Design and Implementation of in-Home Real-Time Wireless Fever Monitoring in Pediatrics during the COVID-19 Pandemic
- DOI
- 10.2991/jrnal.k.210521.009How to use a DOI?
- Keywords
- Wireless temperature monitoring system; wireless sensor network; data logging; alarming system
- Abstract
Fever is one of the most common concern to be taken care by parents which sometimes force them to bring their children to the hospital emergency for continuous following up especially at night when sleeping. Fever is defined when the rectal temperature reaches over 38.0°C (100.4°F). Temperatures measured from other sites of body are usually less. There is no defined threshold for fever due to variation of body temperatures between different individuals as much as 1°F. Fever itself is not life threatening unless the rectal temperature is persistent over than 41.6°C (107°F). Fever may be due to a serious illness such as COVID-19 and usually is caused by common infections, which are not serious. However, a fever can be caused by other reasons other than infections. Since continuous temperature monitoring is inapplicable at the rectal site, the paper aims at developing a real-time system using wireless sensor network for wireless continuous fever monitoring on the head skin or wrist, which are the most applicable area with suitable compensation for the read temperature correction. The system can record the temperature on the patient’s side who is required to be isolated and transmit the fever status and critical situations to an alarming system on the side of taking-care people. This system will help in in-home care for pediatrics suffering from fever and especially during the COVID-19 Pandemic.
- Copyright
- © 2021 The Author. Published by Atlantis Press B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Fever is one of the most important symptoms of many diseases and especially nowadays during the COVID-19 Pandemic [1]. Fever may be due to a serious illness and usually is caused by common infections, which are not serious. The body temperature increasing is controlled by the part of the brain called the hypothalamus to fight the infection that may reach the fever level. Fever is considered as one of the most common concern to be taken care by parents which sometimes force them to bring their children to the hospital emergency for continuous following up especially at night when sleeping. Fever is defined when the rectal temperature reaches over 38.0°C (100.4°F). Temperatures measured at other sites of body are usually less. There is no defined threshold for fever due to variation of body temperatures among different individuals as much as 1°F. Fever itself is not life threatening unless the rectal temperature is persistent over than 41.6°C (107°F) [2].
In the past, a thermometer constructed of glass and filled with mercury was used for body temperature monitoring. However, the American Academy of Pediatrics suggests not using mercury thermometers and recommended thermometers which are the electronic ones with the digital temperature display. Another type of thermometers is the plastic strip placed on the forehead, which changes color to indicate the temperature, which is the least accurate. Hence, there are many kinds of temperature measurement methods, most of which are inconvenient to infants and children monitoring, because they cannot realize the real-time continuous temperature reading [3].
Therefore, a method for real-time continuous temperature monitoring should be developed for using at home and be safe and convenient [4]. This method will enable a continuous reading of the temperature data by utilizing the wireless technology that the multiple transmitter nodes can enable the person on charge to monitor the temperatures of many patients (infants and children). This paper aims at designation and implementation of a system applying the embedded technology and wireless sensor network technology [5] for wireless real-time continuous fever monitoring on the head skin or wrist which are the most applicable areas taken in consideration with suitable compensation for the temperature. The Wireless Temperature Monitoring System (WTMS) provides 24/7 real-time continuous temperature monitoring on critical patients (infants and children). The continuous monitoring provides the means to detect abnormalities (fever) at an early stage. The wireless technology is needed especially in COVID-19 patients who have to be isolated. Using the wireless will eliminates cabling and this in turn makes the patient comfortable especially when sleeping and during every day practice. WTMS allows for easy field data collection. The temperature data are transmitted from the sensors at the transmitter nodes to a nearby receiver node via wireless connection. The receiver node can be connected to a computer via USB. In addition, the receiver node can work standalone without the PC. A universal receiver node can be utilized as a data logger, which can collect data from any transmitter node. This universal receiver and the attached PC can work to trigger visual and/or audible alarm for preset temperature values for fever detection. Moreover, it can send Short Message Service (SMS) to the smart phone belonging to the person in charge such as parents. In addition, the data can be analyzed later for diagnosis and reported by a dedicated software package.
2. SYSTEM DEVELOPMENT
2.1. Hardware and System Block Diagram
2.1.1. Transmitter node
The WTMS designed as shown in Figure 1 consists of three main parts: transmitter node, receiver node, and optional data access module.
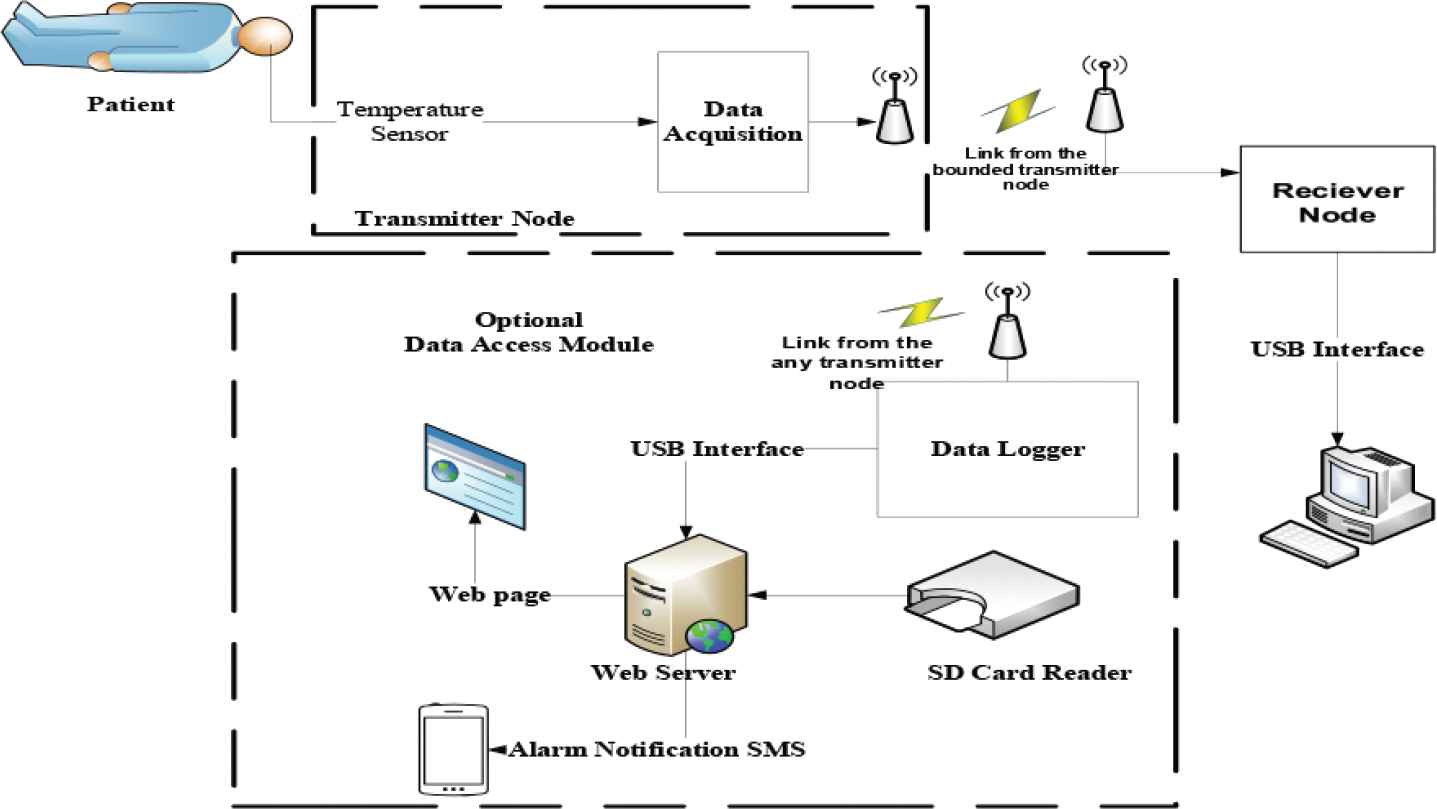
System block diagram.
The system is comprised of Wireless transmitter node, which consists of temperature sensor; lead off detector, microcontroller, power subsystem (battery), and the transmitting antenna as shown in Figure 2. This module is based on wireless Wi-Fi technology. This module is designed to operate in moisture environment and is protected by adding moisture resist material, which will protect and isolate the patient from being connected to the circuit via moisture. The transmitter node has a lead off detector to trigger an alarm on the receiver node when there is no or bad contact on the patient skin. The transmitter is attached to the patient skin all the time by the mean of head bandage or wrist strap, which will give the patient a convenient way of every day practice.
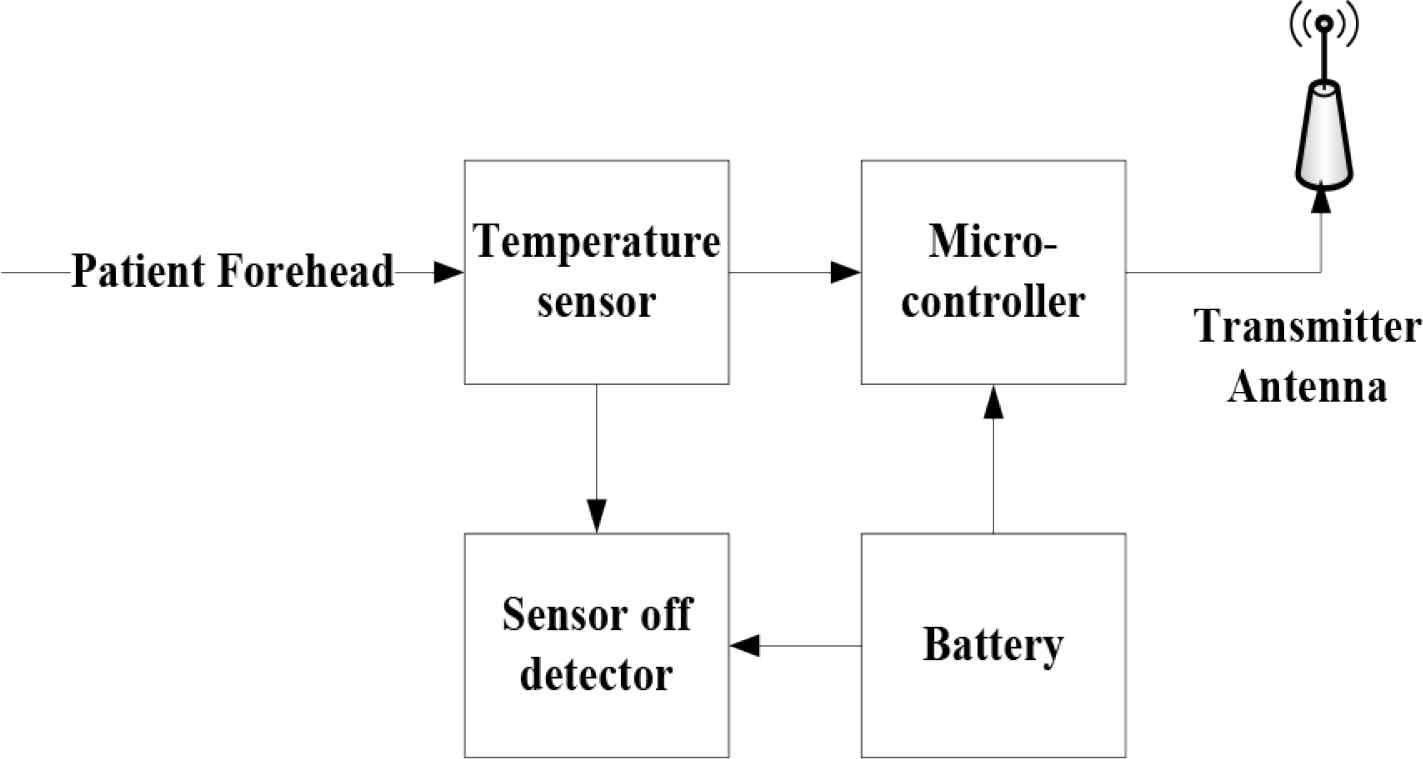
Transmitter node.
2.1.2. Receiver node
It consists of receiving antenna, microcontroller, power subsystem (battery and battery management; recharge circuit operate from USB port). The outputs are liquid crystal display (LCD) as a reading out device for the temperature and alarm values, buzzer for audible alarm, mass storage [I2C EEPROM, and Secure Digital (SD)] card that are controlled by the microcontroller as shown in Figure 3. The controller has a USB interfacing to the PC to collect the data for further analysis. In addition, the receiver node battery could be charged from the PC USB port. This module is based on wireless Wi-Fi technology, which can be directly connected to the PC via USB for data collection and further analysis. Any receiver node can be programmed to collect data from many transmitters, as the case when there are many children or infants to be monitored for temperature rise. The receiver contains SD card to store the data for further analysis by physicians. The collected data can be sent to physician over the internet under user control when the receiver node is connected to a PC.
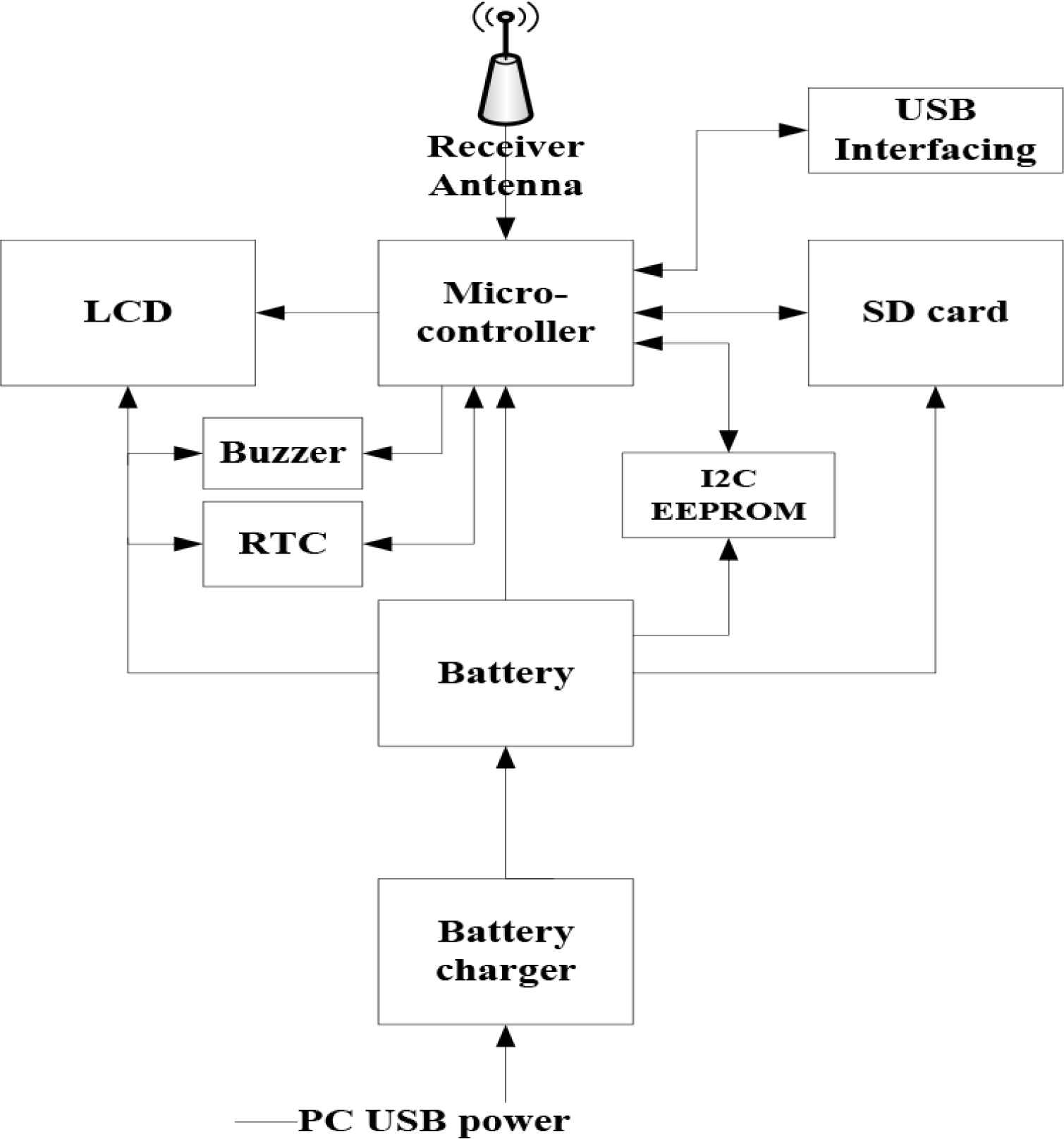
Receiver node.
2.1.3. Data access module
It consists of data logger module which can be connected to a server for data distribution over the web, sending alarm notification SMS to smart phone. SD card reader can be connected to the server for reading SD card from any receiver. The data logger can connect to any transmitter node(s) for data collection and analysis. The data logger is mainly powered from the USB port.
2.2. Software and User Interface
A user interface as shown in Figure 4 is developed using Laboratory Virtual Instrument Engineering Workbench (LabVIEW) [6]. LabVIEW is used to control the wireless module and collect the temperature data of patient events of high temperature threshold of fever.
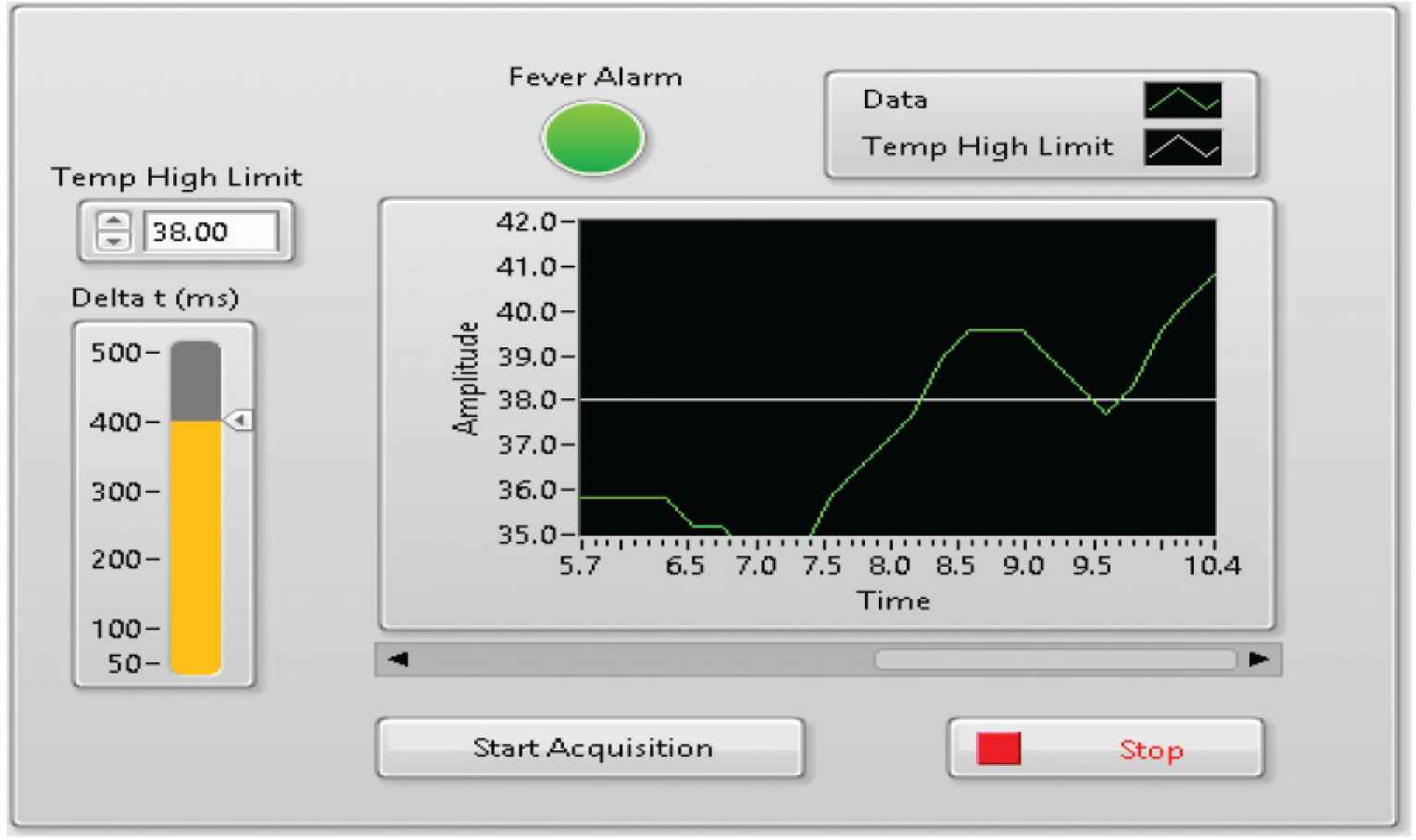
User interface of temperature data collection and fever alarms events.
3. RESULTS AND DISCUSSION
3.1. Analysis of Body Temperature Measurements Comparison Test
Testing the sensor DS18B20 as body temperature sensor is done with comparison to the measurement results with mercury thermometer. The selection of this type of thermometer is due to its accuracy compared to other types of thermometers. Table 1 shows the comparison results, the measurement difference and the average measurement error.
| No. | Time (min) | Temp data (°C) | Temp high limit (°C) | Events of alarms (in RED) |
|---|---|---|---|---|
| 1 | 5.7 | 35.8 | 38 | |
| 2 | 5.9 | 35.8 | 38 | |
| 3 | 6.1 | 35.8 | 38 | |
| 4 | 6.3 | 35.8 | 38 | |
| 5 | 6.5 | 35.2 | 38 | |
| 6 | 6.7 | 35.2 | 38 | |
| 7 | 6.9 | 34.6 | 38 | |
| 8 | 7.1 | 34.6 | 38 | |
| 9 | 8.4 | 38.9 | 38 | FEVER |
| 10 | 8.6 | 39.6 | 38 | FEVER |
| 11 | 8.8 | 39.6 | 38 | FEVER |
| 12 | 9 | 39.6 | 38 | FEVER |
| 13 | 9.2 | 38.9 | 38 | FEVER |
| 14 | 9.4 | 38.3 | 38 | FEVER |
| 15 | 9.6 | 37.7 | 38 |
Body temperature test results
The test results showed the temperature has an average error around 0.64% using the Mercury Thermometer compared to the test results using developed system. Hence, it can be stated that the sensor readings are very good.
3.2. System Analysis and Validation
To analyze, validate the system performance and test its ability to catch events of high temperature threshold, fever test is done. Table 2 shows the test results of continuous acquisition of temperature data in real-time. The acquired temperature data shows the system ability of catching critical events of fever (as shown in RED color), and hence, activating alarming system to prevent deterioration of the patient condition.
| No. | Temperature Sensor (°C) | Mercury thermometer (°C) | Measurement difference (°C) |
|---|---|---|---|
| 1 | 36.75 | 37.60 | 0.85 |
| 2 | 36.63 | 37.25 | 0.62 |
| 3 | 36.25 | 36.97 | 0.72 |
| 4 | 36.35 | 36.94 | 0.59 |
| 5 | 36.56 | 37.25 | 0.69 |
| 6 | 36.06 | 36.70 | 0.64 |
| 7 | 35.95 | 36.49 | 0.54 |
| 8 | 36.85 | 37.28 | 0.43 |
| 9 | 36.75 | 37.57 | 0.82 |
| 10 | 36.70 | 37.53 | 0.83 |
| 11 | 36.50 | 37.30 | 0.80 |
| 12 | 36.53 | 37.16 | 0.63 |
| 13 | 36.54 | 36.96 | 0.42 |
| 14 | 36.26 | 36.71 | 0.45 |
| 15 | 36.23 | 36.75 | 0.52 |
| Average - Error | 0.64% | ||
Events of high temperature threshold of fever test results
3.3. Analysis of Data Transmission Performance Test
The performance test of Nodemcu ESP8266 works to find out if the sensor is accessible by other devices with a certain distance. Testing is done by sending data on Nodemcu ESP8266 to display the results on the website and then test access with a certain range. Distance parameter of the maximal use range is about 50 m. From the tests that have been done, it can be concluded that the website is inaccessible in the range above 50 m. The test results of this communication between the master and the slave modules, the slave module used can accept data successfully from master module according to data delivered.
4. CONCLUSION AND FUTURE WORK
The designed system goal is to provide in home, self-dependent, real-time continuous monitoring for critical events, and alarming system to prevent deterioration of the patient condition such as the COVID-19 Pandemic. The system has many features with wireless (Wi-Fi) connectivity in range of up to 50 m (the distance between the transmitter and receiver nodes), typical signal reception of once every 1–10 min under user control, frequency of data transmission increases with fast temperature rise, temperature range 25–50°C with 0.1°C resolution, preset alarm values, moisture resistant for humid environments.
CONFLICTS OF INTEREST
The author declares no conflicts of interest.
ACKNOWLEDGMENT
I would like to thank the Deanship of Scientific Research of University of Hail, for their support to my research.
AUTHOR INTRODUCTION
Dr. Ali S. Al-Mejrad
 He received the B.Sc. with 1st honor in Electrical Engineering from King Saud University, Kingdom of Saudi Arabia, M.Sc. in Bioengineering from Strathclyde University, UK in 1987 and 1990, respectively; and the PhD in Medical Engineering from University of Edinburgh, UK in 1996. He is currently an Associate Professor of Medical Engineering and Instrumentation in Clinical Laboratory Sciences in the College of Applied Medical Sciences, UoH, KSA. His research interests include Development of Biomedical Instrumentation and Intelligent Systems for Health Care using advanced technologies. He is a member of IEEE and IPEM.
He received the B.Sc. with 1st honor in Electrical Engineering from King Saud University, Kingdom of Saudi Arabia, M.Sc. in Bioengineering from Strathclyde University, UK in 1987 and 1990, respectively; and the PhD in Medical Engineering from University of Edinburgh, UK in 1996. He is currently an Associate Professor of Medical Engineering and Instrumentation in Clinical Laboratory Sciences in the College of Applied Medical Sciences, UoH, KSA. His research interests include Development of Biomedical Instrumentation and Intelligent Systems for Health Care using advanced technologies. He is a member of IEEE and IPEM.
REFERENCES
Cite this article
TY - JOUR AU - Ali S. Al-Mejrad PY - 2021 DA - 2021/05/28 TI - Design and Implementation of in-Home Real-Time Wireless Fever Monitoring in Pediatrics during the COVID-19 Pandemic JO - Journal of Robotics, Networking and Artificial Life SP - 37 EP - 40 VL - 8 IS - 1 SN - 2352-6386 UR - https://doi.org/10.2991/jrnal.k.210521.009 DO - 10.2991/jrnal.k.210521.009 ID - Al-Mejrad2021 ER -
