A cross-sectional study of pediatric eye care perceptions in Ghana, Honduras, and India
Present address: School of Medicine, New York Medical College, Valhalla, NY 10595, USA.
- DOI
- 10.1016/j.jegh.2014.06.004How to use a DOI?
- Keywords
- Pediatric eye health; Perceptions; Misconceptions; Barriers; Vision 2020
- Abstract
Of the more than 1.4 million blind children worldwide, 75% live in developing countries. To reduce the prevalence of childhood blindness and associated diseases, attention is given to understanding the perceptions and level of awareness held by caregivers. This understanding can enable tailored health programs to reduce the global prevalence of blindness with increased efficiency. This study, which took place in Ghana, Honduras, and India, found that 95% of caregivers believed in the importance of eye exams for children, yet 66% of caregivers said that none of their children had ever received an eye exam. Participants’ major reasons for not bringing their children included the belief that their child had no eye problems along with similar and unique socio-economic barriers. Further information was gained through the use of a five-question test on basic child eye care symptoms, which showed that out of the three country locations, the studied population in India had the least understanding about pediatric eye symptoms. Further analysis revealed significant gaps in understanding of general eye health while detected knowledge barriers provide evidence that fundamental misconceptions appear to be inhibiting caregivers’ competence in facilitating their children’s eye health.
- Copyright
- © 2014 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
1. Introduction
According to the World Health Organization (WHO), childhood blindness refers to diseases or conditions occurring in childhood or early adolescence, which, if left untreated, may result in severe visual impairment that is likely to be untreatable later in life [1]. The WHO estimates that 19 million children worldwide are currently visually impaired, of which 1.5 million are fully blind [2]. Furthermore, it is estimated that roughly 500,000 additional cases of childhood blindness occur each year, with a higher prevalence of these cases in lower-income populations [3]. Visual impairment is known to have a significant bearing on the health, social and future economic wellbeing of children around the world [4].
While the number of cases of blindness in children is lower than the rate among adults, the effects are still severe. As an economic drain on the family, community and nation, pediatric blindness is estimated to have a global annual cost of nearly 1 trillion US dollars [5–7]. Adding to the social and economic challenge, children who live with a significant visual impairment are less likely to attend and complete an education, find work, achieve financial independence, or establish an independent household. Pediatric visual impairment and blindness has also been linked to child mortality. Up to 60% of children die within a year of becoming blind from systemic complications or from a lack of coordinated care provided by their impoverished families [5,7]. The etiological factors linking child mortality and vision loss also include premature birth, measles, congenital rubella syndrome, and vitamin A deficiency [8]. Thus, eye care and pediatric health are inextricably bound, making it crucial that visual problems be treated as early as possible.
Vision 2020: The Right to Sight Initiative developed by the International Agency for Prevention of Blindness (IAPB) and WHO aims to reduce pediatric visual impairment and blindness internationally. It is estimated that 1 million blind children live in Asia, 0.3 million in Africa, 0.1 million in Latin America, and 0.1 million in the rest of the world [5]. As developing countries constitute 75% of childhood blindness, Vision 2020 is focused on improving disease control, human resource development, and health-care infrastructure in the developing world [2,10]. India, the world’s second largest country by population, is home to 21% of the world’s blind and 23% of the visually impaired [9,11]. India has approximately 270,000 blind children; while no valid estimates exist for Ghana, Sub-Saharan Africa has approximately 320,000 blind children [12,13]. Similarly, with no valid estimates for the number of blind or visually impaired children in Honduras, Latin America has an estimated 100,000 blind children [13].
Several factors contribute to high rates of untreated pediatric blindness and visual impairment in Africa, Asia and Latin America. A shortage of pediatric ophthalmologists and ophthalmology centers as well as significant misunderstandings about pediatric eye issues and treatment options in rural communities have been identified in India and Ghana [14,15]. While pediatric eye care has not been well studied within Honduras, cursory pilot studies indicate that Honduran families may also be experiencing misconceptions about adult eye health and treatment options [16,17]. These misconceptions, along with unique local barriers, may be preventing families from seeking proper treatment.
Since 2000, India’s National Population Policy has prioritized developing local primary healthcare services to provide basic care [18]. This is in accordance with the WHO which has prioritized combating childhood blindness by listing primary healthcare as the most important factor for early identification of eye disease symptoms [10]. However, Indians tend to bypass local sub-centers or primary health centers for specialized hospitals [19]. As a result, many Indian families are not seeking or receiving essential preventative ophthalmologic care. Similarly, a recent study in Ghana reported that rural patients did not value preventive ophthalmologic care [15]. In both countries, routine eye exams are overlooked and treatment for eye health is typically under-utilized. In Honduras, where affordability is a significant issue, families are not pursuing treatment for serious eye ailments let alone preventative care [20].
Parents and caregivers in Ghana, Honduras and India may have significant misconceptions about the causes and treatment methods for pediatric visual impairment. Without proper education of signs and symptoms of common pediatric eye ailments, parents may not recognize an eye problem in a timely manner [21]. However, by developing comprehension of basic symptoms, treatment options, and importance of timely care for pediatric eye conditions, Ghanaian, Honduran, and Indian communities could improve the overall quality of pediatric health while reducing the number of visually impaired children.
To combat pediatric visual impairment and blindness, it is essential to understand the perceptions held by caregivers. Currently, there is very limited information available about parents’ and caregivers’ understanding of pediatric eye care. This cross-sectional analysis examines barriers and misconceptions of eye care in rural and under-privileged Ghanaian, Honduran, and Indian communities that prevent caregivers from seeking routine examinations, early diagnosis, treatment, and other eye care services for their children.
2. Methods
2.1. Ghana
In the 61-day period of June and July 2011, daily outreaches were carried out by Ghanaian eye clinics. These clinics are located in the Accra and Kumasi region of Ghana and treat patients living in villages up to 250 km away. Patients (including children) received eye care services from optometric nurses and doctors from Save The Nation’s Sight Eye Clinic, Charity Eye Centre, Northwestern Eye Centre, and Crystal Eye Clinic through these outreach programs. All adults who received eye services from these outreach clinics were asked whether they would be willing to participate in a research study. Ultimately, exactly 200 participants enrolled, and 3 original enrollees declined to participate citing time as their main concern.
2.2. Honduras
A similar study was carried out in Honduras during a six-week period between June and July 2012. The Honduran clinic Centro de Salud Integral ZOE organizes weekly outreach trips and also sees many patients at its main facility. Outreaches allow the ZOE Eye Clinic to reach individuals in predominantly rural areas up to 130 km away who face a significant deficiency in eye care services. All adults who came to the outreach clinic were screened for the study by asking whether they would be willing to participate. At the ZOE Eye Clinic, a random procedure was followed to survey a pool of consenting participants. In total, 60 outreach patients and 100 clinic patients were surveyed.
2.3. India
During a two-month period from July to August 2012, daily outreaches were planned and operated by the Kalinga Eye Hospital & Research Centre (KEHRC), located in Dhenkanal, Orissa, India. KEHRC treats patients living in villages up to 100 km away. All adult participants who attended outreach clinics and received eye care services were asked whether they would be willing to participate in the research study in which 154 adults were surveyed.
2.4. Survey protocol and statistical analysis
A total of 514 participants – 80% female and 20% male – from Ghana, Honduras and India were interviewed. This study did not involve any minors under the age of 18. Participants were asked survey questions relating to demographic information, country-specific poverty scorecards designed by Microfinance Risk Management [22–24], family history relating to eye health, and questions assessing eye care perceptions, knowledge, and misconceptions. The questions relating to eye care knowledge asked participants whether they believed that any of the following five outcomes in children could indicate an eye problem: squinting, itching of eyes, frequent headaches, difficulty in school, and ear pain (which are all clinically related to eye problems, except for ear pain). These five questions were chosen because they involve easily noticeable conditions in both rural and urban Ghanaian, Honduran and Indian communities, according to the local clinics mentioned above. Hypothetically, caregivers who can sufficiently suspect that a child has an eye problem should answer the majority of these questions correctly. Additionally, bivariate cross-comparisons of the responses to pairs of questions can be used to check for particular discrepancies in the response of caregivers to eye health care. Statistical analysis was performed using JMP, and R-Professional statistical software tools. To overcome language barriers, local community member volunteer or clinic staff with each eye clinic served as a translator, except in Honduras where the investigator conducted interviews in Spanish.
3. Results
3.1. Pediatric eye care
Participants were asked whether their child (or children) ever had an eye exam in the past. Of the total 514 participants from Ghana, Honduras and India, 67% reported their children not having an eye examination. A country-specific analysis of the sample shows that in India 66.9% of children never had an eye exam, while 61.2% of Honduran and 36.7% of Ghanaian children never underwent an eye exam by an ophthalmic professional. Interestingly, when participants were asked whether they believed an eye exam was beneficial to their child’s eye health, 95% of total participants acknowledged that eye exams were beneficial for the health of their children’s eyes. When asked whether their children had any existing eye problems, 40% of the total sample who responded to this question (172 of 425) reported that their children had visual problems. As per individual country, 44% of Ghanaian, 49% of Honduran, and 24% of Indian caregivers reported some form of pediatric visual abnormality.
3.2. Self-reported barriers hindering the uptake of eye exams for children
To assess the effect that poverty may have on the opportunity of a caregiver to coordinate an eye examination for their child, logarithmic odds plots were diagramed based on results from the poverty scorecard surveys. Fig. 1A demonstrates that when all countries were taken together, poverty does significantly inhibit the chances of acquiring an eye exam for a child in those developing countries (p = 0.0095, primary coefficient t-test for significance). However, when each country was isolated and individually plotted, Fig. 1C and D for India and Ghana respectively showed no prominent influence as a result of poverty levels for those two countries (p = 0.42 and p = 0.14 respectively, t-tests of significance for primary coefficients). It was observed that poverty did have the greatest effect on Hondurans (p = 0.0786). Furthermore, to ascertain any barriers preventing caregivers from acquiring an eye exam for their child, participants were asked to describe why they were not able to bring their children to the outreach clinic or attend a local community clinic to get their children’s eyes examined by a medical professional (Table 1).
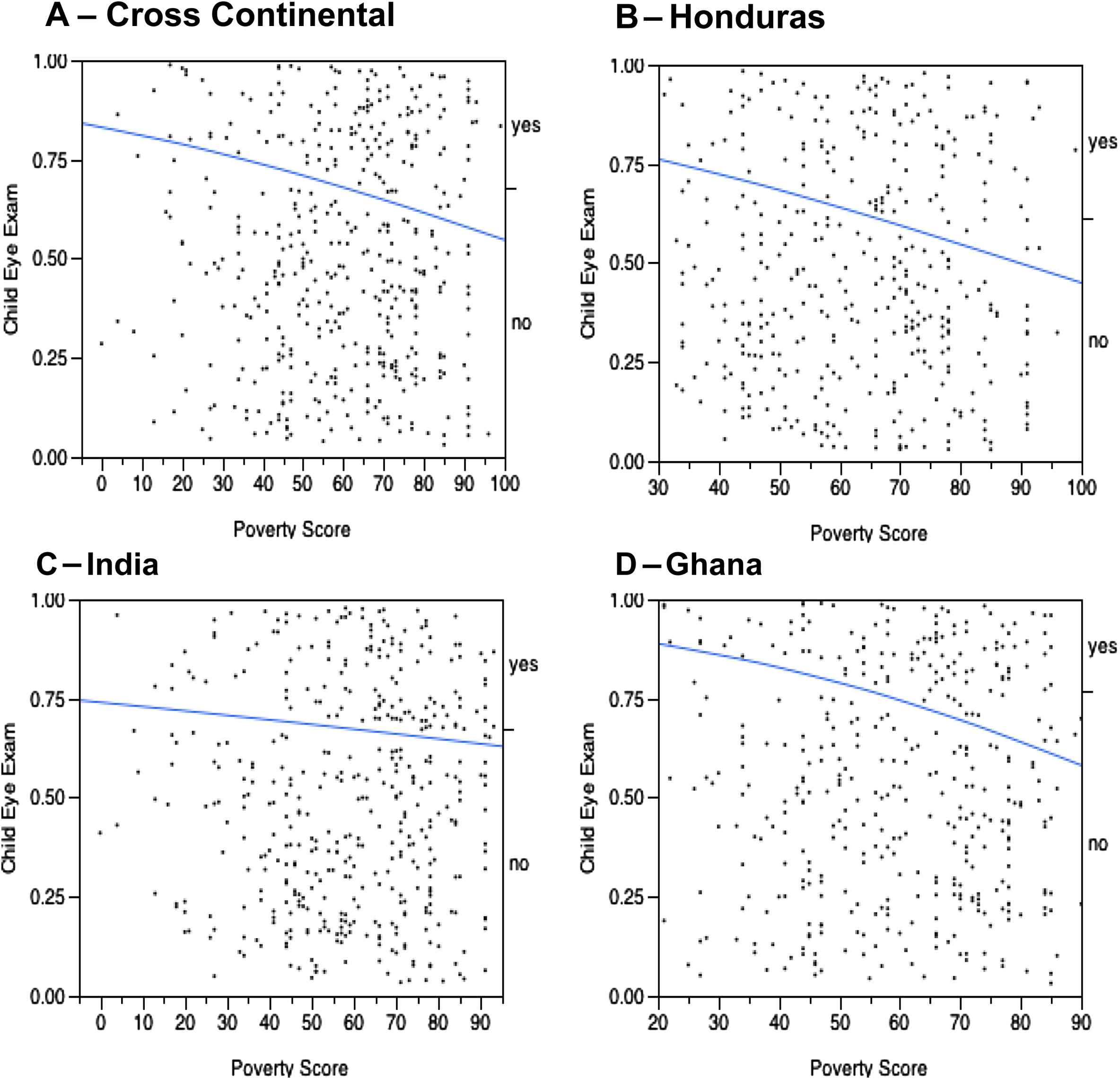
Log odd plots illustrating the effect of poverty on whether a child is more or less likely to have an eye exam. A – Combined poverty values for all three countries, B – log plot for data values obtained in Honduras, C – data values obtained in India, and D – data values obtained in Ghana.
| Patient self reported reasons for not attending an eye clinic | ||
|---|---|---|
| N | % | |
| Ghana | ||
| Children at work or school | 61 | 38.6 |
| Children do not live in household | 49 | 31.0 |
| Children have no eye problems | 29 | 18.4 |
| Child does not belong to me | 8 | 5.1 |
| Thought clinic was for adults | 4 | 2.5 |
| Has no time | 3 | 1.9 |
| Has no money | 3 | 1.9 |
| Forgot to carry child for eye exam | 1 | 0.6 |
| Honduras | ||
| Child has no eye problems | 50 | 49 |
| Has no money | 17 | 16.7 |
| Not necessary/priority | 11 | 10.8 |
| Not my responsibility | 7 | 6.9 |
| Has no time | 4 | 3.9 |
| Child is too young | 3 | 2.9 |
| Treated simple problems myself | 3 | 2.9 |
| No answer | 3 | 2.9 |
| No clinic nearby | 2 | 2.0 |
| Chose to skip question | 2 | 2.0 |
| India | ||
| No reason for getting an eye exam | 104 | 75.4 |
| Child has no eye problems | 15 | 10.9 |
| Caregiver has visual problems | 11 | 7.9 |
| Injury | 3 | 2.1 |
| No money | 1 | 0.7 |
| Spouse | 1 | 0.7 |
| Distance | 1 | 0.7 |
Patient self-reported reasons for not attending a clinic to acquire an eye exam for their child.
This study noted similarities from all three locations in participants’ response to what barriers to eye care they encountered, such as time, cost and distance. Interestingly, of all participants who responded, 50.9% (223/438) said that their child had no eye problems or did not need an eye exam. Furthermore, unique site-specific barriers were identified; 11 adult participants (7.9%) within the Indian cohort responded that their own visual problems prevented them from acquiring eye exams for their own children. This number may be significantly higher as India is home to the largest number of visually impaired and blind adults. In addition, 61 Ghanaian participants (30.7%) reported that their child was either in school or at work and thus was not available to get an eye exam.
3.3. Knowledge of pediatric eye symptoms
All 514 participants responded to whether squinting, itching, headaches, difficulty in school, and ear pain were basic symptoms of visual abnormalities (Table 2). Participants answering all five questions accurately were grouped as being fully capable of detecting pediatric visual symptoms, while others were not (Table 3). This study found that 23% Ghanaians, 43% Hondurans and 8% Indians were fully capable, revealing that only 24.9% of the sample pool possessed sufficient knowledge on child eye care to accurately suspect that a child has an eye problem (Chi Square for independence = 53.4). Bivariate comparisons determined that those whose children had an eye exam in the past were significantly more likely to be fully capable of recognizing eye problems than those whose children did not have an eye exam (17.14% of 140 vs. 10.54% of 294, 2-sample 1-tailed z-test for proportions, p < 0.05). This implies that participants whose children had an eye exam may have acquired knowledge during the physical examination by a healthcare provider. Incidentally, while knowledge on general eye health appeared to be a significant barrier for the communities in all three countries, poverty levels did not show any significant statistical influence on caregivers capacity to recognize pediatric symptoms (log odds p = 0.0026).
| Ghana (%) | Honduras (%) | India (%) | X2 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Correct | Incorrect | N/A | Correct | Incorrect | N/A | Correct | Incorrect | N/A | Ratio | |
| Squinting eyes | 86.5 | 5.5 | 8.0 | 78.8 | 21.3 | 0.0 | 34.9 | 56.6 | 8.6 | 153.5 |
| Itching eyes | 94.0 | 3.0 | 3.0 | 88.1 | 11.9 | 0.0 | 69.7 | 27.0 | 3.3 | 54.7 |
| Headaches | 72.5 | 13.5 | 14.0 | 90.0 | 10.0 | 0.0 | 59.5 | 34.6 | 5.9 | 69.6 |
| Difficulty in school | 50.8 | 31.9 | 17.3 | 88.8 | 11.3 | 0.0 | 71.9 | 22.2 | 5.9 | 78.2 |
| Ear pains | 45.0 | 37.0 | 18.0 | 63.8 | 36.3 | 0.0 | 26.8 | 62.1 | 11.1 | 81.4 |
Cross comparison of participants’ response to five questions assessing knowledge on eye disease symptoms: are the following related to eye problems if a child frequently – squints, itches eyes, has headaches, has difficulty in school, and has ear pain? All, excluding ear pain, are clinically related to eye health.
| Participants’ capacity to recognize pediatric eye symptoms | ||||||||
|---|---|---|---|---|---|---|---|---|
| Ghana | Honduras | India | Total | |||||
| N | % | N | % | N | % | N | % | |
| Fully capable | 46.0 | 23.0 | 69.0 | 43.1 | 13.0 | 8.4 | 128.0 | 24.9 |
| Not fully capable | 154.0 | 77.0 | 91.0 | 56.9 | 141.0 | 91.6 | 386.0 | 75.1 |
| Total | 200.0 | 100.0 | 160.0 | 100.0 | 154.0 | 100.0 | 514.0 | 100.0 |
Contingency table of participants’ capacity to recognize pediatric eye problems.
3.4. Current beliefs about pediatric eye health (in India)
Participants from the India cohort were surveyed with additional questions about child eye care symptoms. Those enrolled were asked at what age an individual can require the need for spectacles; 85 (or 55% of those responding) participants stated an age which fell within the range of 40–49 years old (Fig. 2). A 2-sample t-test showed no statistical difference between the average ages stated by men compared with women (at 95% CI). Overall, less than 6% of individuals surveyed thought that children could ever require spectacles. An additional 20% did not know at what age children could possibly require spectacles. Furthermore, respondents were asked whether children could have one or more cataracts in their eyes, and 60% of participants replied that it was not possible for children to have cataracts, while 18.8% responded that they did not know if children could have cataracts (Table 4). For further insight leading to understanding the perceptions of caregivers toward pediatric eye exams, individuals were asked: “How frequently should a child receive an eye exam?” Thirty-two percent of individuals surveyed considered an annual or biannual eye exam beneficial for children while 48.7% of respondents (Table 5) stated “only when a problem arises.”
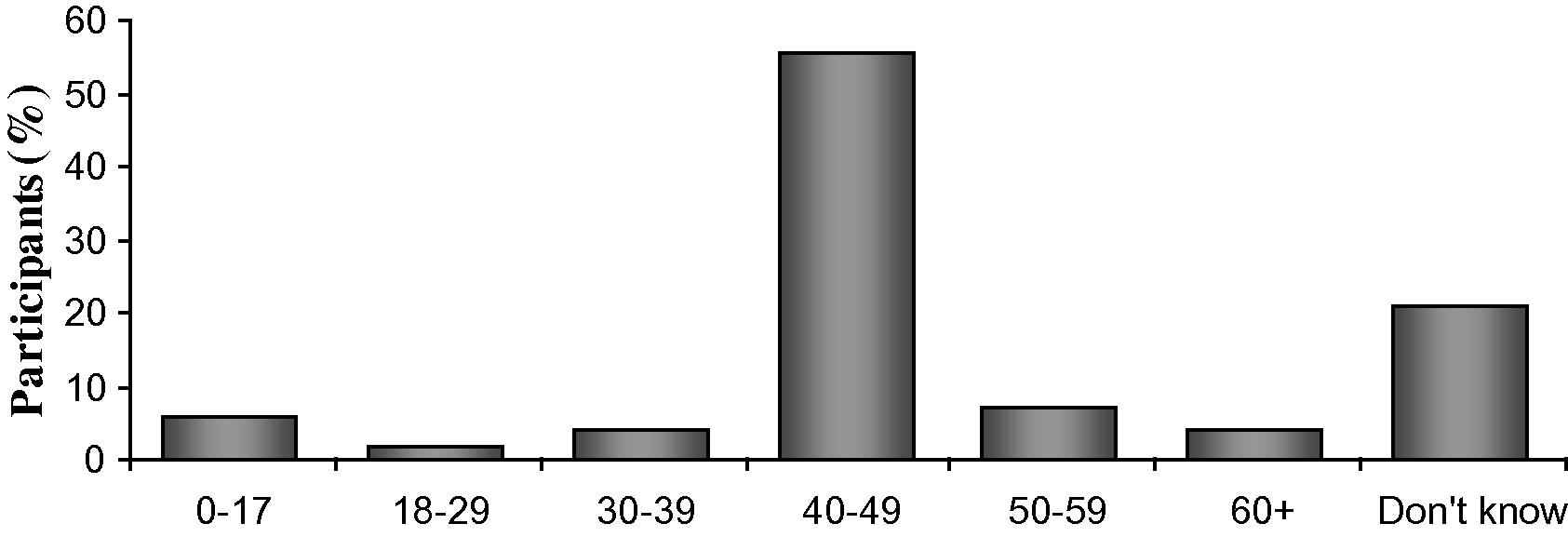
Participant selected age ranges for when an individual could begin requiring the need for spectacles.
| Pediatric cataracts | N | % |
|---|---|---|
| Can have | 33.0 | 21.4 |
| Cannot have | 92.0 | 59.7 |
| Does not know | 29.0 | 18.8 |
| Total | 154.0 | 100.0 |
Participant response to whether children can acquire cataracts in their eyes.
| Frequency of child eye exam | N | % |
|---|---|---|
| When a problem arises | 75 | 48.7 |
| One time a year | 17 | 11.0 |
| Two times a year | 32 | 20.8 |
| Three times a year | 4 | 2.6 |
| Four times a year | 4 | 2.6 |
| Other | 6 | 3.9 |
Participant response to the frequency in which a child should have a routine eye exam.
4. Discussion
This is the first study to examine the perceptions and misconceptions associated with pediatric eye health in communities across three continents (Ghana, Honduras and India). This study demonstrates that the barriers faced by Ghanaian, Honduran and Indian communities have similar trends, as well as unique site-specific impediments. These barriers appeared to be primarily socio-economic. The most significant common barrier was the caregivers’ belief that their children had no eye problems. One third of caregivers considered eye examinations for their children unnecessary due to a perceived lack of eye problems. However, it was observed that only 25% of overall participants were fully capable of detecting eye symptoms. While there is no way to verify that all 33% of participants’ children truly did or did not have visual symptoms, it can be implied that this belief may have contributed to the significant lack of preventative care and lack of eye examinations. Within the study population, 67% of children never previously received an eye examination. If a child does not show physical symptoms of a visual complication, the etiologic and biochemical causative factors may continue to lie hidden, unless examined by a qualified medical professional. If left untreated, the subtle side effects of ophthalmologic issues may progress into more debilitating problems later in life.
Bivariate cross-comparison revealed that the proportion of all 514 participants who answered the pediatric eye health questions correctly did not significantly differ for those who reported that their children previously had an eye exam, compared with those whose children did not have an eye exam. This may suggest that even after receiving an eye examination by an eye specialist, an individual may still not have learned or received sufficient information regarding basic ocular symptoms (97.84% of 139 people vs. 95.10% of 286 people, 2-sample 2-tailed z-test for proportions yields a p-value greater than 0.10).
Child motility was a unique impediment recorded in the Ghanaian study population. Children who move from household to household appear to be less likely to receive a routine eye check-up. Additionally, since a large majority of participants stated that their children regularly attend school, it would be beneficial to incorporate routine eye exams or medical screening in schools as a means of targeting and preventing childhood visual problems or blindness. Among Honduran participants, lack of financial resources and the perceived high cost of eye exams were mentioned by caregivers as significant factors hindering the acquisition of proper eye care. The Indian study population demonstrated significant misunderstandings about potential symptoms of pediatric visual impairment. Caregivers within the Indian cohort had the lowest capacity (only 8%) to detect visual symptoms. Thus, it is highly recommended that tailored adult educational programs be implemented to correct these misconceptions, as ensuring child eye health is the responsibility of parents and other caregivers.
Several significant misconceptions were also found to impede pediatric care. While this portion of the study was only conducted in India, its results may be reflective of a wider and more prevalent issue in other developing countries such as Honduras and Ghana. This study showed that a majority of participants believed that spectacles were only to be used by adults. When asked the age at which an individual requires eyeglasses, the average age stated was 39.6 years. Furthermore, less than 6% of individuals surveyed thought that children could require spectacles, while an additional 20% did not know at what age children could begin using spectacles. Several possible explanations may account for these misconceptions and corresponding high rates of uncorrected pediatric refractive error in India. First, Nirmalan et al. described that families in rural India believed children under the age of four should not wear spectacles [14]. Second, the cost of a refractive exam and spectacles for children may be another deterrent for impoverished families. Typical spectacles in rural India cost the equivalent of approximately five days’ work [25]. At KEHRC, a refractive exam and assessment by an optometrist at the clinic costs 30 rupees (approximately $0.50 USD), though comprehensive eye exams conducted by KEHRC in villages are provided free of charge. A pair of spectacles at the Kalinga Eye Hospital Optical Shop can cost between 150 rupees to 8000 rupees (approximately $3–$130 USD) depending on the brand and strength of the corrective lens. In Dhenkanal, Orissa, 150 rupees (approximately $3 USD) translates to about three weeks’ worth of bread or a low-quality sari (Indian garment worn by women).
Another prominent misconception of Indian caregivers was a lack of awareness about pediatric cataracts. Responsible for approximately 10% of childhood blindness in India, pediatric cataracts have significant implications on visual acuity [26]. The study population revealed a lack of awareness that children can be afflicted by cataracts. In addition, caretakers were not able to identify potential triggers or symptoms of this condition. Almost 60% of caregivers studied responded that children cannot acquire cataracts, while an additional 18.8% responded that they did not know if children could get cataracts in their eyes. This response further emphasizes the significant misconceptions and lack of knowledge centering potential causes of pediatric visual impairment.
Another common theme in this study is the perception of eye care as important only upon the manifestation of visible or perceived visual impairment. Almost all participants from Ghana, Honduras and India said they would take their child to the hospital or clinic if a problem arose. In India, 48.7% of participants said that children should only receive an eye exam if a problem occurs. Similarly, in Honduras, 49.0% of participants justified not bringing their children for eye exams because they had not presented any eye problems or shown any symptoms. One Honduran female study participant explained that “if there are no problems, we do not go to the doctor for prevention.” Only 32% of the Indian study population considered an annual or semiannual eye exam to be beneficial to child health.
The under-utilization of preventive care has significant implications. Half of childhood blindness is preventable with proper prenatal care, eyeglasses and treatment [27]. With proper education of pediatric visual issues and timely care, a significant number of pediatric ophthalmologic issues could be identified and treated before they become irreversible. Besides humanitarian grounds for conducting regular eye exams to prevent avoidable suffering, cursory reports suggest an economic benefit. Taylor et al. modeled the economic impact on Australia of such an intervention package and found that it would give a 4.8-fold return on investment [28]. Although this study pertains to a developed rather than developing country, it is maintained that prevention and early detection of visual maladies in developing countries may offer similar economic advantages by increasing worker productivity.
5. Conclusion
Results obtained in this study confirm that eye health education and awareness efforts in developing countries can help eliminate preventable blindness by reducing misconceptions. However, these educational campaigns should emphasize the importance of prevention as opposed to the treatment upon manifestation of a problem. One possible way to raise awareness may be the distribution of culturally-appropriate, locally-developed posters or other visual aids in waiting areas of clinics that administer eye examinations in the hopes of encouraging patients and their families who come for an eye ailment to also undergo a routine eye exam. Hill et al. noted that flyers and posters are a more reliable way to increase public health awareness than are word of mouth and other media [29]. Additionally, interventions should encourage local physicians to discuss symptoms of eye issues during exams, training community health workers to supplement information about eye care and common diseases, and instructing teachers on how to identify early childhood symptoms in school.
A potential shortcoming of this study is that the differences in subject responses between data collection sites were assumed to be negligible. In addition, the majority of participants from the surveyed sites were female. Additionally, the inferential bias for a random sample of participants, without addressing participant’s non-response bias may be a limitation, since whether or not a subject responded during the interview is itself a variable. Furthermore, while this study was conducted in rural and impoverished areas of Ghana, Honduras and India, the results may not be representative of other regions in each country. Perceptions and misconceptions may vary contingent upon socio-economic factors. The large percentage of females who participated in this study should not be underscored; while it does reflect a limitation of the study, it also reflects a broader gender role in child healthcare.
However, this study was conducted throughout predominantly rural areas where proper eye care is inaccessible to the majority of inhabitants. Finances, child motility, distance, adult visual health, a shortage of physicians, and most importantly misconceptions regarding pediatric eye health are hindering children from receiving care. An extrapolation of these results, coupled with the diversity of an international sample pool from this study, can provide a foundation for better understanding similar issues in other parts of developing countries. The authors hope that it may have an impact on the paradigms, policies and approaches taken by international and local governments and non-profit organizations in addressing pediatric eye health needs as well as the attainment of the main goal outlined in Vision 2020 – the reduction of childhood blindness and refractive error.
Authors’ contribution
DR and TP conducted surveys in Ghana, while RE and SG conducted surveys in Honduras and India, respectively. DR, RE, SG and TP participated in the design, implementation and coordination of the study. TP provided statistical assistance, and along with DR contributed to interpreting the results. DR drafted the manuscript, and RE and SG revised the manuscript for intellectual content. All authors read and gave their final approval. DR is the guarantor of the paper.
Funding
This research was supported by grants from the York College Association Fund, the DukeEngage program of Duke University, Princeton University’s Program in Latin American Studies, and the Carswell Fund of Wake Forest University.
Ethical approval
Ethical approval for this study was obtained through the Institutional Review Boards of York College of The City University of New York, Jamaica, New York (IRB# 11050160147), Duke University, Durham, North Carolina (IRB# A05), Princeton University, Princeton, New Jersey (IRB# 5792), and Wake Forest University, Winston-Salem, North Carolina (IRB# 00020761). Additional approval for this study was given by Unite For Sight, Inc. (USA), Save The Nation’s Sight Eye Clinic, Charity Eye Centre, Northwestern Eye Centre, and Crystal Eye Clinic (Ghana), Centro de Salud Integral ZOE clinic (Honduras), and Kalinga Eye Hospital & Research Centre (India). No other institutional research approval was mandatory for this study.
Conflict of interest
We have no conflict of interest to declare.
Acknowledgments
The authors would like to thank the six aforementioned clinics for their support and hospitality, and for coordinating outreach programs and access to clinics and patients.
References
Cite this article
TY - JOUR AU - Daryl Ramai AU - Ryan Elliott AU - Shoshanna Goldin AU - Tejas Pulisetty PY - 2014 DA - 2014/08/12 TI - A cross-sectional study of pediatric eye care perceptions in Ghana, Honduras, and India JO - Journal of Epidemiology and Global Health SP - 133 EP - 142 VL - 5 IS - 2 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2014.06.004 DO - 10.1016/j.jegh.2014.06.004 ID - Ramai2014 ER -
