Central blood pressure is associated with trunk flexibility in older adults
- DOI
- 10.1016/j.artres.2017.07.002How to use a DOI?
- Keywords
- Central hemodynamics; Arterial stiffness; Stretching; Aging
- Abstract
Background: Increase in central blood pressure is more predictive of future cardiovascular disease than increased brachial blood pressure. Arterial stiffness causes an early return of the reflected pressure wave to the aorta, with subsequently augmented central systolic pressure. It has been reported that arterial stiffness is associated with poor trunk flexibility; however, the effect of flexibility fitness on central blood pressure remains unclear. The purpose of the present study was to examine the relationship between trunk flexibility and central blood pressure using a cross-sectional design.
Methods: A total of 198 middle-aged (50–64 years) and older (65–75 years) adults participated in this study. We measured central blood pressure, carotid-femoral pulse wave velocity (cfPWV), and sit-and-reach flexibility as an index of body trunk flexibility. Study subjects were divided into either poor- or high-flexibility fitness group for each age category.
Results: Among middle-aged subjects, there were no significant differences in any hemodynamic parameters between the two groups. Among older subjects, the central systolic blood pressure and central pulse pressure in the high-flexibility group were lower than that in the poor-flexibility group. cfPWV was also lower in older subjects with high flexibility than those with poor flexibility. Furthermore, sit-and-reach flexibility was significantly correlated with central systolic blood pressure and central pulse pressure.
Conclusion: We demonstrated that trunk flexibility is correlated to central systolic blood pressure and pulse pressure in the elderly.
- Copyright
- © 2017 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Introduction
Increased blood pressure and arterial stiffness are independent risk factors for cardiovascular disease, morbidity, and mortality.1,2 Central aortic blood pressure is a better predictor of cardiovascular outcomes than brachial blood pressure.3 Central blood pressure is composed of an incident wave and reflected waves.4 As arterial stiffness increases, the transmission velocity of the reflected wave increases and the pressure overlap of the reflected and incident waves is augmented during late systole. Hence, an increase in the pulsatile component of central aortic pressure, mainly because of an elevated systolic peak pressure and augmentation pressure, is considered to more accurately indicate left ventricular afterload, carotid intima–media thickness, and peripheral organ damage.5,6 It has been reported that central systolic blood pressure and pulse pressure increase with advancing age as well as arterial stiffness.7 Furthermore, pulsation of central blood pressure represented a greater indicator of cardiovascular and cerebrovascular risk than pulse wave velocity. In addition, Roman et al. documented that, after adjusted with taking of antihypertensive medication, only central pulse pressure remained as an independent predictor of cardiovascular outcome.3 Xu et al. reported that central pulse pressure was a stronger correlate of the cerebral flow pulsatility of middle cerebral artery than aortic pulse wave velocity.8 Therefore, the management of age-related increase in central blood pressure may be of great pathophysiological importance.
Central blood pressure is often treated by non-pharmacological therapy. Our group demonstrated that central blood pressure decreased after life-style modification (exercise and diet) concurrently with a reduction in arterial stiffness in overweight and obese men.9,10 Laskey et al. reported that a 20-week exercise rehabilitation program decreased central systolic pressure in patients with coronary heart disease.11 These studies imply that higher levels of physical fitness appear to prevent arterial deterioration. Furthermore, trunk flexibility, which is one of the physical fitness parameters, is associated with pulse wave velocity in the elderly.12 Taken together, it is possible that poor flexibility-related arterial stiffening induces increase in central blood pressure. However, the effect of trunk flexibility on central blood pressure in middle-aged and older individuals has not yet been examined. Therefore, the purpose of this study was to examine the relationship between trunk flexibility, central blood pressure and arterial stiffness in middle-aged and older individual.
Methods
Subjects
A total of 198 adults (39 men and 159 women), middle-aged (50–64 years) and older (more than 65 years) adults participated in this study. None of the subjects had smoking habits or received cardiovascular-acting medication or hormone replacement therapy. We excluded subjects with abnormal blood chemistries, history of angina, arrhythmia, heart failure, stroke, cardiovascular and cerebrovascular disease, and diabetes mellitus. All potential risks associated with the study were explained to the subjects, and written informed consent with regard to participation in the study was provided by all participants. All procedures were reviewed and approved by the ethical committee of the University of Tsukuba.
Procedures
All experiments were conducted in the morning after a 12-h overnight fast. Subjects abstained from alcohol and caffeine for at least 12 h and did not exercise for at least 24 h before beginning the experiment so as to avoid the potential acute effects of exercise. Measurements were performed in a quiet, temperature-controlled (24–26 °C) room. We measured central blood pressure, arterial stiffness, and flexibility. To assess the effects of flexibility on central blood pressure, the subjects were furthermore divided into a poor- or a high-flexibility group on the basis of the median value of a sit-and-reach test.
Measurements
Blood pressure
Arterial pulse waves of the left radial artery were measured non-invasively by an automated tonometric system (HEM-9000 AI, Omron Healthcare, Kyoto, Japan), with the study individuals in a seated position. The wave was calibrated to simultaneously measure brachial blood pressure in the right brachium with an oscillometric device. Late systolic blood pressure in the radial artery was used as an estimate of the central systolic blood pressure.13 Central pulse pressure was calculated from central systolic blood pressure and brachial diastolic blood pressure (central pulse pressure = central systolic blood pressure − brachial diastolic blood pressure).9
Pulse wave velocity
Carotid-femoral pulse wave velocity (cfPWV) was measured as an indicator of arterial stiffness by a semi-automated vascular testing system, as similar to our previous report.14 Briefly, carotid and femoral pressure waves were obtained by two applanation tonometry sensors incorporating an array of 15 transducers (Form PWV/ABI, Colin Medical Technology, Komaki, Japan). The distance between the left common carotid and femoral arterial recording sites divided by the transit time enabled the calculation of cfPWV.
Flexibility
Flexibility was measured by a sit-and-reach test using a flexibility-testing device (Yagami Inc., Nagoya, Japan). Subjects were seated on the floor, with the hip, back, and occipital region of the head touching the wall and with legs held straight by the tester. They put both hands on the device with their arms held straight, and the device was set to zero. Participants were then asked to slowly bend forward and reach as far forward as possible. The best bout of two trials was recorded.15 The subjects were divided into either poor- or high flexibility group on the basis of the median value of a sit-and-reach value in each age category and each sex.
Blood samples
Blood samples were collected from the antecubital vein after overnight fasting. Serum total cholesterol, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, and triglycerides were determined using standard enzymatic techniques.
Physical activity
Physical activity levels and step counts were assessed using a uniaxial accelerometer for consecutive one week (Lifecorder, KENZ, Nagoya, Japan). The activity level was subsequently converted using an algorithm to calculate energy expenditure (kcal).
Statistical analyses
All data are expressed as mean ± standard deviation (SD). A two-way analysis of variance (age and flexibility) was performed to identify any interaction or main effect. The Bonferroni post hoc test was used to identify significant difference among mean values, when indicated for a significant main effect or interaction. Since the data were not normally distributed based on a Kolomogorov–Smirnov test, Spearman’s rank-order correlation analyses were applied to determine the relationship between variables of interest. Partial correlation coefficients were adjusted with regard to age, sex and arterial stiffness. Statistical data analyses were performed using SPSS software and statistical significance was set a priori at P < 0.05 for all comparisons.
Results
Table 1 shows the characteristics of the study participants. There were no significant differences in terms of height, weight, total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides, brachial diastolic blood pressure, heart rate, physical activity or daily steps between the poor and high flexibility groups in both age categories. Brachial systolic blood pressure was higher in the older poor-flexibility group than in the middle-aged poor-flexibility group. In older categories, brachial systolic blood pressure in the high-flexibility group was lower than that in the poor-flexibility group. Table 2 shows the effect of age and flexibility on central hemodynamics. With regard to cfPWV, central systolic blood pressure, and central pulse pressure, values were higher in the older poor-flexibility group compared with the middle-aged poor-flexibility group. In older subjects, cfPWV, central systolic blood pressure, and central pulse pressure were lower in the high-flexibility group than in the poor-flexibility group. Meanwhile, there were no significant differences in any central hemodynamic parameters in middle-aged subjects.
| Middle-aged | Older | |||
|---|---|---|---|---|
| Poor flexibility | High flexibility | Poor flexibility | High flexibility | |
| n (men/women) | 66 (10/56) | 64 (10/54) | 35 (9/26) | 33 (10/23) |
| Age, years | 58 ± 4 | 58 ± 4 | 69 ± 4# | 68 ± 3# |
| Height, cm | 158 ± 6 | 159 ± 7 | 156 ± 8 | 158 ± 7 |
| Weight, kg | 56 ± 9 | 57 ± 9 | 54 ± 10 | 56 ± 7 |
| Total cholesterol, mg/dL | 221 ± 40 | 229 ± 31 | 231 ± 30 | 221 ± 31 |
| HDL cholesterol, mg/dL | 71 ± 21 | 70 ± 20 | 70 ± 18 | 68 ± 17 |
| LDL cholesterol, mg/dL | 132 ± 37 | 140 ± 28 | 140 ± 26 | 133 ± 29 |
| Triglyceride, mg/dL | 87 ± 47 | 85 ± 36 | 89 ± 42 | 95 ± 43 |
| Brachial SBP, mmHg | 123 ± 17 | 127 ± 20 | 134 ± 18# | 124 ± 13* |
| Brachial DBP, mmHg | 74 ± 10 | 78 ± 10 | 74 ± 12 | 72 ± 9 |
| Heart rate, beats/min | 64 ± 9 | 61 ± 10 | 64 ± 9 | 62 ± 8 |
| Sit-and-reach, cm | 33 ± 6 | 47 ± 5* | 33 ± 7 | 45 ± 6* |
| Physical activity, kcal/day | 214 ± 95 | 231 ± 105 | 225 ± 92 | 218 ± 94 |
| Step counts, steps | 9037 ± 3243 | 8944 ± 3000 | 9438 ± 2924 | 8806 ± 2971 |
Values are means ± SD. HDL: high-density lipoprotein, LDL: low-density lipoprotein.
P < 0.05 vs. the poor flexibility,
P < 0.05 vs. the middle-aged.
Characteristics of the subjects.
| Middle-aged | Older | |||
|---|---|---|---|---|
| Poor flexibility | High flexibility | Poor flexibility | High flexibility | |
| cfPWV, cm/s | 1060 ± 183 | 1030 ± 158 | 1198 ± 220# | 1092 ± 160* |
| Central systolic blood pressure, mmHg | 116 ± 17 | 120 ± 20 | 127 ± 20# | 118 ± 14* |
| Central pulse pressure, mmHg | 42 ± 11 | 42 ± 13 | 53 ± 14# | 45 ± 9* |
Values are means ± SD. cfPWV: carotid-femoral pulse wave velocity.
P < 0.05 vs. the poor flexibility,
P < 0.05 vs. the middle-aged.
Central arterial hemodynamics in poor- or high-flexibility group.
Figure 1 shows the relationships between sit-and-reach flexibility and cfPWV, central systolic blood pressure and central pulse pressure for both age categories. cfPWV, central systolic blood pressure and central pulse pressure were negatively correlated with sit-and-reach flexibility in older subjects (P < 0.05). After adjusting for age and sex, a significant relationship was observed between sit-and-reach flexibility and central systolic blood pressure and central pulse pressure in the older-age category (P < 0.05). However, there was no significant correlation between sit-and-reach flexibility and central systolic blood pressure or central pulse pressure after adjusting for cfPWV in addition to age and sex. Meanwhile, no significant correlations were observed in the middle-aged group.
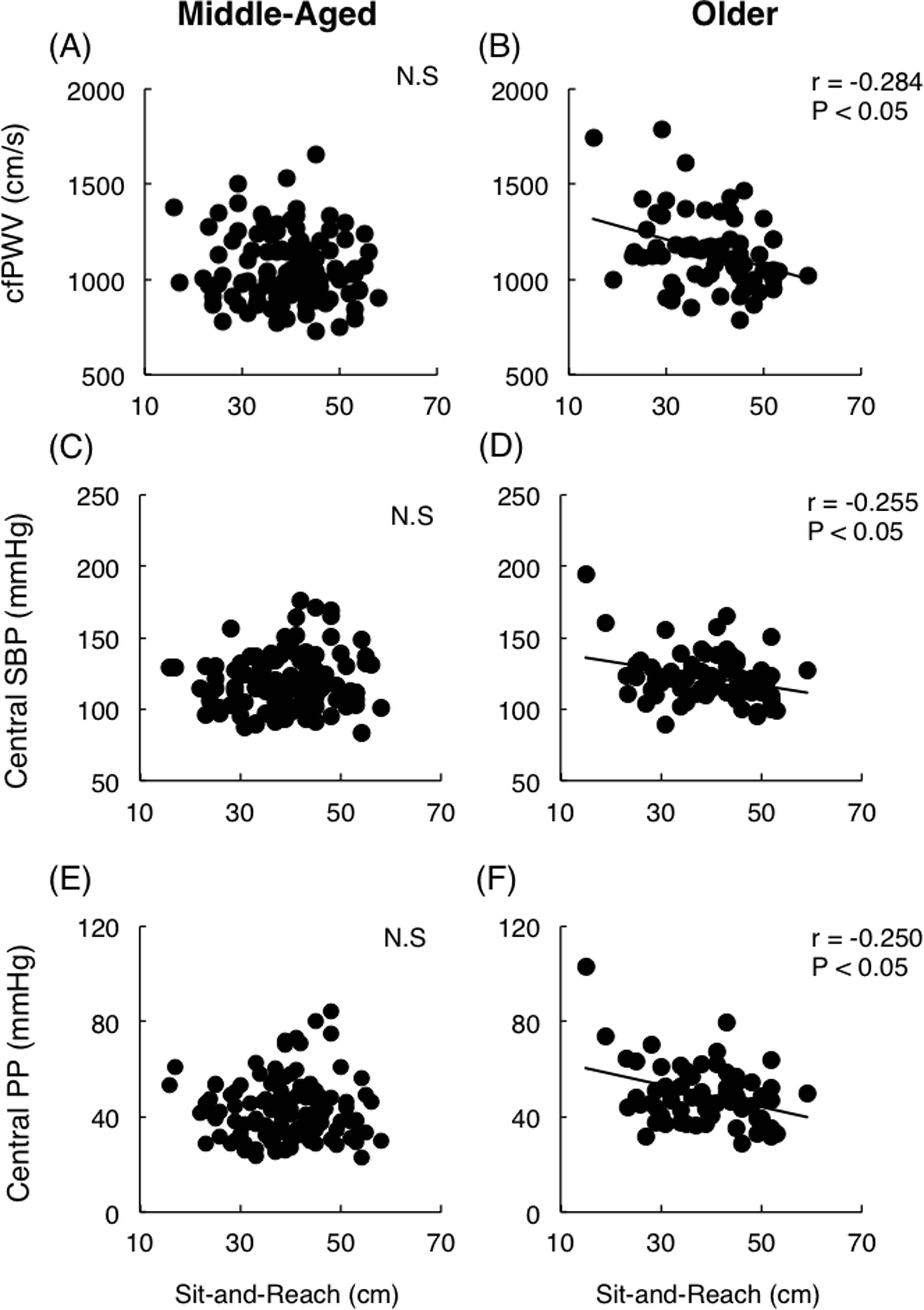
The relationship between sit-and-reach flexibility and carotid-femoral pulse wave velocity in middle-aged (A) and older (B) individuals, between sit-and-reach flexibility and central systolic blood pressure in middle-aged (C) and older (D) individuals, and between sit-and-reach flexibility and central pulse pressure in middle-aged (E) and older (F) individuals. cfPWV, carotid-femoral pulse wave velocity; SBP, systolic blood pressure; PP, pulse pressure.
Discussion
In the present study, we investigated the relationship between sit-and-reach flexibility and central blood pressure in middle-aged and older individuals. We demonstrated that elderly subjects with poor flexibility exhibited higher central systolic blood pressure and pulse pressure than those with high flexibility. Moreover, sit-and-reach flexibility was weakly but significantly correlated with central systolic blood pressure and central pulse pressure in the elderly. These findings suggest that greater flexibility fitness is associated with attenuating the age-related increase in central blood pressure.
The aorta and carotid arteries are rich in elastic components. Compliant artery has ability to buffer the pulsatile pressure wave and delay the reflected wave arriving from the periphery.16 It has been reported that aging leads to an increase in arterial stiffness, a hastened arrival of the reflected wave and an elevation of central peak systolic blood pressure and pulse pressure.17 In this study, we demonstrated a relationship between trunk flexibility and central blood pressure in the elderly population. The present study also showed that the correlation between flexibility and central blood pressure was significant after adjusting for age and sex. However, the significant correlation disappeared after adjusting for cfPWV as an index of arterial stiffness, implying that arterial stiffness is an important mediator of the relationship between flexibility and central blood pressure. These results suggest that poor flexibility-related arterial stiffening may induce increase in central blood pressure in the elderly.
Flexibility fitness and habitual stretching have beneficial effects on central arterial stiffening. Yamamoto et al. showed that among the elderly, central aortic stiffness was lower in individuals with high flexibility than in those with poor flexibility.12 Cortez-Cooper et al. demonstrated that a 12-week stretching program intervention decreased carotid pulse pressure and arterial stiffness in middle-aged and older adults.18 The American College of Sports Medicine and American Heart Association recommend cardiorespiratory, muscular, and flexibility activity in healthy adults.19 Flexibility exercise is conducted mainly to maintain the range of motion of the joint, postural stability and balance ability.20 To the best of our knowledge, the effect of flexibility on central aortic blood pressure has not been determined. The present study is the first to show the relationship between trunk flexibility and central blood pressure in the elderly, albeit in cross-sectional design. The results of the present study provide new evidence concerning the interaction between flexibility and cardiovascular health. However, in order to clarify cause-and-effect relationship, it is necessary to investigate the effect of a longitudinal stretching intervention on central blood pressure.
In this study, we did not observe any relationship between flexibility and central blood pressure in middle-aged subjects. It is well known that central blood pressure and arterial stiffness increase with advancing age.7 Indeed, central blood pressure and cfPWV in the elderly were higher than those in the middle-aged subjects in this study. Moreover, the increase in arterial stiffness begins to accelerate around and over the age of 60s.7,21 Thus, it is possible that body flexibility may affect the elevated central blood pressure with age-related arterial stiffness.
With regard to the precise mechanism underlying the correlation between trunk flexibility and central blood pressure, there are several possibilities. First, it is thought that cross-links of collagen and elastin in the connective tissue determine tensile strength and elasticity of vascular wall and tendon or ligaments, which are related to both stiffness of arterial wall and flexibility of joint.22,23 Thus, the alternation of connective tissue by aging may be similar in the central artery and the trunk joint.24 Second, flexibility may affect the sympathetic nerve activity and endothelial function. The autonomic nervous system regulates vascular tone and cardiovascular function. Sympathetic nerve activity induces vasoconstriction, blood pressure elevation and arterial stiffness. Furthermore, nitric oxide (NO), which is produced in the vascular endothelium, regulates vascular tone. In normal resting condition, NO is continually released from endothelium and relaxes smooth muscle cells, thereby maintaining vascular distensibility.25 Recently, it was demonstrated that yoga (mainly stretching exercises) reduces sympathetic nerve activity and increases serum NO bioavailability in healthy older adults.26 Therefore, the age-related increase in central blood pressure may be counterbalanced by flexibility due to sympathetic nerve activity and/or endothelial function. However, further studies are required to verify these possibilities.
It is likely that physical activity is correlated to arterial stiffness and flexibility fitness.27 In this study, there were no differences in physical activity and step counts among the groups. Furthermore, after adjusting for physical activity or step counts, sit-and-reach was significantly correlated with central systolic blood pressure and pulse pressure (P < 0.05). Therefore, physical activity may not affect a link between central blood pressure and flexibility fitness in older population.
Central artery pressure waveforms can be subdivided into a forward traveling wave and latter-arriving backward reflected wave. Increased magnitude and shortened timing of wave reflection results in an increase pressure augmentation in systole. The augmentation pressure is influenced by age, gender, height, and arterial stiffness. In contrast to this conventional concept, recent studies have showed that central pressure waveform morphology was determined mainly by the arterial reservoir pressure which is associated with the volume of blood stored in the proximal aorta (e.g., the ascending aorta and aortic arch).28 The aortic reservoir pressure related stronger to augmentation pressure, augmentation index, and left ventricular mass index and contributed to consist of the central blood pressure waveform than wave reflection and arterial stiffness component.29 cfPWV likely reflects velocity of propagation along the descending aorta, then does not cover the ascending aorta and aortic notch. These studies suggest that cfPWV may not be the sole contributor to elevation in central systolic pressure and pulse pressure. To clarify the physiological mechanism underlying the effect of flexibility fitness on central hemodynamics, further studies are warranted to investigate the component of aortic waveform such as the height of incident wave, amplification and timing reflected wave, and augmentation pressure or reservoir pressure and excess pressure.
In conclusion, we examined the relationship between flexibility and central blood pressure. We demonstrated that poor trunk flexibility is associated with increased central systolic blood pressure in the elderly. Our findings suggest that higher flexibility attenuate the age-related increase in central blood pressure.
Conflict of interests
The authors declare that they have no conflict of interest regarding this paper.
Acknowledgments
The study was supported by Grants-in-Aid for Scientific Research (
References
Cite this article
TY - JOUR AU - Miho Komatsu AU - Nobuhiko Akazawa AU - Koichiro Tanahashi AU - Hiroshi Kumagai AU - Toru Yoshikawa AU - Keisei Kosaki AU - Asako Zempo-Miyaki AU - Seiji Maeda PY - 2017 DA - 2017/08/08 TI - Central blood pressure is associated with trunk flexibility in older adults JO - Artery Research SP - 91 EP - 96 VL - 19 IS - C SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2017.07.002 DO - 10.1016/j.artres.2017.07.002 ID - Komatsu2017 ER -
