & LON which presents after the first 72 h of life.10
Early onset sepsis (EON) is associated with acquisition of microorganism from the mother. Transplacental infection or an ascending infection from the cervix. The microorganisms most commonly associated are the group B Streptococcus, Escherichia coli, Staph, Hemophilus influenza and Listeria.11
Inflammatory challenges of neonatal sepsis lead to activation of fetal immune system, a condition known as fetal inflammatory response syndrome (FIRS). FIRS is initially subclinical but eventual amplification of the inflammatory process manifests after birth in some neonates as systemic inflammatory response syndrome (SIRS), which is clinically diagnosed as EONS.12
The exact nature of cellular and molecular mechanisms of sepsis-induced encephalopathy is still elusive. The impairment of cerebral autoregulation, damage to blood–brain barrier (BBB), and the direct inflammatory effects of free radicals, oxidative stress, and cytokines on glial cells have been speculated to be the contributory factors.13,14
The exact mechanism by which these cytokines access to the cerebral compartment to induce injury is still debatable. Transfer of cytokines across BBB15 and damage of BBB causing increased permeability16 could be the responsible factors. It has also been shown that astrocytes and microglia are capable of producing proinflammatory cytokines during inflammation.17
In the cerebral compartment, proinflammatory cytokines may induce excitotoxicity by modifying the re-uptake of glutamate,18 stimulating the release of free radicals,19,20 or induce the local production of nitric oxide, a potent vasodilator.21
Improvements in critical care medicine have resulted in the increased survival of premature, low birth weight and asphyxiated infants. An integrated clinical and radiological approach to the neurological assessment of such neonates over the past few years has led to a better understanding of the cause and evolution of the cerebral lesions and thus allowed more appropriate medical intervention to favorably alter clinical outcome.22
Changes in cerebral blood flow velocity (CBFV) may have a key role in perinatal brain damage, and both acute and long-term morbidity may be closely related to rapid vascular changes during the early hours of life. Moreover, altered CBF may also be used as a surrogate marker for the diagnosis of EONS also other literature investigated the association of potential risk factors for neurodevelopmental disorders. Children who developed neonatal sepsis were three times more likely to have neuromotor and cognitive development alterations at 12 months of corrected age.23
Color Doppler sonography have broadened applications in pediatric neurosonography for evaluation of cerebral vascular anatomy and perfusion.24 The technique is readily applied at bedside, does not involve ionizing radiation, is cost effective and can be used sequentially.22
In the current study, preterms with diagnosis of EONS were evaluated for their cerebral blood flow velocities and indices, using TCD at day 3; significantly lower resistance (RI and PI), and relatively higher peak systolic velocity in MCA & ACA have been noted in neonates with EONS in comparison to neonates of the control group, indicating generalized increase in CBF as an early response to sepsis and cerebral vasodilatation. This agreed with the study of Sriparna et al. that detected significantly lower resistance (RI and PI), vasodilatation, and higher peak systolic velocity in all the three major cerebral vessels (ICA, MCA and vertebral artery (VA)) documented within 24 h of birth in neonates with EONS, indicating generalized increase in CBF as an early response to sepsis7 and Koch et al. who stated that their chorioamnionitis full terms had decreased resistance in most of the major cerebral vessels compared with controls.25
However in this study the Mean PSV was higher than that detected by Sriparna et al.,7 that could be related to the timing of the performance of the TCD, as they conducted it within the first 24 h after delivery, while in this study was on the 3rd day, & it is documented that there is progressive increase in the CBFV with the postnatal age.6,26
There is a paucity of literature explaining the effect of sepsis on CBF through early cerebrovascular alteration,27 with increase in CBF that could be a part of fetal response to chorio-amnionitis (FIRS).28 Severely disturbed vasomotor reactivity leading to vasodilatation and increased CBF.29–32 Hyperdynamic state and cerebral microcirculatory alterations has been documented in experimental animal models of sepsis,33 also the cardiac dysfunction could be a possible explanation for increases in CBF.34,35
Whereas, other authors have demonstrated decreased CBFV along with higher PI in patients with sepsis.36–38 Reduced CBF is ascribed to the vasoconstriction of the resistance arterioles.37 Increased PI, a parameter for compliance of the vascular bed suggesting cerebral edema or venous congestion, has been found to correlate with poor neurological outcome.39
During their hospital stay, some of the septic preterms developed IVH & three of them died within the one month follow up period by cranial ultrasound, that may be an indicator of the cerebral blood flow alteration relation to the development of IVH, yet the lack of Doppler assessment of the cerebral blood flow at the time of IVH development could not verify this assumption The study was a cross sectional with single-time assessment of CBFV and, therefore, could not assess the fluctuation of CBFV over a period of time & correlate it with the adverse effect. Yet, Sriparna et al. added that within the sepsis group, CBF was further increased in those who expired or had IVH compared to those who had uncomplicated survival.7
Limitations of the study include the relatively small number for assessing the statistical validity of cerebral flow and vascular resistance as a predictor of adverse outcomes and the single measurement of each parameter and not serial measurements that would document reliably the changes over time was done.
Conclusion
The new in the current study that it focused on a relatively vulnerable, under studied group of patients which are the preterms with early onset neonatal sepsis.
In the present work, early onset neonatal sepsis was found to cause increase in Peak systolic velocity and decrease in the resistivity and pulsatility indices, thus causing increase in the cerebral blood flow, which in turn showed increased incidence in Intraventricular hemorrhage among the sepsis group compared with the control group.
So adding Doppler examination to the routine screening of the preterms with EONS by transcranial sonography give insight into the cerebral hemodynamic status among this vulnerable group of patients, with early detection of the increased blood flow.
So clinical care of the preterms with EONS, regarding providing a hemodynamic stability, maintaining normotensive status and avoid activities which can cause further alteration of blood flow, as well as early institution of anti-inflammatory therapy can also be considered in their treatment regimen.
Conflict of interest
We the authors, here, admit that there is no conflict of interest encountered during the study done in this research article.
References
Cite this article
TY - JOUR AU - Rania H. Hashem AU - Yasmin E. Abdalla AU - Yasmen A. Mansi AU - Mohamed H. Shaaban AU - Hassan A. El Kiki PY - 2017 DA - 2017/07/30 TI - Transcranial Doppler evaluation of cerebral hemodynamic alteration in preterms with early onset neonatal sepsis JO - Artery Research SP - 83 EP - 90 VL - 19 IS - C SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2017.06.004 DO - 10.1016/j.artres.2017.06.004 ID - Hashem2017 ER -
