Screening Strategy of Active Pulmonary Tuberculosis in Sheltered Homeless People in Marseille, 2019
 , Floriane Holi-Jamovski3, Van Thuan Hoang1, 2, 4,
, Floriane Holi-Jamovski3, Van Thuan Hoang1, 2, 4,  , Ndiaw Goumballa1, 2, 5, Meriem Louni1, 2, Thi Loi Dao1, 2, 6,
, Ndiaw Goumballa1, 2, 5, Meriem Louni1, 2, Thi Loi Dao1, 2, 6,  , Michel Drancourt2, 7, Philippe Gautret1, 2, *,
, Michel Drancourt2, 7, Philippe Gautret1, 2, *, 
- DOI
- 10.2991/jegh.k.201009.001How to use a DOI?
- Keywords
- Active pulmonary tuberculosis; tuberculosis-screening questionnaire; chest X-ray; microscopical testing; GeneXpert MTB/RIF assays; culture
- Abstract
We aimed to assess the reliability of a screening questionnaire for Active Pulmonary Tuberculosis (APTB) in a population of sheltered homeless persons (HP). Participants from two homeless shelters completed a questionnaire specially designed to identify patients at high-risk of APTB (available at www.tb-screen.ch), underwent a Chest X-ray (CXR), and provided sputum samples. Computed Tomography (CT) scanning was subsequently performed on those which had images consistent with APTB. Microscopical examination, real-time polymerase chain reaction (qPCR) and culture testing were applied for Mycobacterium tuberculosis complex detection. Additionally, we retrospectively selected 16 HP hospitalised in our hospital between 2017 and 2019 with biologically confirmed tuberculosis and typical CXR images, and retrospectively documented a screening questionnaire by reviewing their medical files. Overall, the population (n = 383 HP) was predominantly migrants (87%). Forty-seven individuals (11.7%) had positive screening questionnaire scores and four (2.4%) displayed abnormal CXR features consistent with APTB. Three of them three underwent CT scanning that ruled out APTB and one was lost to follow-up. None tested positive through microbiological investigation. Fifteen (of 16, 93.8%) hospitalised patients with biologically confirmed APTB had a positive screening questionnaire score. The sensitivity and specificity of questionnaire for confirmed APTB were 93.8% and 87.7%, respectively. Screening questionnaires can be used as a first assessment tool in people arriving at homeless shelters and to refer those screening positive for a CXR.
- Copyright
- © 2020 The Authors. Published by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
In France, the annual incidence of Active Pulmonary Tuberculosis (APTB) in 2018 was 5.4 per 105 individuals, and the trend of morbidity and mortality regularly decreased over the past 20 years [1,2]. Nevertheless, concentrated epidemics continue to occur among hard-to-reach groups such as homeless people and migrants [1,2]. Homeless people accounted for 7% of all new ATPB cases in Marseille (France) in 2016, while the homeless population in Marseille represents only around 0.2% of the population [3]. Over the past two decades, we have seen a change in the sheltered homeless population in Marseille, with a rising proportion of migrants [4]. All of the nine homeless APTB patients hospitalised at our hospital between 2017 and 2018 were migrants [5]. Screening for APTB in homeless people is, therefore, of major importance in terms of public health.
In a preliminary study conducted by our team in 2018, in two Marseille homeless shelters, we showed that the use a short questionnaire aiming at screening for APTB [6] was well accepted by both homeless persons and medical staff during Chest X-ray (CXR)-based TB screening campaigns [3]. In this paper, we report the results of cross-sectional 1-day surveys conducted at these two Marseille homeless shelters in 2019, where all participants were investigated using questionnaire, chest radiography and microbiological examination of respiratory samples, with the aim of assessing the reliability of this screening questionnaire in a population of sheltered homeless people.
2. MATERIALS AND METHODS
2.1. Ethics
Ethical approval was obtained from the Marseille Institutional Review Board and Ethics Committee (Protocol number: 2010-A01406-33). Written informed consent was obtained from the survey participants.
2.2. Setting, Study Design and Population
In this cross-sectional 1-day survey, adult homeless people housed in shelters A and B in Marseille were recruited on a voluntary basis during three campaigns conducted in March, May, and December 2019. Participants were systematically asked to provide basic demographic information and information on their smoking habits, and to complete a questionnaire specially designed to identify patients at a high risk of APTB [6]. Mobile CXR were systematically performed on site at enrolment and analysed by a pneumonologist. Finally, two sputum samples were systematically collected from each participant, including one in a sterile vial for microscopic examination and real-time PCR, and another in a vial containing transport medium (C-Top TransBK liquid medium, Eurobio Scientific, Ulis, France) for mycobacterial culture. Samples from patients testing positive through the questionnaire screening and/or CXR with images consistent with APTB, and/or with a positive microscopic examination were further tested by qPCR (Figure 1).
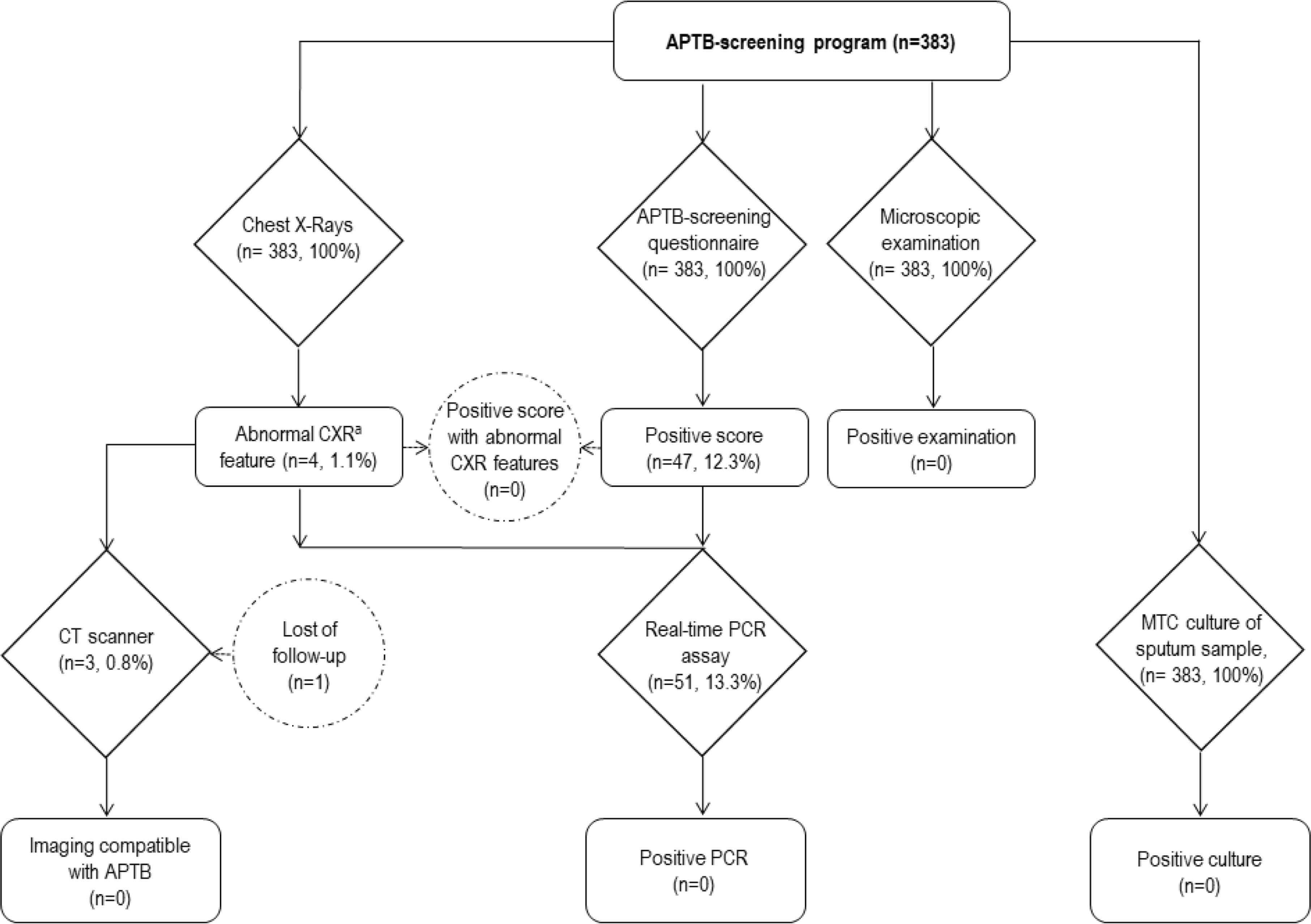
Flow chart for pulmonary tuberculosis screening among homeless participants. aAbnormal CXR feature consistent with pulmonary TB. MTC, Mycobacterium tuberculosis complex.
In addition, we retrospectively selected sixteen homeless patients hospitalised in our hospital between 2017 and 2019 with biologically confirmed tuberculosis and typical CXR images, and retrospectively documented a screening questionnaire by reviewing their medical files.
2.3. Questionnaire
The questionnaire is designed to identify patients at high risk of APTB, based on their country of origin, clinical data, history of TB, and contact with TB patients (www.tb-screen.ch, version 4.3.1 updated 3 January 2018) [6]. The questionnaire comprised nine closed simple questions available in 32 differences languages (together with visual and audio formats) that takes a short time to complete. Participants with a score ≥10 are considered likely to be suffering from APTB. Questionnaires were administered by nurses under the supervision of medical doctors.
2.4. Chest Radiography
All CXRs with images consistent with APTB were double-checked by radiologists within 48 h and patients with abnormal findings underwent a Computed Tomography (CT) scan within 2 weeks, when possible.
2.5. Laboratory Procedure
Quality of expectorated sputum specimens was assessed using quantification of squamous epithelial cells and polymorphonuclear cells per low-power field, in a Gram-stained smear of the specimen. Sputum samples were stained using a kit featuring Kinyoun staining (Cold ZN, RAL, Toulouse, France) and scanned by automated microscopy (Axio Scan Z1 Digital Slide Scanner, Zeiss, Germany) [7]. Positive results were confirmed by classical microscopic examination after Ziehl–Neelsen staining. qPCR (GeneXpert MTB/RIF assays, Cepheid, Sunnyvale, CA, USA) was performed to detect Mycobacterium tuberculosis and rifampicin resistance genes, according to the manufacturer’s recommendations. Participants were informed of their microscopy and qPCR results within 72 h of recruitment. Culture of M. tuberculosis Complex (MTC) organisms was carried out on solid culture media including Coletsos medium (bioMérieux, France) for all samples for up to 6 weeks. The case definition for confirmed APTB was a positive qPCR (highly sensitive detection method) and/or a positive culture for MTC organisms which is considered the gold standard. If an individual was confirmed to have APTB, they were referred to hospital.
2.6. Statistical Analysis
Data were collected and analysed using SPSS (version 23.0, IBM, USA). Percentage differences were tested using Pearson’s chi-square or Fisher’s exact tests when appropriate. The theoretical normal distribution of quantitative data was assessed using Shapiro–Wilks test and means of quantitative data were compared using the Wilcoxon signed-rank test when samples were not normally distributed. A p-value <0.05 was considered to be statistically significant. The sensitivity and specificity of questionnaire for confirmed APTB were also calculated.
3. RESULTS
3.1. Characteristics of Individuals Participating in Screening Campaigns
Overall, 383 subjects volunteered to participate in this study, accounting for an estimated 40% of homeless people sheltered within in two shelters at the time of enrolment (Table 1). About two-thirds were recruited from shelter A. All subjects were male, and their mean age was 40 years. The majority of participants were migrants and had settled in France approximately 6 years before the survey took place. Two-thirds had health insurance when they were recruited. A proportion of 53.5% of patients reported that they smoked tobacco.
| Characteristics | Total | Positive screening according to questionnaire | Negative screening according to questionnaire | p-valuea |
|---|---|---|---|---|
| Total | 383 | 47 | 336 | – |
| Shelter | ||||
| A | 266 (69.5) | 36 (76.6) | 230 (68.5) | 0.26 |
| B | 117 (30.5) | 11 (23.4) | 106 (31.5) | – |
| Sex | ||||
| Male | 383 (100) | 47 (100) | 336 (100) | 1.00 |
| Female | 0 (0) | 0 (0) | 0 (0) | – |
| Mean age (years, SD) | 40.0 ± 16.6 | 40.0 ± 15.0 | 40.0 ± 16.8 | 0.76c |
| Age range (years)b | 18–90 | 22–82 | 18–90 | – |
| ≤34 years of age | 196 (53.3) | 22 (46.8) | 174 (51.9) | 0.51 |
| >34 years of age | 186 (48.7) | 25 (53.2) | 161 (48.1) | – |
| Unknown | 1 (-) | – | – | – |
| Geographical origin | ||||
| France | 50 (13.1) | 6 (12.8) | 44 (13.1) | N/A |
| Other countries | 333 (86.8) | 41 (87.2) | 292 (86.9) | – |
| Mean duration of residence in France for migrants (SD) | 6.1 (0–19.1) | 6.6 (0–19.9) | 6.0 (0–18.9) | 0.68c |
| Range of duration of residence in France for migrantsb | 1 week to 59 years | 1 month to 48 years | 1 week to 59 years | – |
| ≥10 months | 154 (50.8) | 20 (57.1) | 134 (50.0) | 0.43 |
| <10 months | 149 (49.2) | 15 (42.9) | 134 (50.0) | – |
| Health insurance | ||||
| Yes | 254 (66.3) | 34 (72.3) | 220 (65.5) | 0.35 |
| No | 129 (33.7) | 13 (27.7) | 116 (34.5) | – |
| Tobacco consumption | 205 (53.5) | 24 (51.1) | 181 (53.9) | 0.72 |
Comparison between positive questionnaire group and negative questionnaire group.
Median of the variable is used for analysis.
Wilcoxon signed-rank test was used.
SD, standard deviation; N/A, not applicable.
Characteristics of homeless population (n = 383 individuals) participating in screening campaigns
3.2. Screening Questionnaire
The results of the screening questionnaires are summarised in Tables 2 and 3. Forty-seven participants (12.3%) screened positive (with a score ≥10), and 336 (87.7%) screened negative (with a score <10). Five (of 383, 1.3%) participants came from countries with a national TB incidence over 500/100,000 inhabitants or a national Multidrug-resistant Tuberculosis (MDR-TB) incidence higher than 20/100,000 inhabitants, including Russia (n = 2), Georgia (n = 2), and Somalia (n = 1). Regarding alleged symptoms, 21.7% of individuals reported recent weight loss; 21.4% currently felt ill; 21.1% reported a productive cough and 13.3% reported a prolonged cough; 11.0% reported sweating at night. A proportion of 4.7% of participants reported previous TB treatment and 3.1% reported TB in close relatives. The investigators considered 8.1% of the participants to be in poor health.
| Items | Total | Positive screening | Negative screening |
|---|---|---|---|
| Total | 383 | 47 | 336 |
| Mean of score (SD, range) | 4.9 ± 3.5 (0–16) | 11.7 ± 1.7 (10–16) | 4.0 ± 2.5 (0–9) |
| Part 1. (Q0) Country of origin (0–8 points) | |||
| 0 if national TB incidence <20/100,000 | 67 (17.5) | 7 (14.9) | 60 (17.9) |
| 1 if 20–49/100,000 | 32 (8.4) | 0 (0) | 32 (9.5) |
| 2 if 50–99/100,000 | 123 (32.1) | 11 (23.4) | 112 (33.3) |
| 3 if 100–149/100,000 | 38 (9.9) | 0 (0) | 38 (11.3) |
| 4 if 150–199/100,000 | 50 (13.1) | 10 (21.3) | 40 (11.9) |
| 5 if 200–299/100,000 | 5 (1.3) | 0 (0) | 5 (1.3) |
| 6 if 300–399/100,000 | 63 (16.4) | 18 (38.3) | 45 (13.4) |
| 7 if 400–499/100,000 | 0 (0) | 0 (0) | (0) |
| 8 if ≥500/100,000 or if national MDR-TB incidence ≥20/100,000 | 5 (1.3) | 1 (2.1) | 4 (1.2) |
| Part 2. Interview questions (0–16 points) | |||
| Q1. Cough (4 points if positive answer: have you been coughing for more than 3 weeks?) | 51 (13.3) | 26 (55.3) | 25 (7.4) |
| Q2. Cough with phlegm (2 if positive answer) | 81 (21.1) | 30 (63.8) | 51 (15.2) |
| Q3. Weight loss over the last 3 months (1 if positive answer) | 83 (21.7) | 34 (72.3) | 49 (16.4) |
| Q4. Sweat at night (1 if positive answer) | 42 (11.0) | 18 (38.3) | 24 (11.2) |
| Q5. Previous TB treatment (1 if positive answer) | 18 (4.7) | 4 (8.5) | 14 (4.2) |
| Q6. TB in member of immediate family (1 if positive answer) | 12 (3.1) | 7 (2.1) | 5 (10.6) |
| Q7. Currently feeling ill (3 if positive answer) | 82 (21.4) | 35 (74.5) | 47 (14.0) |
| Q8. Impression of poor health by the examiner (3 if positive answer) | 31 (8.1) | 14 (29.8) | 17 (5.1) |
Q0–Q8, question from 0 to 8.
Tuberculosis screening questionnaire
| ID code | Score | Total score | CXRa | ME | qPCRb | Culturec | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Participant | Country of origin (Q0) | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | |||||
| N°1 | Ivory Coast (4) | 4 | 2 | 1 | 1 | 0 | 1 | 3 | 0 | 16 | Normal | NEG | NEG | NEG |
| N°2 | Nigeria (6) | 4 | 2 | 1 | 0 | 0 | 0 | 0 | 3 | 16 | Normal | NEG | NEG | NEG |
| N°3 | Russia (8) | 4 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 15 | Normal | NEG | NEG | NEG |
| N°4 | Algeria (2) | 4 | 2 | 1 | 0 | 0 | 0 | 3 | 3 | 15 | Normal | NEG | NEG | NEG |
| N°5 | Algeria (2) | 4 | 2 | 1 | 0 | 0 | 0 | 3 | 3 | 15 | Normal | NEG | NEG | NEG |
| N°6 | France (0) | 4 | 2 | 1 | 1 | 0 | 0 | 3 | 3 | 14 | Normal | NEG | NEG | NEG |
| N°7 | Algeria (2) | 4 | 2 | 0 | 1 | 0 | 1 | 3 | 0 | 13 | Normal | NEG | NEG | NEG |
| N°8 | Nigeria (6) | 0 | 2 | 1 | 1 | 0 | 0 | 3 | 0 | 13 | Normal | NEG | NEG | NEG |
| N°9 | Nigeria (6) | 0 | 2 | 1 | 1 | 0 | 0 | 3 | 0 | 13 | Normal | NEG | NEG | NEG |
| N°10 | Niger (6) | 4 | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 13 | Normal | NEG | NEG | NEG |
| N°11 | Nigeria (6) | 0 | 2 | 1 | 1 | 0 | 0 | 3 | 0 | 13 | Normal | NEG | NEG | NEG |
| N°12 | Nigeria (6) | 0 | 0 | 1 | 0 | 0 | 0 | 3 | 3 | 13 | Normal | NEG | NEG | NEG |
| N°13 | France (0) | 4 | 2 | 1 | 0 | 0 | 0 | 3 | 3 | 13 | Normal | NEG | NEG | NEG |
| N°14 | Guinea (4) | 0 | 0 | 1 | 0 | 0 | 1 | 3 | 3 | 12 | Normal | NEG | NEG | NEG |
| N°15 | Guinea (4) | 4 | 2 | 1 | 1 | 0 | 0 | 0 | 0 | 12 | Normal | NEG | NEG | NEG |
| N°16 | Algeria (2) | 4 | 0 | 0 | 0 | 0 | 0 | 3 | 3 | 12 | Normal | NEG | NEG | NEG |
| N°17 | Algeria (2) | 4 | 2 | 1 | 0 | 0 | 0 | 3 | 0 | 12 | Normal | NEG | NEG | NEG |
| N°18 | Algeria (2) | 0 | 2 | 1 | 1 | 0 | 0 | 3 | 3 | 12 | Normal | NEG | NEG | NEG |
| N°19 | Nigeria (6) | 0 | 2 | 1 | 0 | 0 | 0 | 3 | 0 | 12 | Normal | NEG | NEG | NEG |
| N°20 | Nigeria (6) | 0 | 2 | 0 | 1 | 0 | 0 | 3 | 0 | 12 | Normal | NEG | NEG | NEG |
| N°21 | Algeria (2) | 4 | 2 | 1 | 0 | 0 | 0 | 3 | 0 | 12 | Normal | NEG | NEG | NEG |
| N°22 | France (0) | 0 | 2 | 1 | 0 | 1 | 1 | 3 | 3 | 11 | Normal | NEG | NEG | NEG |
| N°23 | Guinea (4) | 4 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 11 | Normal | NEG | NEG | NEG |
| N°24 | Guinea (4) | 4 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 11 | Normal | NEG | NEG | NEG |
| N°25 | Guinea (4) | 0 | 2 | 1 | 1 | 0 | 0 | 3 | 0 | 11 | Normal | NEG | NEG | NEG |
| N°26 | Niger (6) | 4 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 11 | Normal | NEG | NEG | NEG |
| N°27 | Algeria (2) | 4 | 2 | 0 | 0 | 0 | 0 | 3 | 0 | 11 | Normal | NEG | NEG | NEG |
| N°28 | France (0) | 4 | 2 | 1 | 1 | 0 | 0 | 3 | 0 | 11 | Normal | NEG | NEG | NEG |
| N°29 | France (0) | 4 | 2 | 1 | 1 | 0 | 0 | 3 | 0 | 11 | Normal | NEG | NEG | NEG |
| N°30 | Algeria (2) | 4 | 2 | 0 | 0 | 0 | 0 | 0 | 3 | 11 | Normal | NEG | NEG | NEG |
| N°31 | Nigeria (6) | 0 | 0 | 1 | 1 | 0 | 0 | 3 | 0 | 11 | Normal | NEG | NEG | NEG |
| N°32 | Nigeria (6) | 0 | 0 | 1 | 1 | 0 | 0 | 3 | 0 | 11 | Normal | NEG | NEG | NEG |
| N°33 | Algeria (2) | 0 | 2 | 1 | 0 | 0 | 0 | 3 | 3 | 11 | Normal | NEG | NEG | NEG |
| N°34 | Guinea (4) | 4 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 10 | Normal | NEG | NEG | NEG |
| N°35 | Guinea (4) | 4 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 10 | Normal | NEG | NEG | NEG |
| N°36 | Nigeria (6) | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 10 | Normal | NEG | NEG | NEG |
| N°37 | Guinea (4) | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 3 | 10 | Normal | NEG | NEG | NEG |
| N°38 | Romania (0) | 4 | 2 | 0 | 0 | 1 | 0 | 3 | 0 | 10 | Normal | NEG | NEG | NEG |
| N°39 | Guinea (4) | 4 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 10 | Normal | NEG | NEG | NEG |
| N°40 | Nigeria (6) | 0 | 0 | 1 | 0 | 0 | 0 | 3 | 0 | 10 | Normal | NEG | NEG | NEG |
| N°41 | Algeria (2) | 4 | 0 | 1 | 0 | 0 | 0 | 3 | 0 | 10 | Normal | NEG | NEG | NEG |
| N°42 | Nigeria (6) | 0 | 0 | 1 | 0 | 0 | 0 | 3 | 0 | 10 | Normal | NEG | NEG | NEG |
| N°43 | Nigeria (6) | 0 | 0 | 0 | 0 | 1 | 0 | 3 | 0 | 10 | Normal | NEG | NEG | NEG |
| N°44 | Nigeria (6) | 0 | 0 | 1 | 0 | 0 | 0 | 3 | 0 | 10 | Normal | NEG | NEG | NEG |
| N°45 | Nigeria (6) | 0 | 0 | 1 | 0 | 0 | 0 | 3 | 0 | 10 | Normal | NEG | NEG | NEG |
| N°46 | France (0) | 0 | 2 | 1 | 1 | 0 | 0 | 3 | 3 | 10 | Normal | NEG | NEG | NEG |
| N°47 | Nigeria (6) | 0 | 0 | 1 | 0 | 0 | 0 | 3 | 0 | 10 | Normal | NEG | NEG | NEG |
Chest X-rays.
Real-time polymerase chain reaction (Xpert MTB/RIF) of Mycobacterium tuberculosis complex DNA.
Culture of Mycobacterium tuberculosis complex organisms.
ID, identity; Q0–Q8, question from 0 to 8; NEG, negative; ME, microscopic examination.
Details of 47 participants screening positive by questionnaire
Questionnaire scores ranged from 0 to 16 with an average [± Standard Deviation (SD)] of 4.9 (± 3.5). No significant differences were observed between patients having a score >10 and others, regarding sex, age, duration of stay in France for migrants, and health insurance coverage (Table 1).
Fifteen (of 16, 93.8%) hospitalised patients with biologically confirmed tuberculosis had a screening questionnaire score >10 (ranging from 11 to 19) (Table 4), one (patient TB°15) had a screening questionnaire score = 2.
| ID code | Year of study | Score | Total score | CXRa | CT scanner test | ME | qPCRb | Culturec | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Participant | Country of origin (Q0) | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | |||||||
| TB°1 | 2019 | Mongolia (8) | 4 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 15 | Lesion of caverns in two lung apex | Cavitary parenchymal lesions and a cavern of 43 and 33 mm in diameter in the left and right lung apex, respectively. | POS | POS | NEG |
| TB°2 | 2019 | Senegal (3) | 4 | 0 | 1 | 1 | 0 | 0 | 3 | 3 | 15 | Lesion of cavern in the right lung apex | A cavern of 70 × 58 × 31 mm in the superior lobe of right lung | POS | POS | NEG |
| TB°3 | 2019 | Mauritania (3) | 4 | 2 | 1 | 1 | 0 | 0 | 3 | 3 | 17 | Lesion of cavern in the right lung apex | A cavern in the right lung apex and disseminated micro nodules in the left lower-lung zone | POS | POS | NEG |
| TB°4 | 2019 | Morocco (3) | 4 | 2 | 0 | 1 | 0 | 0 | 3 | 0 | 13 | Lesion of cavern in the right lung apex, large right-sided pleural effusion | Cavitary parenchymal lesions, a cavern of 23 × 30 × 30 mm in superior lobe of right lung, large right-sided pleural effusion | POS | POS | NEG |
| TB°5 | 2018 | Algeria (2) | 4 | 0 | 1 | 1 | 0 | 0 | 3 | 0 | 11 | Lesion of cavern in the right lung apex | Cavitary parenchymal lesions, presence of a cavern in the superior lobe of right lung | NEG | POS | NEG |
| TB°6 | 2018 | Algeria (2) | 4 | 2 | 0 | 0 | 0 | 0 | 3 | 0 | 11 | Lesion of cavern in the right lung apex | Cavitary parenchymal lesions, presence of a cavern in the superior lobe of right lung | NEG | POS | NEG |
| TB°7 | 2018 | Romania (2) | 0 | 2 | 1 | 1 | 0 | 0 | 3 | 3 | 12 | Lesion of cavern in the right lung apex, large right-sided pleural effusion | Cavitary parenchymal lesions, presence of a cavern in the superior lobe of right lung, disseminated micro nodules in the right lower-lung zone, and large right-sided pleural effusion | POS | POS | NEG |
| TB°8 | 2018 | Algeria (2) | 0 | 2 | 1 | 1 | 0 | 0 | 3 | 3 | 12 | Lesion of cavern in the right lung apex | Cavitary parenchymal lesions, presence of a cavern in the superior lobe of right lung | POS | POS | POS |
| TB°9 | 2018 | Nigeria (6) | 4 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 13 | No feature consistent with pulmonary TB | No feature consistent with pulmonary TB | NEG | POS | NEG |
| TB°10 | 2018 | Algeria (2) | 4 | 2 | 1 | 1 | 0 | 0 | 3 | 0 | 13 | Acute lobar pneumonia in the right upper lobe | Alveolar condensation in the right upper lobe with cystic bronchiectasis | POS | POS | NEG |
| TB°11 | 2018 | Mauritania (3) | 4 | 2 | 1 | 1 | 0 | 0 | 3 | 0 | 14 | Rounded opacity in the inferior lobe of right lung. | Cavitary parenchymal lesions, a cavern of 35 × 40 × 40 mm in the inferior lobe of right lung, several peripheric micro nodules in the right lower-lung zone | POS | POS | NEG |
| TB°12 | 2018 | Armenia (6) | 4 | 0 | 0 | 0 | 1 | 0 | 3 | 0 | 14 | Lesions of caverns in two lung apex | Cavitary parenchymal lesions, two caverns in two lung apex, and bilateral hilar and mediastinal lymphadenopathy | NEG | POS | NEG |
| TB°13 | 2018 | Pakistan (5) | 4 | 2 | 0 | 1 | 0 | 0 | 3 | 0 | 15 | Lesions of cavern in the left lung apex | A cavern in the left lung apex, and hilar-mediastinal lymphadenopathy | POS | POS | NEG |
| TB°14 | 2018 | Armenia (6) | 4 | 2 | 0 | 1 | 1 | 0 | 3 | 0 | 17 | Lesion of caverns in two lung apex | Parenchymal condensation with multiple excavated lesions in two lung apex, and a cluster of small nodules within the apical segment of right lower lobe | NEG | POS | POS |
| TB°15 | 2017 | Algeria (2) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | Lesions of cavern in the left lung apex | Several caverns in the left lung apex | NEG | POS | POS |
| TB°16 | 2017 | Pakistan (5) | 4 | 2 | 1 | 1 | 0 | 0 | 3 | 3 | 19 | Lesions of cavern in the left lung apex and rounded opacity in the superior lobe of left lung | Several caverns in the apex and in the superior lobe of left lung | POS | POS | POS |
Chest X-rays.
Real-time polymerase chain reaction (Xpert MTB/RIF) of Mycobacterium tuberculosis complex DNA.
Culture of Mycobacterium tuberculosis complex organisms.
ID, identity; Q0–Q8, question from 0 to 8; POS, positive; NEG, negative; ME, microscopic examination.
Detail of 16 patients with biologically-confirmed active pulmonary tuberculosis with retrospective evaluation using the screening questionnaire
3.3. Imaging
Four screened participants (2.4%) had abnormal CXR features consistent with APTB (Table 5). Of the four, three underwent a CT scan and one was lost to follow-up. The CT scan was considered normal in two participants and revealed signs of bronchiolitis in the other (Table 5). Questionnaire scores ranged from 2 to 5 in these patients with abnormal radiographies.
| ID code | Score | Total score | CXRa | CT scannerb | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Participant | Country of origin (Q0) | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | |||
| N°1 | Algeria (2) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | Rounded opacity of the right lung apex | N/A |
| N°2 | France (0) | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | Well-circumscribed opacity of the left lung apex + micro nodule in the left mid lung zone | Bronchiolitis, CT scanner control in 3 months |
| N°3 | France (0) | 0 | 0 | 1 | 1 | 0 | 0 | 3 | 0 | 5 | Apical micronodular in two lungs | Normal |
| N°4 | France (0) | 4 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 5 | Apical micronodular in two lungs | Normal |
Chest X-rays.
Thoracic computed tomography scanner.
ID, identity; Q0–Q8, question from 0 to 8; N/A, not applicable.
Imaging results of four screened participants with abnormal CXR features consistent with APTB
Fifteen (of 16, 93.8%) hospitalised with biologically confirmed APTB had both CXR and CT scan features consistent with APTB (Table 4), one (patient TB°9) had no feature consistent with pulmonary TB on both CXR and CT scan.
3.4. Microbial Investigations
The results of the direct microscopic examination of sputum samples were negative for all screened participants. Fifty-one participants (including 47 with a positive questionnaire and four with abnormal CXRs) were tested with GeneXpert assays and no MTC-DNA was detected. All cultures were negative 6 weeks after recruitment in screened individuals. Hence, no case of APTB was diagnosed based on microbiological criteria in screened people.
Of 16 patients hospitalised with biologically confirmed APTB, 10 (62.5%) had positive direct microscopic examination, 16 (100%) had positive PCR, and four (25%) had positive culture testing (Table 4).
The sensitivity and specificity of the questionnaire for confirmed APTB were 93.8% (15/16) and 87.7% (336/383), respectively.
4. DISCUSSION
In our study, homeless people were characterised by a high proportion of migrants, a high proportion of smokers, and one third lacked health insurance coverage which is in line with previous surveys conducted in Marseille homeless shelters [3–5] and with surveys conducted in others European cities such as Frankfurt (Germany) [8] and Geneva (Switzerland) [6].
For migrants and refugees in reception or detention centres, crowded living conditions, poor environmental conditions (poor ventilation, lack of sufficient food) and lack of continuity of care (delayed diagnosis, interrupted or poor quality treatment) may increase their vulnerability to TB [9]. Our APTB screening strategy was designed in accordance with European recommendations [10] and French guidelines for the 2019–2023 period [2], promoting decentralisation and intersectional collaboration between regional tuberculosis control centres, acute care and follow-up care structures, medical biology laboratories and medical staff in shelters. The key strength of our study is the large population (>380 people) enrolled over a 1-year period. In spite of our efforts, no confirmed cases of active TB were diagnosed in the target population. In 2005, an APTB screening campaign was conducted among 221 homeless people in Marseille, using CXRs, and reported a 0.9% rate of infection [11]. During the 2013–2018 period, we conducted 1-day cross-sectional surveys among 617 sheltered homeless people, using various microbiological investigations (qPCR of sputum or stools, sputum culture), and found no cases of APTB [3]. These results are in line with the 0–2% APTB prevalence reported among homeless populations in western European countries during the 2000–2019 period [3,6,12]. As in our preliminary survey, conducted in 2018, we found a higher prevalence of participants with a positive screening result (9.2% and 12.2%, respectively) than in the study by Janssens et al. (4.1%). One major finding of our survey is a higher sensibility of screening questionnaire (93.8%) for confirmed ATPB when applicated for homeless persons in Marseille, as compared to previous study conducted on asylum individuals in Switzerland during the period 2007–2008 (55%, p = 0.008) [13].
Our study has several limitations. Notably, the population was not randomly and homogenously recruited. Only homeless people present in the shelters were enrolled on a voluntary basis leading to a 40% participation rate and we cannot exclude the possibility that those harbouring respiratory symptoms (cough, expectoration) might have been more likely to enrol in the survey, given that a medical examination was offered, while in the Janssens’s study, 87% of homeless people present in the shelter were enrolled [6].
We propose that medical staff in homeless shelters use screening questionnaires as a first assessment tool for each person arriving at the shelters and refer those screening positive to the regional tuberculosis control centres for a CXR. This strategy, which is cost-effective and easy to implement, may complete 1-day cross sectional CXR screening campaigns that are currently conducted twice a year in shelters.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
TD and PG contributed to the experimental design, data analysis, statistics, interpretation, and writing. TD, VT, TL, ML and NG administered questionnaires, examined patients, and collected samples. FH analysed the results of the chest X-rays. MD contributed to critically reviewing the manuscript and PG coordinated the work.
ACKNOWLEDGMENTS
No potential conflict of interest relevant to this study was reported. We thank the “Centre de lutte antituberculeuse à Marseille” and the “Oeuvre Antituberculeuse des Bouches-du-Rhône à Marseille” for their cooperation.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Tran Duc Anh Ly AU - Floriane Holi-Jamovski AU - Van Thuan Hoang AU - Ndiaw Goumballa AU - Meriem Louni AU - Thi Loi Dao AU - Michel Drancourt AU - Philippe Gautret PY - 2020 DA - 2020/10/15 TI - Screening Strategy of Active Pulmonary Tuberculosis in Sheltered Homeless People in Marseille, 2019 JO - Journal of Epidemiology and Global Health SP - 124 EP - 131 VL - 11 IS - 1 SN - 2210-6014 UR - https://doi.org/10.2991/jegh.k.201009.001 DO - 10.2991/jegh.k.201009.001 ID - Ly2020 ER -
