Left atrial appendage dysfunction in acute embolic stroke young patients with sinus rhythm: Correlation with Tissue Doppler mitral annular systolic velocity
- DOI
- 10.1016/j.artres.2016.06.002How to use a DOI?
- Keywords
- Stroke; Left atrial appendage; Mitral annular systolic velocity
- Abstract
Background: Trans-esophageal echocardiogram (TEE) is a gold standard test for diagnosis of left atrial (LA) appendage function.
Aim: To evaluate left atrial appendage (LAA) dysfunction using mitral annular systolic velocity measured by tissue Doppler imaging “Sm” in acute embolic stroke young patients with sinus rhythm.
Methods: Transthoracic (TTE) and transesophageal echocardiography (TEE) were performed in 70 consecutive patients with sinus rhythm without obvious left ventricular dysfunction within 2 weeks after embolic stroke. Two groups were identified: LAA dysfunction [LAA emptying peak flow velocity (LAA-eV) <0.55 m/s, n = 28, age 52 ± 11 years] and without LAA dysfunction (LAA-eV ≥ 0.55 m/s, n = 42, age 54 ± 10 years) on TEE. Tissue Doppler mitral annular systolic velocity “Sm” was obtained in apical four chambers view on TTE and D-dimer level estimated for all patients.
Results: Sm was significantly lower in patients with than in those without LAA dysfunction (P < 0.0001). There was a significant correlation between Sm, LAVI, LAEF%, E/A ratio and LAA-eV in all selected patients groups. The optimum cut-off value of Sm for predicting LAA dysfunction was below or equal 8 cm/s (sensitivity 89.6% and specificity 94.2%).
Conclusion: Tissue Doppler mitral annular systolic velocity is an independent non-invasive easy predictor of LAA dysfunction and significantly correlated with LAA-eV (p < 0.0001) in acute embolic stroke young patients with sinus rhythm.
- Copyright
- © 2016 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Introduction
Cardio-embolic stroke is an important clinical issue, because it is the most common cause of death in patients with acute ischemic stroke.1,2 Previous clinical reports have prescribed Atrial fibrillation “AF” as independent risk factor for ischemic stroke, increasing the risk by fivefold.3,4 In a large cohort of patients with paroxysmal AF on aspirin therapy had a stroke rate similar to sustained AF as well as similar stroke risk factors.5
The left atrial appendage (LAA) was reported to be a major source of thrombo-embolism in stroke patients with atrial fibrillation.6–8Many clinical reports have indicated that left atrial mechanical remodeling is associated with thrombus formation in the LAA.9–11 The presence of spontaneous echocardiographic contrast or reduced LAA peak flow velocity, as measured by transesophageal echocardiography (TEE), was reported to be useful for detecting LAA dysfunction, which causes thrombus formation in the LAA.12,13
LAA dysfunction may play a role as an underlying cause of cardiogenic brain embolism not only in chronic AF but also in paroxysmal AF.14 Independent of the basic rhythm there is a close relationship between LAA-eV and qualitative parameters of elevated thromboembolic risk, and LAA-eV could be a quantitative parameter for risk stratification. LAA-eV ≥ 0.55 m/sec is associated with low risk of LAA thrombosis and spontaneous echo contrast.15,16
While transthoracic echocardiography (TTE) is widely used as a screening tool because it is a non-invasive procedure, it is thought to be difficult to detect LAA thrombus and evaluate LAA dysfunction by TTE. Recently pulsed wave tissue Doppler has become a reproducible and readily available technique for measuring atrial function parameters.17,18 The LAA has a close anatomic and functional relation with lateral mitral annulus and thus annular velocities obtained by TDI may reflect the LAA function.19 The aim of the present study is to evaluate LAA dysfunction using tissue Doppler mitral annular systolic velocity in acute embolic stroke young patients with sinus rhythm.
Patients
After ethical committee approval and all patients consent for the study.
The study enrolled 70 patients with sinus rhythm selected from 180 acute stroke patients (confirmed by computed tomography as recent infarction) admitted in neurology department, Tanta university hospital from October 2011 to April 2013 and referred to cardiology department for cardiac evaluation and to exclude cardiac source of embolization Patients examined within 2 weeks of infarction onset. They were divided into 2 groups according to LAA-eV value detected by TEE.
Exclusion criteria
- •
Patients with documented AF either permanent or paroxysmal AF documented by ECG or Holter monitoring.
- •
Patients with a contraindication to perform TEE such as dysphagia and esophageal stricture
- •
Patients refusal.
- •
Patients with low EF%, severe MR and severe diastolic dysfunction (E/E′ ≥ 15).
Methods
All patients are subjected to
- I.
Detailed history: History of previous attacks of stroke or TIA, hypertension, DM, hyperlipidemia, rheumatic heart disease and the presence of any condition that makes TEE contraindicated. Drug history including ACE inhibitors, anti-arrhythmic drugs and oral anticoagulation.
- II.
All patients were underwent full clinical evaluation before trans-esophageal echocardiographic evaluation.
- III.
12 leads ECG to detect and 24 h Holter monitoring to detect atrial flutter, fibrillation and ischemia.
Laboratory investigations
Including Prothrombin time (PT), International Normalized Ratio (INR) and D-Dimer measured quantitatively using immunoturbudimetric method by SYSMEX CA-1500 automated coagulometer before TEE examination.20
- IV.
Transthoracic Echocardiography:
Echocardiograms using 2D-echo and conventional Doppler performed before TEE to detect EF%, E/A ratio, wall motion abnormalities, valvular lesions, diastolic function, presence or absence of thrombi in left atrium, measure the size of the left atrium using M-mode study and LA volume.21,22 Images were obtained with the patient in the left lateral decubitus position with M3S probe Vivid7, GE Vingmed (Horton, Norway).
- V.
transesophageal echocardiography procedure:
Using 2D-echo the following data was obtained:
- 1
The presence of thrombi and the degree of spontaneous echo contrast that was graded from 0 to 4 according to the following criteria): 0 = none (absence of echogenicity); 1+ mild (minimum echogenicity located in the LAA or sparsely distributed in the main cavity of the left atrium); 2+ mild to moderate (more dense swirling pattern than 1+ but with similar distribution); 3+ moderate (dense swirling pattern in the LAA, generally associated with somewhat lesser intensity in the main cavity); 4+ severe (intense echo -density and very slow swirling patterns in the LAA, usually with similar density in the main cavity.13
- 2
Left atrial appendage for the detection of thrombi and spontaneous echo contrast.
- 3
Mitral valve study, wall motion abnormality, LVH. Color Doppler, PW, CW Doppler were also used.
LAA-eV calculation:
LAA emptying flow velocity (eV) was measured using pulsed wave Doppler, with the sample volume placed 1 cm distal from the mouth of the appendage by TEE. LAA-eV within each RR interval was determined by scanning the appendage at angles between 0° and 90°.13
The study group were divided into two groups: group (1) LAA dysfunction group [LAA emptying peak flow velocity (LAA-eV) <0.55 m/s, n = 28, age 52 ± 11 years] and group (2) without LAA dysfunction (LAA-eV ≥ 0.55 m/s, n = 42, age 54 ± 10 years).
- VII.
Tissue Doppler mitral annular systolic velocity assessment:
Pulsed-wave TDI were performed in apical four chamber, a 5 mm pulsed tissue Doppler volume was subsequently placed at lateral side of mitral annulus. The filter setting was decreased to exclude high-frequency signals and the gain minimized to allow for clear tissue signals with minimal background noise. The sample volume was positioned as parallel as possible with the lateral mitral annular motion.23 Variables of the tissue velocity evaluated were peak systolic myocardial velocity (Sm) early diastolic myocardial velocity (Em) and late diastolic myocardial velocities (Am).
Statistical analysis
Results are expressed as means ± standard deviation (SD) for continuous variables and as percentages of the total number of patients for categorical variables. Statistical analyses were performed using SPSS statistical package version. T-tests were used for comparison of continuous variables and Z tests used to compare two proportion.
Multivariate analysis correlation in-between LAA-eV and different echocardiographic parameters done using linear regression test. A receiver operating characteristic (ROC) curve was constructed to determine Sm cut-off value giving optimum sensitivity and specificity for predicting LAA dysfunction.
Inter- and intra-observer agreement on Echocardiographic and Doppler measurements were evaluated by Pearon’s r –test.
Results
Table 1: shows the clinical characteristics of the 180 patients with acute stroke. The mean age was 55 ± 13years, 60% of the patients were men, and 45 patients had AF (14 paroxysmal AF, 31chronic AF). The etiology was cardio-embolic stroke in 63.8% (115 patients, 45 AF excluded and 70 sinus rhythm), athero-thrombotic stroke in 30% (excluded), and lacunar stroke in 6.1% of patients (excluded).
| Parameters | Values |
|---|---|
| Age | 55 ± 13 |
| Sex | 108 males (60%) |
| Hypertension | 130 (72%) |
| Dyslipidemia | 98 (54.4%) |
| Diabetes mellitus | 40 (22%) |
| Smoking | 84 (46.6%) |
| Previous stroke | 45 (25%) |
| Paroxysmal AF | 14 (7.7%) |
| Chronic AF | 31 (17.3%) |
| CHA2DS2VASc score | 2.7 ± 1.2 |
| Medications | |
| Anticoagulants | 38 (21%) |
| Warfarin | 30 (16.6%) |
| Dabigatran | 8 (4.4%) |
| Anti-arrhythmic medications | 33 (18.3%) |
| Anti-HTN medications | 72 (40%) |
| ACE inhibitors | 38 (21%) |
| ARBs | 20 (11%) |
| Clinical categories | |
| Cardio-embolic stroke | 115 (63.9) |
| Athero-thrombotic stroke | 54 (30%) |
| Lacunar stroke | 11 (6.1%) |
AF = atrial fibrillation, CHA2DS2VASc score before onset of acute stroke.
Clinical characteristics of all patients (180 patients).
The clinical characteristics of the patients with or without LAA dysfunction are shown in Table 2. There were 28 patients with LAA dysfunction, 4 of them LAA thrombus detected and 9 spontaneous echo contrast (6 grade III, 3 grade II).
| Parameters | Without LAA dysfunction = 42 (LAA-ev ≥ 0.55) | With LAA dysfunction = 28 (LAA-ev < 0.55) | P value |
|---|---|---|---|
| Age | 54 ± 10 | 52 ± 11 | 0.43 |
| Sex(male) | 25 (59.5%) | 17 (60.7%) | 0.9 |
| Hypertension | 21 (50%) | 11 (39.2%) | 0.36 |
| Dyslipidemia | 21 (50%) | 15 (53.5%) | 0.38 |
| Diabetes mellitus | 7 (16.6%) | 4 (14.2%) | 0.78 |
| Smoking | 19 (45.2%) | 13 (46.4%) | 0.46 |
| Rheumatic heart disease | 17 (40%) | 15 (53%) | 0.28 |
| Previous stroke | 7 (16%) | 4 (14.3%) | 0.84 |
| Medications | |||
| Anti-coagulants (added after TEE) | – | 11 | S |
| Warfarin | 9 | ||
| Dabigatran | 2 | ||
LAA eV = left atrial appendage emptying flow velocity.
Clinical characteristics of patients with cardio-embolic stroke and sinus rhythm (70 patients).
Patients with LAA dysfunction (LAA-eV < 0.55) had significantly greater E/A ratio, LAEF%, D-dimer and LAVI values compared to those without LAA dysfunction (LAA-eV ≥ 0.55) Table 3. Sm was significantly lower in patients with than in those without LAA dysfunction (P < 0.0001) Table 3, Fig. 2. There were no significant differences in Simpson LVEF, E′, E/E′ ratio, A′ between patients with or without LAA dysfunction (Table 3).
| With LAA dysfunction(LAA-ev < 0.55) = 28 pt | Without LAA dysfunction(LAA-ev ≥ 0.55) = 42 pt | P value | |
|---|---|---|---|
| LAD(mm) | 41 ± 7 | 38 ± 8 | 0.1 |
| LVEDD(mm) | 48 ± 5 | 47 + 7 | 0.9 |
| Simpson LVEF (%) | 63 ± 10 | 59 ± 11 | 0.79 |
| E/A | 1.09 ± 0.35 | 0.87 ± 0.29 | 0.0045 |
| Patent foramen ovale | 3 (10%) | 2 (4%) | 0.35 |
| LAVI(ml/m2) | 34 ± 15 | 26 ± 12 | 0.016 |
| E/E′ | 12.7 ± 1.8 | 11.9 ± 1.6 | 0.055 |
| E′m | 9.7 ± 0.9 | 10.2 ± 1.3 | 0.08 |
| A′m | 8.8 ± 1.4 | 9.4 ± 1.2 | 0.06 |
| E′m/A′m | 1.12 ± 0.15 | 1.2 ± 0.18 | 0.056 |
| LAEF (%) | 32.5 ± 15.3 | 43.7 ± 19.2 | 0.012 |
| Sm(cm/sec) | 7.1 ± 0.9 | 11.6 ± 1.0 | <0.0001 |
| D-dimer | 349 ± 97 | 298 ± 92 | 0.03 |
LAD = left atrial dimension; LVDd = left ventricular end-diastolic dimension; LVEF = left ventricular ejection fraction; E/E′ = the ratio of the early transmitral flow velocity and the early mitral annular velocity; LAVI = left atrial volume index; LAEF = left atrial emptying fraction.
LAA eV = left atrial appendage emptying flow velocity, E/A = early diastolic to late diastolic mitral flow Doppler velocities ratio, E′ = early diastolic mitral annular velocity, A′ = late diastolic mitral annular velocity.
Echocardiographic and tissue Doppler imaging characteristics of patients with cardio-embolic stroke and sinus rhythm (70 patients).
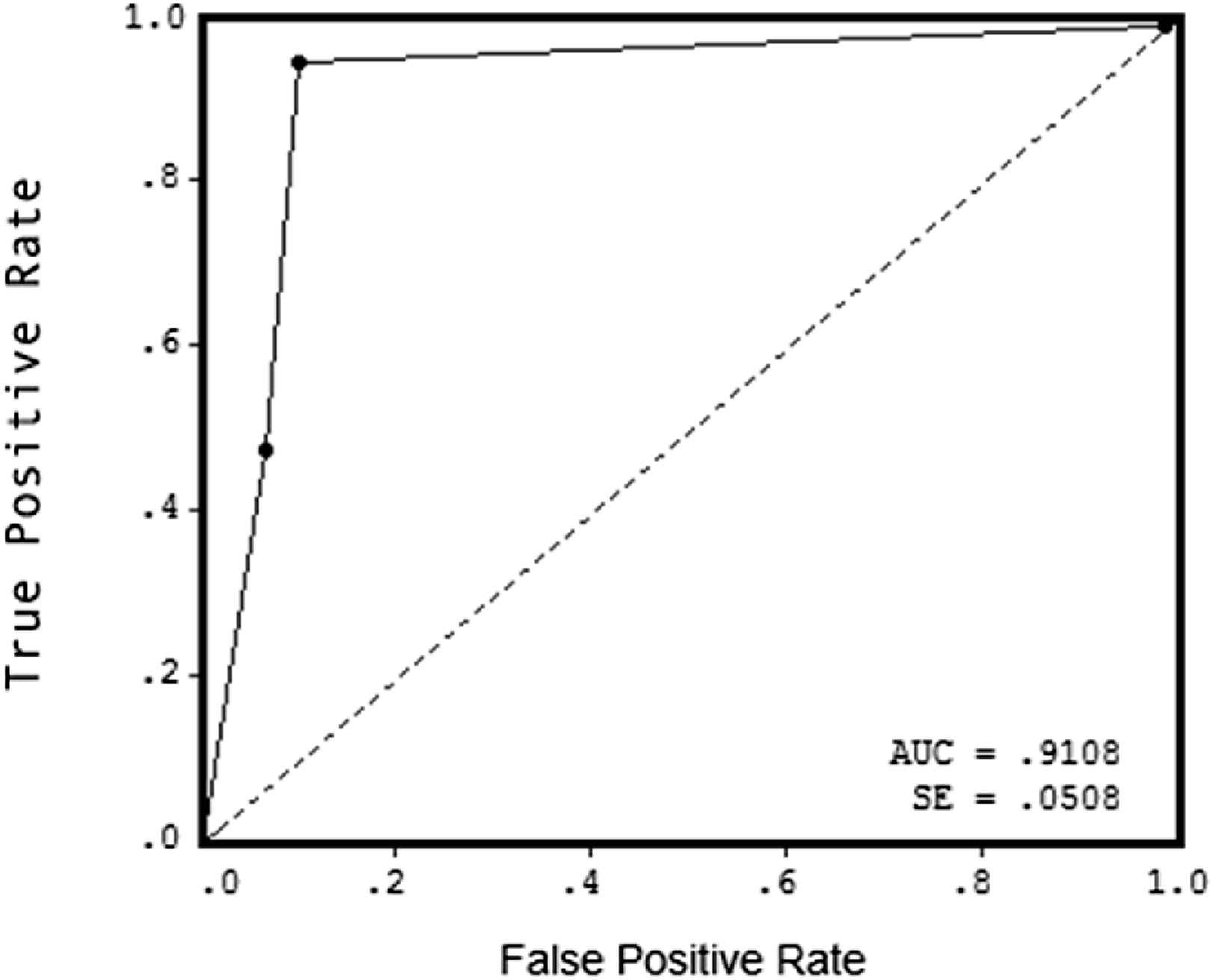
ROC curve to detect Sm sensitivity % specificity %for LAA dysfunction diagnosis.
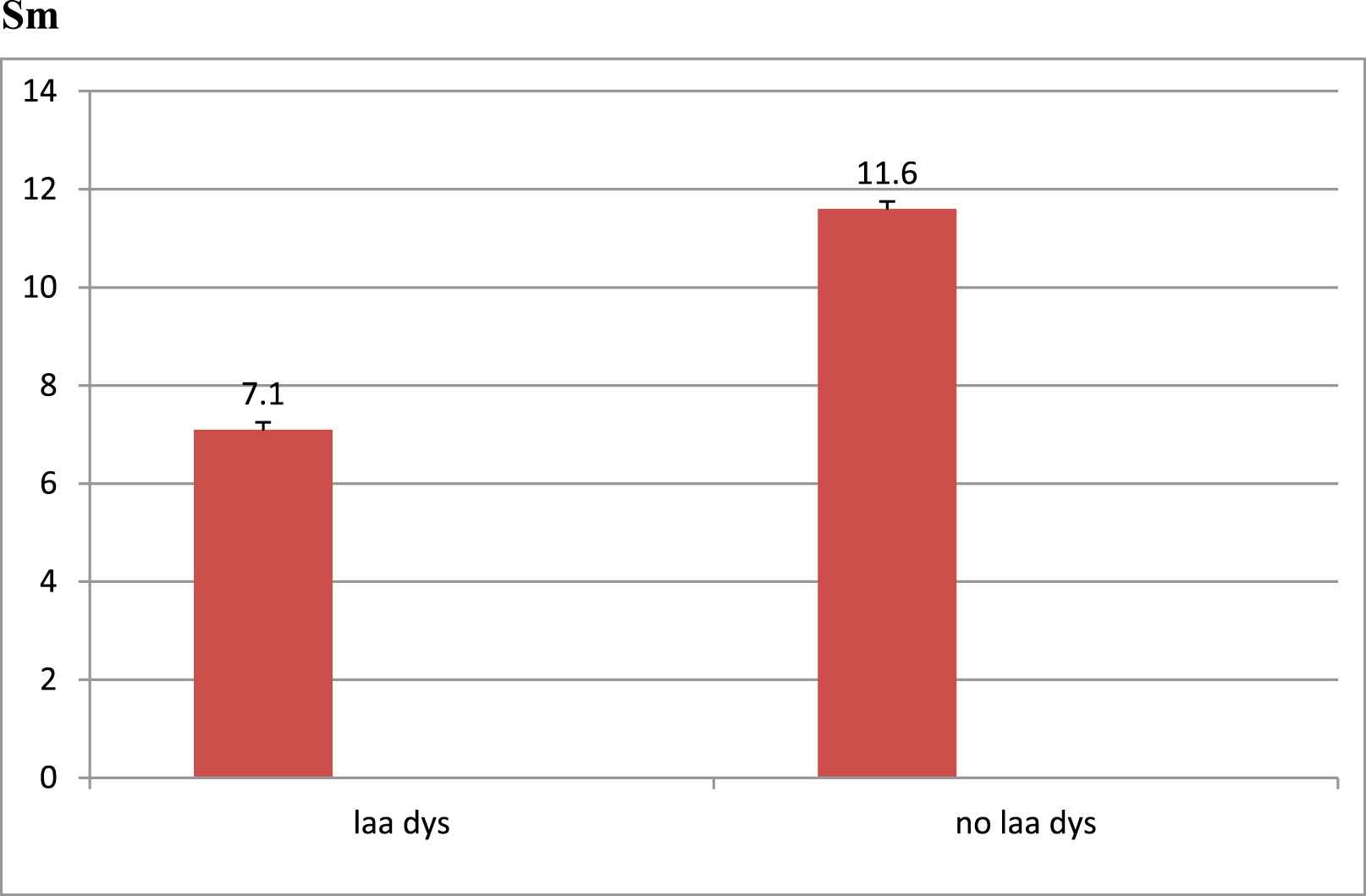
Sm mean values in LAA dysfunction and normal function group (p < 0.0001).
A significant positive strong correlation between measurements obtained for inter-observer agreement r = 0.94 and P < 0.001, and intra-observer agreement r = 0.97, P < 0.001.
There was a significant correlation between Sm, LAVI, LAEF%, E/A ratio and LAA-eV in all selected patients groups (Table 4, Fig. 3). The optimum cut-off value of Sm for predicting LAA dysfunction was determined by ROC curve analysis; Sm below or equal 8 cm/s had a sensitivity of 89.6% and a specificity of 94.2%.The area under the ROC curve (AUC) of Sm was 0.91 (Table 5, Fig. 1).
| Parameters | F Value | P Value |
|---|---|---|
| LAVI | 12.17 | 0.017 |
| LAEF% | 8.24 | 0.034 |
| E/A | 15.3 | 0.011 |
| D-dimer | 6.266 | 0.055 |
| Sm | 98.9 | <0.0001 |
Linear regression correlations in-between LAA-ev and different parameters.
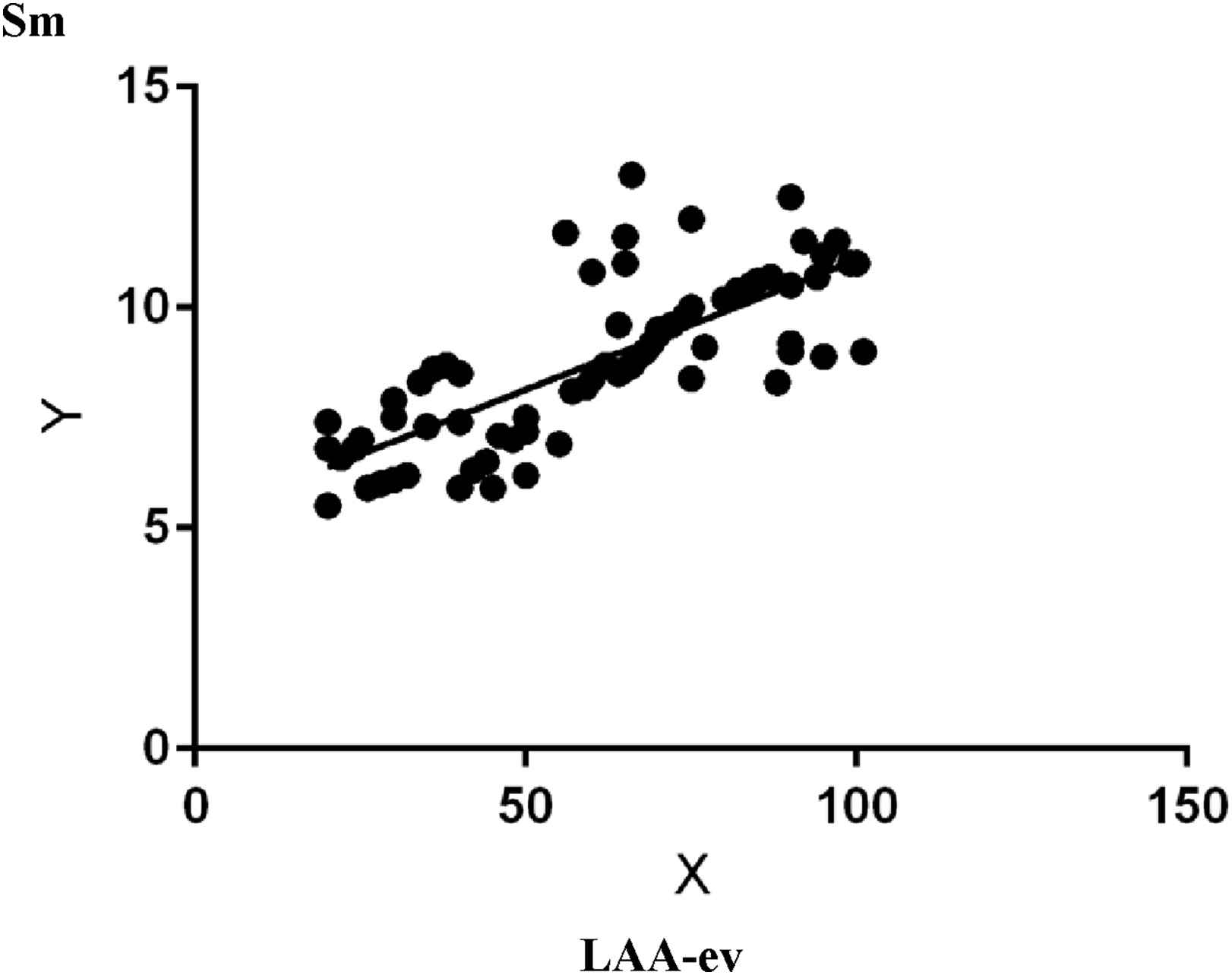
Linear regression correlation of Sm and LAA-ev (X = LAA-ev, Y = Sm).
| Parameters | Cut off point | AUC | Sensitivity | Specificity |
|---|---|---|---|---|
| LAVI | 28 | 0.55 | 70% | 55% |
| E/A | 0.95 | 0.34 | 60% | 62% |
| LAEF% | 30% | 0.3 | 56% | 65% |
| Sm | 8 | 0.91 | 89.6% | 94.2% |
ROC curve calculation of sensitivity and specificity of different parameters.
Discussion
It is well known that TEE parameters for evaluating LAA dysfunction can predict LAA thrombus formation.9–11The presence of spontaneous echo contrast and low LAA eV was reported to be reliable markers for stratifying patients with AF for the risk of thromboembolism.10 In addition, TTE parameters such as increased LAD, decreased LA fractional shortening, and increased trans-mitral inflow velocities (E/A) were useful predictors for LAA thrombus. However their predictive values for detecting LAA thrombus were much lower than those of TEE parameters.24,25
Recently, studies reported that left atrial wall velocity “LAWV” as measured by TTE can be used to stratify patients with AF for the risk of cardiac stroke.26,27 However, LAWV cannot necessarily be accurately measured because of the inherent angle dependence. LA peak systolic strain may be a more sensitive parameter than LAWV. It is known that there are three types of LA mechanical function: reservoir, conduit and booster pump function.28 LA peak systolic strain reflects LA reservoir function. Since LAA clamping during cardiac surgery markedly increases LA pressure and volume, it has been suggested that the LAA may contribute to LA reservoir function, especially in the presence of LA pressure and/or volume overload.29 Saha et al. (2011) reported that LA strain is an integrated marker of dynamic LA function that shows high reproducibility and identifies patients who are at high clinical risk of thromboembolism as defined by CHADS2 score.30 Shih et al. (2011). also reported that LA strain and strain rate are independently associated with stroke in patients with permanent AF.31 Sasaki et al. (2014) have shown a relationship between LA strain and LAA dysfunction such as thrombus formation, in patients with acute ischemic stroke.32
However, all above mentioned studies revealed a relationship between LAWV, LA-strain and LAA appendage dysfunction in embolic stroke patients, AF patients were the most of the studied group either permanent or paroxysmal. The current study is the first one demonstrated that there is a relationship between Sm as an easy, non-invasive parameter measured by tissue Doppler and LAA function in acute cardio-embolic stroke young patients with sinus rhythm. Sm was significantly correlated with LAA-eV in patients with sinus rhythm. Multivariate regression analysis showed that a decrease in Sm < 8 cm/se was an independent predictor of LAA dysfunction with 89.6% sensitivity and 94.2% specificity in patients with acute ischemic stroke in sinus rhythm.
Previously, Sasaki et al. 201432 investigated whether decreased LA strain may predict LAA dysfunction and thrombus formation in patients with acute ischemic stroke in 120 patients (mean age 72 ± 11 years) within 7 days of onset of an acute ischemic stroke. LA peak systolic strain was significantly decreased in patients with LAA dysfunction compared to those without (32.3± 13.7% vs. 12.1± 7.2%, p < 0.0001). LA peak systolic strain was significantly correlated with LAA emptying flow velocity (p < 0.0001). The optimum LA peak systolic strain cut-off value for predicting LAA dysfunction was 19% with 92% sensitivity and 86% specificity. The present study differs from Sasaki et al. study in selection of young group of patients with sinus rhythm, Sasaki et al. study included AF patient in the study and also the present study was restricted to cardio-embolic sources only.
Moreover, Kaneko 201433 evaluated left atrial appendage (LAA) dysfunction using left atrial pulse-wave tissue Doppler imaging (PW-TDI) in acute cerebral embolism patients with sinus rhythm (SR), transthoracic (TTE) and transesophageal echocardiography (TEE) were performed in 60 consecutive patients with SR without obvious left ventricular dysfunction within 2 weeks after ACE. Two groups were identified: LAA dysfunction (LAA emptying peak flow velocity (LAA-eV) <0.55 m/s) and without LAA dysfunction (LAA-eV ≥ 0.55 m/s) on TEE. Left atrial wall motion velocity (WMV) was obtained from PW-TDI. It was significantly lower in the group with versus without LAA dysfunction and prevalence of paroxysmal atrial fibrillation, left atrial volume index, and serum levels of brain natriuretic peptide were significantly higher. They concluded that La’ was an independent predictor of LAA dysfunction and was significantly correlated with LAA-eV (p < 0.0001) and LAA fractional area change (p < 0.0001). The La’ optimal cut-off value for LAA-ev < 0.55 m/s was 5.5 cm/s (sensitivity 83%, specificity 88%).
From our point of view the present study endorses a new simple non-invasive parameter to diagnose LAA dysfunction and select patients indicated for TEE. This also raise the possibility of anti-coagulation in cardio-embolic stroke young patients with sinus rhythm. Further larger multi-centers studies on larger number of patients are needed to compare between different parameters sensitivity, specificity to diagnose LAA dysfunction in same group of patients, either to select one or to gather different parameters for higher level LAA dysfunction prediction.
Conclusion
Tissue Doppler mitral annular systolic velocity is an independent non-invasive easy predictor of LAA dysfunction and significantly correlated with LAA-eV (p < 0.0001). The optimal cut-off value for Sm < 8 cm/se (sensitivity 89.6%, specificity 94.2%) is a useful and convenient strong predictor of LAA dysfunction in acute embolic stroke young patients with sinus rhythm.
Study limitations
- 1
small number of study group
- 2
No control group as TEE is semi-invasive procedure, none accepted to do without a cause.
Conflict of interests
None declared.
Abbreviations
- Sm
mitral annular systolic velocity
- LAA
left atrial appendage
- LAA-ev
left atrial appendage emptying velocity
- TTE
trans-thoracic echocardiography
- TEE
trans-esophageal echocardiography
- LAD
left atrial dimension
- LVDd
left ventricular end-diastolic dimension
- LVEF
left ventricular ejection fraction
- E/E′
the ratio of the early transmitral flow velocity and the early mitral annular velocity
- LAVI
left atrial volume index
- LAEF
left atrial emptying fraction
- TDI
tissue Doppler imaging
References
Cite this article
TY - JOUR AU - Rania Gaber AU - Mai Salama PY - 2016 DA - 2016/07/04 TI - Left atrial appendage dysfunction in acute embolic stroke young patients with sinus rhythm: Correlation with Tissue Doppler mitral annular systolic velocity JO - Artery Research SP - 12 EP - 18 VL - 15 IS - C SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2016.06.002 DO - 10.1016/j.artres.2016.06.002 ID - Gaber2016 ER -
