What Constitutes Health Care Seeking Pathway of TB Patients: A Qualitative Study in Rural Bangladesh
- DOI
- 10.2991/jegh.k.190929.001How to use a DOI?
- Keywords
- Tuberculosis; health care seeking; pathway; Bangladesh
- Abstract
Given the targeted 4–5% annual reduction of tuberculosis (TB) cure cases to reach the “End TB Strategy” by 2020 milestone globally set by WHO, exploration of TB health seeking behavior is warranted for insightful understanding. This qualitative study aims to provide an account of the social, cultural, and socioeconomic breadth of TB cases in Bangladesh. We carried out a total of 32 In-depth Interviews (IDIs) and 16 Key Informant Interviews (KIIs) in both rural and urban areas of Bangladesh. We covered both BRAC [a multinational Non-governmental Organization (NGO)] and non-BRAC (other NGOs) TB program coverage areas to get an insight. We used purposive sampling strategy and initially followed “snowball sampling technique” to identify TB patients. Neuman’s three-phase coding system was adopted to analyze the qualitative data. Underestimation of TB knowledge and lack of awareness among the TB patients along with the opinions from their family members played key roles on their TB health seeking behavior. Quick decision on the treatment issue was observed once the diagnosis was confirmed; however, difficulties were in accepting the diseases. Nevertheless, individual beliefs, intrinsic ideologies, financial abilities, and cultural and social beliefs on TB were closely inter-connected with the “social perception” of TB that eventually influenced the care seeking pathways of TB patients in various ways. Individual and community level public health interventions could increase early diagnosis; therefore, reduce recurrent TB.
- Copyright
- © 2019 Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Tuberculosis (TB) is a major public health problem; it is the ninth leading cause of death globally with 10.4 million new cases detected worldwide in 2016. Nearly 1.3 million of these cases resulted in death [1]. Universal access to quality treatment for all TB patients is necessary to achieve the goal of a TB-free world. To reduce the case fatality rate from 16% to 10% between 2015 and 2020, it is necessary to diagnose and treat patients without any delay [1]. Most TB-burdened countries now provide free treatment facilities through the National Tuberculosis Control Programme (NTP). NTP is normally implemented by the government health services of a country’s national health system. However, many private health care providers and Non-Governmental Organizations (NGOs) also contribute to the NTP delivery system. NTP of Bangladesh first adopted the Directly Observed Treatment Short (DOTS) course strategy in 1993 [2]. The program rapidly expanded in the following years to almost all areas of the country reaching 100% coverage in 2006 [1,2]. For Bangladesh, the program runs on public–private collaboration with strong contribution from NGOs like BRAC along with the Government. BRAC—a multinational NGO, previously known as “Bangladesh Rural Advancement Committee” is the top-ranked NGO in the world for the third year running [3]. Health care seeking behavior of the TB patients has a key role on the success of the program.
According to “The End TB Strategy” in the Sustainable Development Goals, early diagnosis of TB and engagement of public and private health care providers is essential [4]. Since adopting DOTS strategy, impressive case detection and cure rates were recorded [2,5]. However, since 2006 case notification became stagnant and even started to show a declining trend. It is likely that a substantial number of cases are not notified under the NTP and are likely getting treatment from the private sector or not receiving care at all [5,6].
The current TB control strategy is based, among others, on passive case detection, which is influenced by a multitude of health system and patient factors [2]. A patient’s knowledge on TB symptoms, their presence, and severity influence their intention of health care seeking. Similarly, availability and access to anti-TB services, and providers’ behavior also influence care seeking practices and outcomes. Care seeking, therefore, is an important determinant that influences not only the individual’s disease status and its prognosis, but also reflects the epidemiology of TB in a community [7]. A number of studies have been conducted in Bangladesh focusing on health care seeking pathway of TB patients in Bangladesh and they have mostly prioritized the quantitative aspects [2,8,9]. A qualitative exploration can help understand TB patients’ health care seeking patterns for improving the organization of the NTP, which in turn can improve early detection of TB and help patients receive proper treatment without delay. Delay in the diagnosis of these open TB cases often results in transmission of TB among the contacts of the active TB cases and is more likely to fuel its transmission in the community apart from increased morbidity and mortality [10].
The unprecedented success of Bangladesh tackling global health issues is remarkable and highly appreciated. Impressive gains in key human development indicators, educational coverage, poverty alleviation, reduction of maternal and infant mortality, battling several infectious diseases successfully, preparedness for the epidemiological transition of diseases, women empowerment, and technological upgrades make Bangladesh unique and a role model of global development [11]. However, there are still major gaps in our epidemiological knowledge regarding the transmission dynamic of TB despite the fact that TB is endemic and highly prevalent in Bangladesh [12]. With overall progress of the country in all indices past decades, the need analysis with changed environment is crucial to recommend strategy modifications. There are still some knowledge gaps in the DOTS services provided for the urban and rural areas, such as different socioeconomic class and varied educational levels [9]. With alleviation of poverty and a drastic rise in educational indicators, patient and service provider dynamics and expectation levels might have new working dimensions now. DOTS strategy is entirely based on passive case findings that are often greatly influenced by the treatment seeking behavior of the patients suffering from active TB, social stigmatization, and lack of proper access to health services and even diagnostic delays at health facilities [7]. This in turn results in decreased TB case detection with an underestimated number of actual TB cases prevailing in the community. Given the changes in the socioeconomic status (low income to low-middle income), Bangladesh made success in reducing TB [13] and to identify the missing cases as well as retention of TB treatment cases, exploring the health care seeking pathway of TB patients is warranted. Therefore, we carried out a study with the aim to understand the social, cultural, and socioeconomic dimension of TB cases in Bangladesh through qualitative exploration. A recent study was conducted to understand the health care seeking pathway of extrapulmonary TB patients [14]. However, to the best of our knowledge, we have not found any other studies in recent years that studied TB health care seeking behavior context for pulmonary TB patients in Bangladesh.
2. MATERIALS AND METHODS
2.1. Study Design, Participant Selection and Study Site
Qualitative investigation was carried out to explore the TB care seeking pathways in Bangladesh in both rural and urban areas. TB patients from four different subdistricts—Nandail upazila from Mymensingh and Dumuria upazila from Khulna representing the rural areas and Rajshahi City Corporation and Sylhet City Corporation representing the urban areas were selected. These four different geographical areas were selected on the basis of good and bad performance of the health workforce (as per TB program’s expectation) of the existing TB care program implemented by BRAC and non-BRAC NGO TB programs to understand the notion of TB care seeking pathway. In addition, it would lead us to understand the individual TB combating trajectory, i.e., time taken from the onset of symptoms to treatment at DOTS centers, delay in identifying patient, diagnosis, and treatment, socioeconomic and cultural factors were reconnoitered. As the operational arrangement may vary across different habitat and/or under different management, we selected two urban and two rural subdistricts—one from each habitat from BRAC and non-BRAC operational areas. The researchers had several discussions with both BRAC and non-BRAC TB program managers during the planning phase and got impression on good and bad performance of the health workforce. Study site was selected based on that.
The study interviewed TB patients from Bangladesh NTP areas operated by both BRAC and other NGOs. We covered both BRAC (a multinational NGO) and non-BRAC TB program (other NGOs) coverage areas to get an insight. BRAC TB control program was implemented in 42 districts and other non-BRAC TB program was carried out 22 districts out of 64 districts under eight administrative divisions in Bangladesh. Two categories of participants were selected. One representing the patients and other representing the health service providers—either from formal or from informal setting. For the first category, current TB patients and their caregivers/influential household members (who essentially influence the care seeking pathways) were selected. Of the second category, TB care providers [field managers (BRAC terms them as program organizers), community health workers (BRAC terms as shastho sebika)], local pharmacy owners/seller, and assigned DOTS providers who might be either local elite or even neighbors of the patient were interviewed (Figure 1). As these health service providers (both formal and informal) are involved directly with the TB patients in either rural or urban setup, this enables the study to capture the contextual disparities between urban and rural areas. Purposive sampling strategy was used to identify the potential participants. We followed “snowball sampling technique” starting from the TB service provider to identify the suitable participants. A total of 32 In-depth Interviews (IDIs; urban 16 and rural 16) and 16 Key Informant Interviews (KIIs; urban 8 and rural 8) were conducted with TB patients and their caregivers from four subdistricts covered in both BRAC- and non-BRAC-operated areas. Table 1 summarizes the details of participants and tools used.
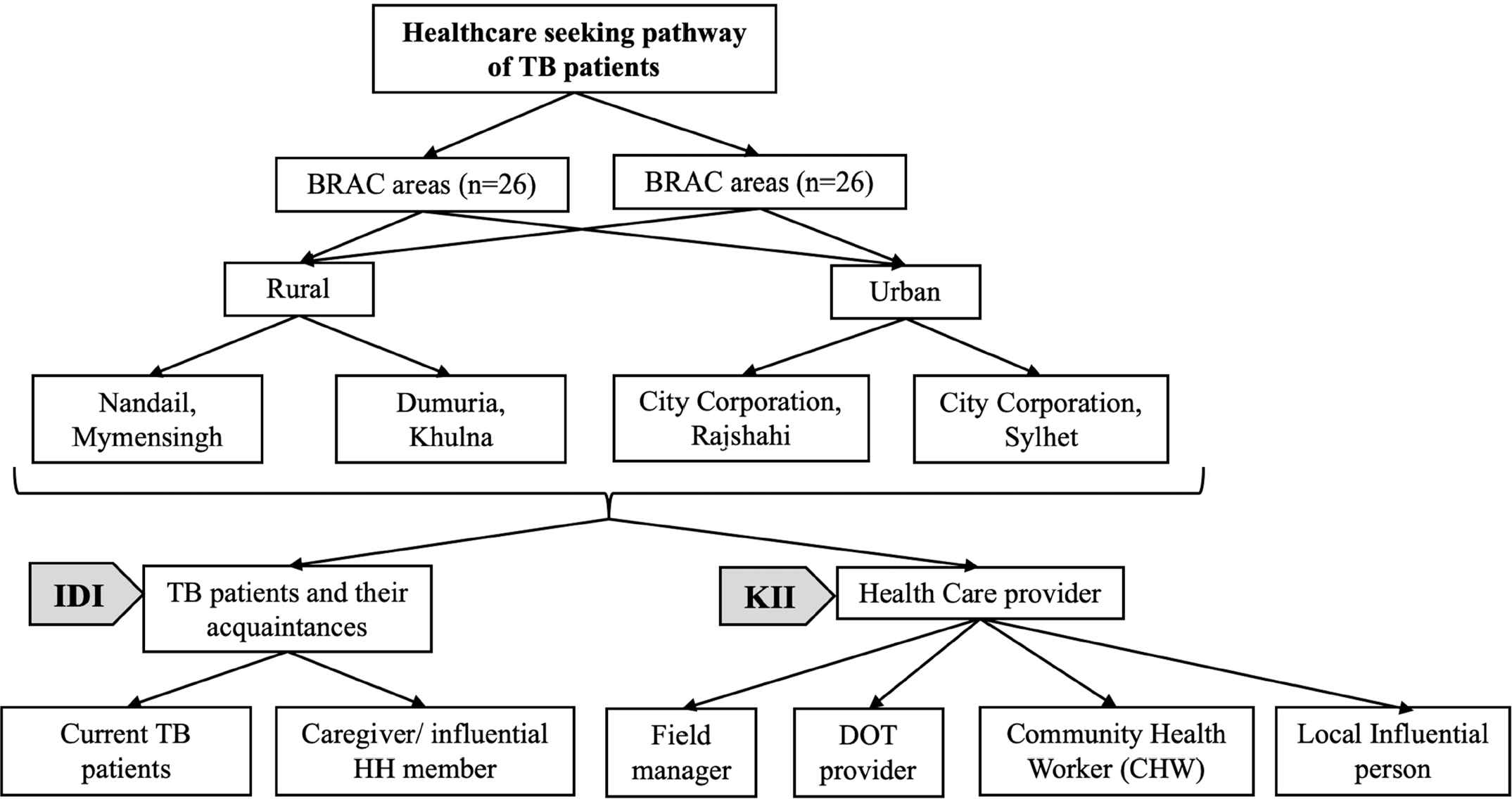
Study flowchart. The flowchart illustrates sampling stages covering both urban and rural areas and different study tools used for each category of participants. IDI, In-depth interview; KII, key informant interview.
| Habitat | BRAC areas (N = 26) | Non-BRAC areas (N = 26) | ||
|---|---|---|---|---|
| IDI (Patients and Caregivers) | KIIs | IDI (Patients and Caregivers) | KIIs | |
| Urban | 8 | 4 | 8 | 4 |
| Rural | 8 | 4 | 8 | 4 |
| Total | 16 | 8 | 16 | 8 |
IDI, in-depth interview; KII, key informant interview.
Summary of the study participants interviewed by habitat
2.2. Data Collection Tools and Techniques
In-depth interview and key informant interview qualitative tools for data collection based on the WHO guideline [15] were used. As per the guideline, we followed eight key steps in conducting IDI that included starting from planning, selecting respondents, preparing interview guidelines, selecting, training, and conducting research assistants, and analyze and report data [16]. TB patients for IDI were selected and contacted from local TB register dataset. Those who agreed to share their experience were finally interviewed and data were recorded. During the selection process, we considered as much variation as we can get in terms of age, gender, education, location, and socioeconomic status of the TB patients. Variation included equal number of TB patients and caregivers for both urban and rural setup in both BRAC and non-BRAC areas. Of that, we covered both good performance and bad performance TB control programs. We ensured gender quality (equal number of male and female) during the selection process. Regarding age, we set our selection criteria of pulmonary TB patients as age 15 years or above with either smear-positive or -negative result. It was important to keep variations among the respondents as one respondent could be different from another in terms of different characteristics. Finally, four current TB patients were purposively selected for IDI from each upazila/ward/municipality level. IDIs were also conducted with a potential household member from every TB patient’s family. All IDIs were envisioned to bring to light the “individual TB-combating trajectory” of the TB patients. KIIs were conducted with the members of health care provider pool who were associated with TB health care service at local level. This target group varied according to the existing operational arrangement of the TB control program at the grassroots level. Shastho Sebika (SS), program organizer (PO), doctors, community volunteers, and village doctors were included as the key informants. Their dealings with TB patients on daily basis and working as TB care as well as general health care provider at the community level for a long time provided strong rationale for selecting them. Simultaneously qualitative research teams were also engaged in conducting informal discussions with local people at every study site. Figure 1 illustrates the sampling stages across different tools. Number of respondents were set until data saturation occurred.
Both IDIs and KIIs were conducted by trained and experienced research teams. A 5-day training was organized before data collection to orient the research assistants with the qualitative checklist and to set a standard for data collection. We used open-ended questions with unrestricted response with limited probing. Interview settings (either open or private) were set as preferred by the respondents. Each interview took around 45–60 min. All interviews were recorded using electronic recorders along with rigorous note-taking by another research assistant after we received verbal consent from each participant. A summary note was prepared by the research assistants each day after the data collection. Data were transcribed by an expert anthropologist who understood the local dialect of the study areas. Field test was conducted after training to ensure quality work outcome in the field.
2.3. Data Analysis
We adopted Neuman’s three-phase coding system [17]. First, taped data were transcribed and skimmed by the researchers to attain a certain level of data familiarization—to have an idea of the content of the data and identify themes. Second, priori codes, inductive codes, and subcodes were formed to define in a broader group. This included code abbreviations, detailed descriptions, color coding, when and which context to use, quotes, and examples. Third, newer version of the data was re-read by each researcher and then the theme was finalized. All transcript data were checked by another qualitative researcher. Data were triangulated for gaining good understanding of the topics from different perspectives. Each researcher attempted to derive a general, abstract theory of process, action, or interaction grounded in view of participants [18]. To understand the TB programs well, the researchers passionately explored the program at micro-level; an event, an activity, a process, or one or more individuals. The case(s) are bound by time and activity. The researchers collected detailed information using a variety of data collection procedures over a sustained period of time [19]. Hence, the study described the TB care pathway under three major contexts: social, cultural, and socioeconomic dimensions at both individual and community level.
3. RESULTS
Equal number of male (n = 24) and female (n = 24) pulmonary TB patients (aged ≥15 years) residing in four different corners (north–south–east–west) of Bangladesh both urban (n = 24) and rural areas (n = 24) covering TB services by both BRAC and non-BRAC organizations were surveyed. The study reported social, cultural, and socioeconomic dimensions at both individual and community level (Figure 2). It was found that knowledge and awareness of patients and their family members played a vital role in TB care seeking pathway. Patients could take a quick decision about their required health care when they were aware of the signs and symptoms of the disease. However, the entire circumstance was not so straightforward as individual belief, ideology, economic ability, and cultural and social consciousness regarding the disease were closely interconnected with the ‘social perception’ of TB that ultimately influenced the care seeking pathways of TB patients in various ways. It emerged from the “TB-combating trajectories” of the patients that individual context (social, cultural, economic, and so on) created different length of pathways.
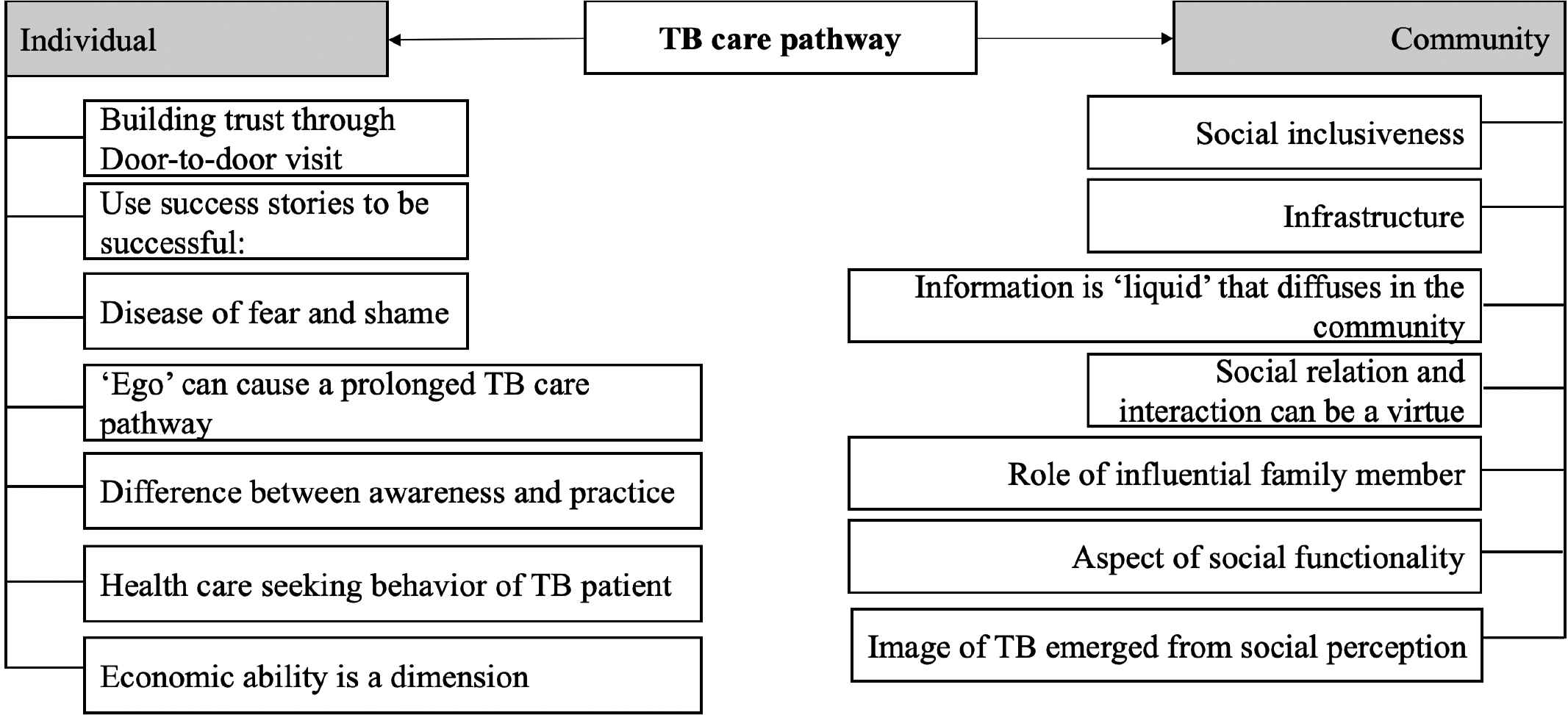
Factors of TB care pathway. Key factors of TB care pathways are stated under three major contexts: social, cultural, and socioeconomic dimensions at both individual and community levels.
3.1. Individual Level
3.1.1. Building trust through door-to-door visit
As TB patients undergo stigma arising from cultural belief, building trust among the patients and their neighborhood is the key to successful TB treatment. Community Health Workers (CHWs) had a remarkable role in capturing more and more patients and gaining their trust. The CHWs create awareness about TB among the community as well as provide support to the TB patients. They further inform the TB patients and their families about the treatment procedure of DOTS and motivate and counsel them to show-up at nearby DOTS center. A meaningful scenario arose from a statement of a frontline worker as she said,
“Usually patients do not want to come under DOT from self-motivation. We visit door to door and motivate them. We arrange a social gathering where they can be informed about TB.”
3.1.2. Using success stories to be successful
In both BRAC and non-BRAC areas cured TB patients played a significant role at community level regarding “TB-combating movement”. They placed their experiences as examples in front of the current and suspected patients so that they could believe that TB is curable through proper treatment. As the cured patients belong to the same community, they were very much influential among community people to develop consciousness regarding the disease. The examples of cured TB patients could help fade the typical terrible image and stigma regarding TB at community level. They also motivated those patients who had chronic cough along with other symptoms of TB to go to the DOTS center for microscopic sputum test. One of the NGO frontline workers and a program in charge stated
“We believe a cured TB patient works like a mobile signboard in the community.”
3.1.3. Disease of fear and shame
Misconception about TB among the community exists in both urban and rural areas. Often patients and their family tried to conceal about the connection with TB, a disease of fear, shame, and probability of “social exclusion”. They had to experience social disregard; it has been observed that there were some common reasons for hiding their illness, sufferings, and their physical difficulties. To some extent, some people were stigmatized for the preconception about the causality of TB, especially in the context of TB care pathway. Indeed, the probability of TB infection was far away from their prediction. In general, they did not want to believe that they could have TB. Thus, they primarily tried to get cured by taking medicines from the source of inherited indigenous family knowledge, local quack, Kabiraj, drugstore keeper, and even from the religious fellows. They had a perception or point of view regarding TB where fear, hesitation, and shame coexisted. It was noticed in some cases that family members of the patients believed TB to be a disease that might spread through contamination and in a few cases in fact it was found that separate utensils were allocated for the patient living under the same roof.
The statement from a TB patient might provide a nuance on the extent of stigma:
“Since I don’t smoke, I have never thought that this thing (TB) can attack. I went to different doctors and drug sellers. After about one year I came to know that I had TB. I scared and fell into a shame. I concealed my diseases from the neighbors because if they know about my bad disease, they will avoid my shop and I will face economic losses.”
3.1.4. ‘Ego’ can cause a prolonged TB care pathway
It emerged from the qualitative data that there existed a sort of behavioral practice where the dilemma of human ego at individual level had come to light. More or less in both BRAC and non-BRAC areas such kind of dilemma had been found. In the grassroots level it could be defined as a conflict of social status that is economic and cultural. The people from an “upper social position” in terms of economic solvency, education level, and social dignity had a psychosocial state of disregard when they were suggested to take medicine from their DOTS providers. Normally SSs came from a “lower social status”. According to the present structure of DOTS of the TB control program, a patient had to depend on his/her DOTS provider and had to go to provider’s place to take medicine every day. In this regard, a field level staff of a subrecipient organization from urban area where they were dependent on BRAC’s SS said,
“There are some affluent and literate patients in the community who aren’t willing to take medicine from a SS. They think SS are not the right person to be a DOT provider. They also think, since these women aren’t educated enough, they haven’t proper knowledge regarding TB. They can’t be trustworthy or dependable in the question of physical distress. They even ignore the suggestion of SSs whenever they are requested to give their sputum for pathological test. Such kind of misunderstanding create sort of delay and make the TB care pathway prolonged.”
Moreover, there was also an undesirable perception about the service of government health facilities among the rich community. In this regard a frontline worker of TB control program said,
“Usually, rich people are reluctant to go to a government hospital for their treatment. They think that the public hospitals are the worse places where doctors and nurses aren’t sincere to their duties. But a suspected TB patient can get a proper treatment in the government hospital because the doctors of government hospitals are properly aware about TB. Many rich patients also think that government provided free treatment of TB might not be good, it is only for poor people and it will be disgraceful for them if they seek a free treatment.”
3.1.5. Health care seeking behavior of TB patient
A typical community health care seeking behavior forms a shape of broad practice that pushes the patients in a certain way of pursuing treatment for their diseases. We found that majority of the patients habitually went to the nearby local drugstores to seek treatment whenever they felt sick. TB patients often made a mistake of treating the symptoms of TB as a regular illness and tended to seek first medical consultation either from a local drugstore keeper or an informal provider—as they would do for other illnesses. Similar scenario was very usual in the TB care trajectories of the patients. It became more palpable when a respondent from Khulna said,
“At first when I suffered from fever and cough, I went to the neighboring drugstore for seeking treatment of my physical distress. I asked for some tablets immediately for fever and cough. The doctor (drug seller) gave some tablets, I came back home and continued those tablets for few days, I felt a little comfort for sometimes, but it could not make me cured... I continued those tablets for about 15–20 days, but my condition remained unchanged. Few days later almost at every night sever cough and fever came back. Then I again went to the same (village) doctor. He changed the medicine and gave me some new medicine again, but my physical condition was unchanged.”
3.1.6. Difference between awareness and practice
Even though some of the patients’ caregivers have sufficient knowledge about TB as they work for TB control program to motivate others, however, we noticed that they are not initially ready to accept the fact that they or their family members could develop TB. Although they have awareness, their practice did not reflect their knowledge. Like others, they seek medicine from the nearby drugstore or village doctor. It became clear when a case of a TB patient whose wife was a CHW for 6 months in BRAC TB control program came to light. She was the caregiver of her husband and described the pathway:
“At first I took him to the local drugstore and got some medicine for usual cough and fever. That medicine was being continued a long period but there was no significant improvement. After about 2 months that means 8 weeks, I suspected that it might be TB. I collected his sputum for pathological test. After sputum test, we went to the government hospital where he was finally identified as a TB patient by a MBBS doctor. Then he came under DOT and I had been playing a role of a DOT provider as well.”
3.1.7. Economic ability is a dimension
Qualitative data showed that sometimes patients did not want to express their physical distress to family members due to the miserable economic condition of the family. Patients thought that if they expressed the sufferings to their family members they may not be able to take the patients to doctor or even buy medicine. Family members might be annoyed. In such poor economic context, patients have hesitations to explain their troubles to the family members. There was a case of a poor woman (mother of two sons) who explained the situation:
“I did not share my troubles with my sons considering their financial condition. They were leading miserable lives with their wives and children. I knew their financial condition very well, they had wives and children, and they could not afford the expenses of my treatment. Moreover, my daughter-in-laws might not take my illness cordially. So, I continued my work although I was suffering from chest pain severely.”
3.2. Community Level
3.2.1. Inclusiveness of all stakeholders
It was interesting to see that both BRAC and non-BRAC organizations arranged meetings with various groups of people in the community. Village doctors, local drugstore owners, and influential groups/persons were given special importance as they could have a role in identifying the suspected patients when the patients come to them seeking treatment. In many cases village doctors/local drugstore owners played the role of DOTS provider too. A BRAC field staff explained the important role of the village doctor/local drugstore owner from her point of view:
“When they (village doctor/pharmacy owner) observe a patient has been suffering from chronic cough for more than three weeks, they advise the patient to go to DOTS center for sputum test. In many cases we provide ‘cough-collection-pots’ to village doctors/pharmacy owners so that they can give the pot to the patients to hold their fasting cough in the morning and can bring it to DOTS center.”
3.2.2. Information is “liquid” that diffuses in the community
In some places people did not know the proper information about the easy accessibility of TB treatment. Sometimes the TB care seeking pathway got prolonged due to inadequate knowledge, awareness, and information about existing TB care services in the community. Describing this issue, a health care provider from BRAC coverage area said:
“The patients who are aware can come more quickly under DOT than those patients who are less aware.”
After repeated misdiagnosis by various health care providers privately, spending money over a year, a patient went to a government hospital to get low-cost treatment. It was his relative who advised him to government health care facilities where the diagnosis turned out correct and he was admitted under the coverage of the local DOTS service. This case showed the lack of awareness among the community and how they suffered due to the lack of information regarding TB treatment. In this regard the caregiver of that patient said:
“We did not know about the DOT service of BRAC and even we did not know about the free and easily reachable treatment of TB. We never even watch carefully the signboard which was held beside the road in front of the BRAC office. We were not introduced with the SS before.”
3.2.3. Social relation and interaction can be a virtue
Patients can have an easy opportunity to be under the DOTS coverage if a TB care provider existed in the social network of a patient. A patient, who was working in brickfield, had been suffering from chronic cough, fever, and chest pain for a long time. Among the labors of the brickfield there was a boy whose mother was a SS of BRAC. Observing the miseries of the patient, the boy suggested him to contact his mother who could help him. Then he communicated with the SS and with the help of the SS he could reach the Sadar Hospital. Finally, in that hospital he was identified as a TB patient through proper diagnosis and taken under DOTS service, and the SS played the role of his DOTS provider.
3.2.4. Role of influential family member/relatives
The role of influential family members came to light through the ‘TB-combating trajectory’ of a patient. We observed that the role of family members/relatives becomes more important when a TB patient gets wrong medicine for using informal health system and their health condition deteriorates. We also noted that there is a presence of trust on government tertiary level hospitals. If anything goes wrong, family members/relatives tend to seek health care at the government tertiary level hospitals. Here a TB patient said:
“…at the end, my son-in-law found a chest specialist and made me bound to go to the doctor where I was identified as a patient of TB.”
3.2.5. Aspect of social functionality
Once diagnosed as pulmonary TB, they entered into a sense of bubble of hesitation and dilemma of social function and they did not act according to the expectation of TB control program. Their pulmonary TB care seeking pathway was also spiral in nature. Behind such kind of health seeking behavior was some socioeconomic and cultural factors. It became obvious through some micronarratives of patient-level experiences. A 40-year-old male patient who was a tailor from an urban area hid his disease from his neighbors because he thought that if people knew about his disease, which was socially stigmatized, customers may not come to his shop and as a result he may face sort of exclusion from both social and financial point of view. A 74-year-old woman from a rural area said:
“I thought my son and my daughter-in-law will not accept me living with them in a same household. For this reason, I liked to hide my illness at the beginning when I was diagnosed as a TB patient. I was alone in the hospital with BRAC’s SS then.”
3.2.6. Image of TB emerged from social perception
We noticed that some patients were stigmatized due to suffering from TB. This social stigma perhaps emerged from historically inherited social perceptions regarding the disease. Socioeconomic and cultural factors that formed the stigmatized social perceptions were correspondingly noticeable in both societal contexts of male and female. According to the typical social belief, ‘there is an empowered state for male’. In such socioeconomic and cultural context, women suffered more than men, which posed them extra burden. However, both male and female patients were fearful of social exclusion due to TB infection. There was a connection among the historical inheritance of social awareness and prejudice regarding TB, individual experience of TB-combating trajectory, and social institutional order (structure) in a social mechanism. Such interconnectedness shaped an image of TB that manifested a typical sense of fear, hesitation, and shame.
4. DISCUSSION
In regard to TB, there is a stigmatized “social perception” that can be understood through a conceptual framework of sociological imagination. The concept of sociological imagination is that stress is able to connect individual experiences and social relationships. Charles Wright Mills defined sociological imagination, “the intense awareness of the relationship between individual experience and the wider society” [20]. Seemingly impersonal and remote historical forces may be linked to incidents taking place in an individual’s life. This implies that people may look at their own personal problems as social issues and connect their own individual experiences with the workings of society. The “sociological imagination” enables people to distinguish between personal troubles and public issues.
“Social perception” comes from “social imagination” that creates “social image” of a social phenomenon. Here, qualitative researchers wanted to understand the social aspect of the existing TB care pathway in the community through a conceptual framework, “sociological imagination.” Through the concept “sociological imagination” Charles Wright Mills, an American sociologist sketched an image of mindset or cognitive affection of the researchers using the concept of “sociological imagination”. It is such kind of effort where researchers have to go through a journey; they try to connect two types of social phenomena, individual experiences and social relationship all the way through an empathetic psycho-social journey [20]. Other aspect is that social capital influences health positively, social capital reduces the odds of adverse treatment outcomes by 63.1%. Authors suggest that proper interventions for building social capital for TB patients and linking them with the program would improve program performance [21]. Social relation and interaction have an advantage that can be a role player in the TB care pathway. Sometimes social relation and interaction can help find out a way of seeking treatment for TB. It can show the right and shorter pathway according to the context of existing TB control service. It is also a matter of diffusion of information.
“Micronarratives” regarding the “social image” of TB is important [20]. Many people are still living with the terrible social image (memories) of earlier death causality of TB. There are also some active socioeconomic and cultural factors. As a result, although TB control program helped reduce social stigma of TB yet it has to go a long way. We can see in Eastern Cape, South Africa where TB is endemic, 95% believe people with TB have a tendency to hide their TB status because they are afraid of social disregard. Furthermore, 90% believe it is mainly the irresponsible patients, who do not take their treatment, are liable for spreading TB, 74% believe that people who get TB through drinking or smoking get what they deserve, and 51% believe that if you have TB people do not respect you [22]. On the gender issue, earlier study reported that women in Bangladesh had significantly longer delay in diagnostic and patient treatment delay in comparison with men [23]. We found that most of the respondents were more or less stigmatized regarding TB. It was even found that even though an individual patient and her/his family was aware of the information about TB, they were not too “proactive” as per the program’s expectation.
Another concept “habitus” from French social scientist Pierre Buordieu became important when we went through the health care seeking behavior of the community. The habitus is socialized norms or trends that guide behaviors and thinking. It influences the identity, actions, and choices of the individual. The habitus structures inherent qualities of mind and character in an individual and is produced by the conditionings associated with a particular class of conditions of existence, this constitutes of systems of durable and transposable personalities [24]. The concept “habitus” is a notion that one is deeply internalized social structure, strongly controlling, and largely inaccessible into consciousness [25]. Social notions of structure reflected through the “habitus” of an individual. It emerged that individual context was a very important factor that played a vital role in deciding whether the TB care seeking pathway will be shorter or not. It might prolong TB care seeking pathway due to a habituated health seeking behavior. Earlier study reported that delays in treatment occur for several reasons, such as lack of knowledge, lack of awareness of the significance of symptoms, negative social attitudes, or different combinations of these three factors [26]. In regard to the cured pulmonary TB patients, we noted that there was also a notion of gratitude; cured TB patients worked for the community people from a point of expressing gratefulness to the organization from where they got a free treatment. They tried to express their gratefulness to the field staffs by contributing in TB control program activities. Health care seeking behavior is the ways in which people interpret health-related symptoms and take action to address these symptoms, including seeking help from a range of alternative sources to prevent, improve, treat, or cope with the symptoms [27].
Besides other factors, training for the drugstore keepers and village doctors should be considered seriously. As most of the patients come to village doctors/pharmacy owners to seek care, a long-term training program will be useful in providing proper TB care service to the community people. This training program should be followed by proper certification. The social notion about certificate will work as an incentive among them. Pharmacy owners and village doctors can be more interested and motivated for that cultural capital (certificate). TB communication-related activities should be enhanced at the community level. There was also a dilemma among researchers that they could not leave the previous knowledge regarding programmatic activities. However, when researchers considered the context of an individual, they felt a necessity for intensive door-to-door awareness activity. Because social individuals now exist in a rat race, they are more considerate on functioning of the body rather than taking care of it.
5. CONCLUSION
Knowledge and awareness of TB patients and their family members play a major role in TB care seeking pathway. In addition, individual belief and ideology, economic ability, and cultural and social consciousness influence the care seeking pathways of TB patients in Bangladesh. Public health TB program should focus on both individual and community aspects of TB burden to increase early diagnosis and thereby reduce TB.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHOR CONTRIBUTIONS
T.S., N.K., A.S.C., A.I. and M.R. conceptualized the study. T.S., N.K. and A.S.C. analyzed the data. T.S., N.K. and F.M.Y. wrote the first draft and finalized the manuscript. A.S.C., A.I. and M.R. edited and reviewed the manuscript.
FUNDING
The study was funded as part of a larger project at BRAC Tuberculosis program supported by the Global Fund to Fight AIDS, Tuberculosis, and Malaria. There was no specific funding for this study. The funding body had no influence on study design, analysis, and manuscript writing.
ACKNOWLEDGMENTS
We would like to share our sincere thanks to the BRAC TB program and BRAC Research and Evaluation (RED) colleagues for their kind support. We would like to share our sincere thanks to all the respondents—patients, caregivers, frontline program staffs, and also the field research team who worked hard during fieldwork.
ETHICAL APPROVAL
The study was ethically approved by the ethical committee of Research and Evaluation Division (RED) of BRAC. The committee approved the verbal consent from participants; however, detailed risks and benefits of the participating in the study were explicitly described to each participant.
CONSENT FOR PUBLICATION
All authors approved the manuscript and consented for journal submission.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Tanvir Shatil AU - Nusrat Khan AU - Fakir Md. Yunus AU - Anita Sharif Chowdhury AU - Saifur Reza AU - Shayla Islam AU - Akramul Islam AU - Mahfuzar Rahman PY - 2019 DA - 2019/10/14 TI - What Constitutes Health Care Seeking Pathway of TB Patients: A Qualitative Study in Rural Bangladesh JO - Journal of Epidemiology and Global Health SP - 300 EP - 308 VL - 9 IS - 4 SN - 2210-6014 UR - https://doi.org/10.2991/jegh.k.190929.001 DO - 10.2991/jegh.k.190929.001 ID - Shatil2019 ER -
