Healthcare-seeking behaviors for acute respiratory illness in two communities of Java, Indonesia: a cross-sectional survey
Joint first authors with equal contribution.
- DOI
- 10.1016/j.jegh.2016.01.002How to use a DOI?
- Keywords
- Healthcare-seeking behavior; Indonesia; Respiratory illness
- Abstract
Understanding healthcare-seeking patterns for respiratory illness can help improve estimations of disease burden and inform public health interventions to control acute respiratory disease in Indonesia. The objectives of this study were to describe healthcare-seeking behaviors for respiratory illnesses in one rural and one urban community in Western Java, and to explore the factors that affect care seeking. From February 8, 2012 to March 1, 2012, a survey was conducted in 2520 households in the East Jakarta and Bogor districts to identify reported recent respiratory illnesses, as well as all hospitalizations from the previous 12-month period. We found that 4% (10% of those less than 5 years) of people had respiratory disease resulting in a visit to a healthcare provider in the past 2 weeks; these episodes were most commonly treated at government (33%) or private (44%) clinics. Forty-five people (0.4% of those surveyed) had respiratory hospitalizations in the past year, and just over half of these (24/45, 53%) occurred at a public hospital. Public health programs targeting respiratory disease in this region should account for care at private hospitals and clinics, as well as illnesses that are treated at home, in order to capture the true burden of illness in these communities.
- Copyright
- Ministry of Health, Saudi Arabia, Production and hosting by Elsevier Ltd.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/)
1. Introduction
Acute respiratory infections are common in Indonesia, and can result in hospitalization and death, particularly among young children, older adults, and other high-risk groups [1–3]. Among Indonesian children up to 2 years of age, the incidence of pneumonia was reported as 21 cases per 100 child-years, with an acute respiratory infection-specific mortality rate of 33 per 1000 live births [4]. These findings are similar to other studies from Asia, where the incidence of lower respiratory tract infection in this age group has ranged from 10 per 100 child-years to 57 per 100 child-years of observation [5–7]. Although data are limited for older adults, researchers in other countries in the region and worldwide have reported that pneumonia is a significant contributor to mortality in this population [8–11]. Further, individuals of any age with underlying health conditions, such as chronic respiratory or cardiac disease, as well as pregnant women, are at an increased risk of severe illness from influenza viruses and other respiratory infections [12–15].
Acute respiratory illness can result from respiratory infections caused by a wide range of pathogens, which may vary by age group and time of year, as well as by other factors such as indoor and outdoor air pollution [16,17]. In Indonesia, attention has focused upon sporadic cases of severe respiratory illness caused by human infection with highly pathogenic avian influenza (HPAI) A (H5N1) virus [18,19]. For this rare zoonotic infection, Indonesia has reported both the highest number of confirmed human cases, and the highest case fatality proportion (83%, 167 deaths/199 confirmed cases), compared to a global case fatality proportion of 53% (449 deaths/844 confirmed cases since 2003) [20]. Possible explanations for this high case fatality include delay in diagnosis and treatment, low clinical suspicion for milder illnesses, and virus characteristics [21]. To date, however, seasonal influenza viruses and other respiratory pathogens have not received the same attention as HPAI A (H5N1) virus in Indonesia. Surveillance data suggest that seasonal influenza is an important public health problem in Indonesia, but influenza disease burden data are lacking [22].
Although the burden of respiratory illness among those seeking care at hospitals and clinics can be estimated through health facility-based surveillance, this methodology will underestimate disease burden, as not all sick individuals seek care at these facilities. In order to understand the impact of disease at the community level, it is important to understand the healthcare-seeking behaviors for respiratory illness. Healthcare utilization surveys (HUS) that ask individuals about where they seek care for acute respiratory illness, and also assess obstacles to and delays in care-seeking, have been conducted in a number of countries [23–30]. In Indonesia, a diverse country of more than 249 million people and 17,000 islands, divided into 34 provinces [31,32], there is a wide variety of healthcare options. These include government and private hospitals, government clinics (puskesmas), private doctors, pharmacies, and traditional healers (dukuns). Factors associated with healthcare-seeking behaviors include age and socioeconomic status, access to different facilities, and perceived severity of illness [33,34]. Understanding healthcare-seeking behaviors for respiratory illness can help improve estimations of disease burden as well as public health interventions to control respiratory disease in Indonesia.
The objective of this study was to describe healthcare-seeking behaviors for respiratory illnesses in two communities located in the western part of the main island of Java, Indonesia, and to explore the factors that affect care seeking. The two sites were selected to provide both urban (East Jakarta) and rural (Bogor) representation.
2. Materials and methods
2.1. Study population and survey design
This cross-sectional study was conducted in two areas: East Jakarta Municipality of Jakarta Capital City (DKI Jakarta) and Bogor District in West Java (Fig. 1). East Jakarta represents an urban area with a population density of 14,304 people/km2 [35], and is one of six districts that make up DKI Jakarta. Bogor District represents a rural area with a population density of 1621 people/km2 [36]. It is one of the 26 districts in West Java province.
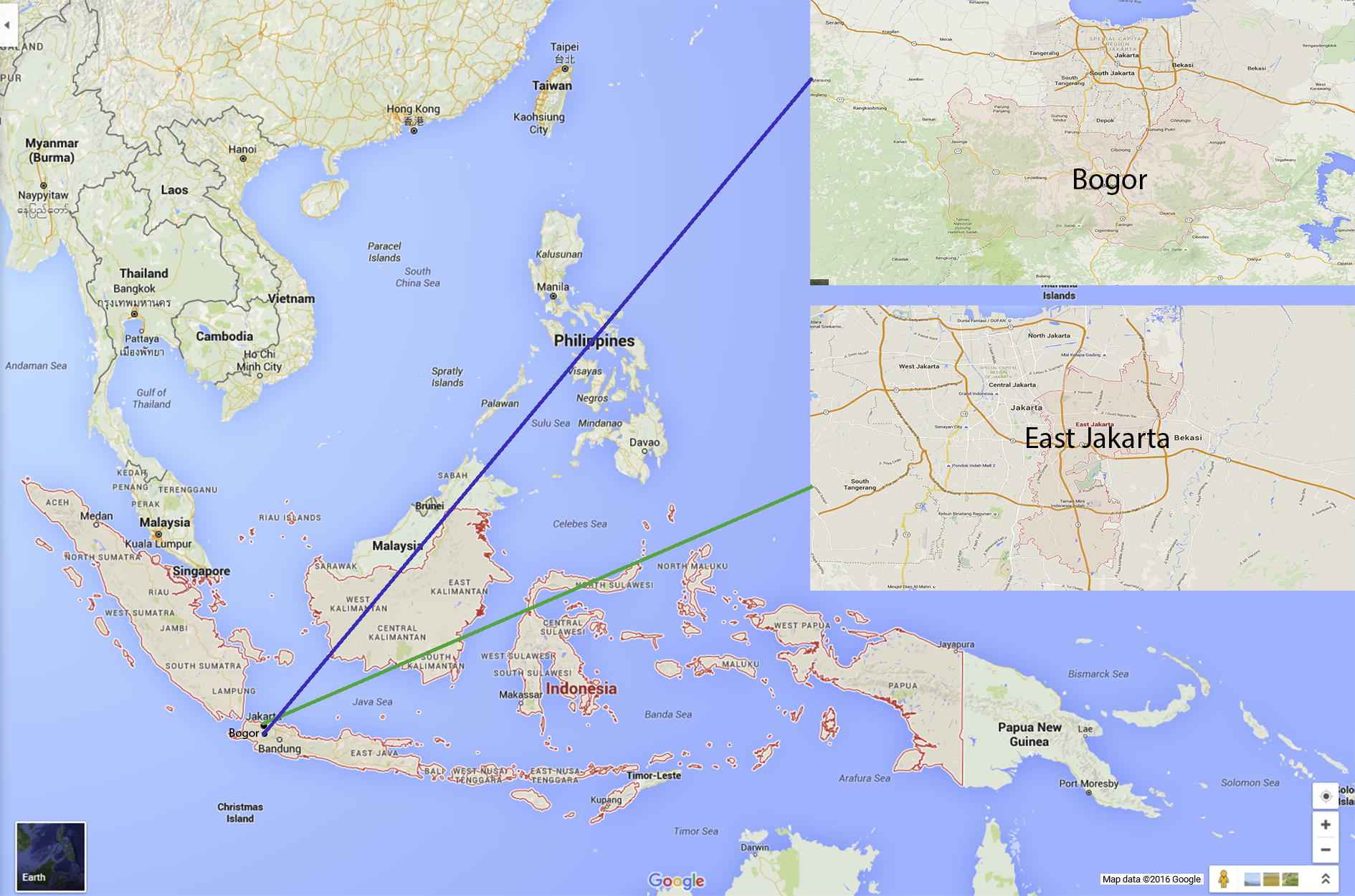
Map of two study sites, West Java, Indonesia.
Households were selected for enrollment through a multistage design (Fig. 2). First, seven subdistricts were selected from East Jakarta because of their proximity to active influenza surveillance activities, and seven subdistricts were selected from Bogor District through a probability proportionate to size method. In each selected subdistrict, nine neighborhood clusters were chosen using the same probability proportionate to size method. Finally, 20 households were selected per cluster using simple random sampling, for a total of 1260 households (7 subdistricts × 9 clusters × 20 households) per district, and 2520 households overall. If an adult household member was not available or did not consent to participate, the nearest household was contacted for recruitment into the study. This sample size was designed to capture all-age respiratory hospitalizations for each district within the past 12 months.
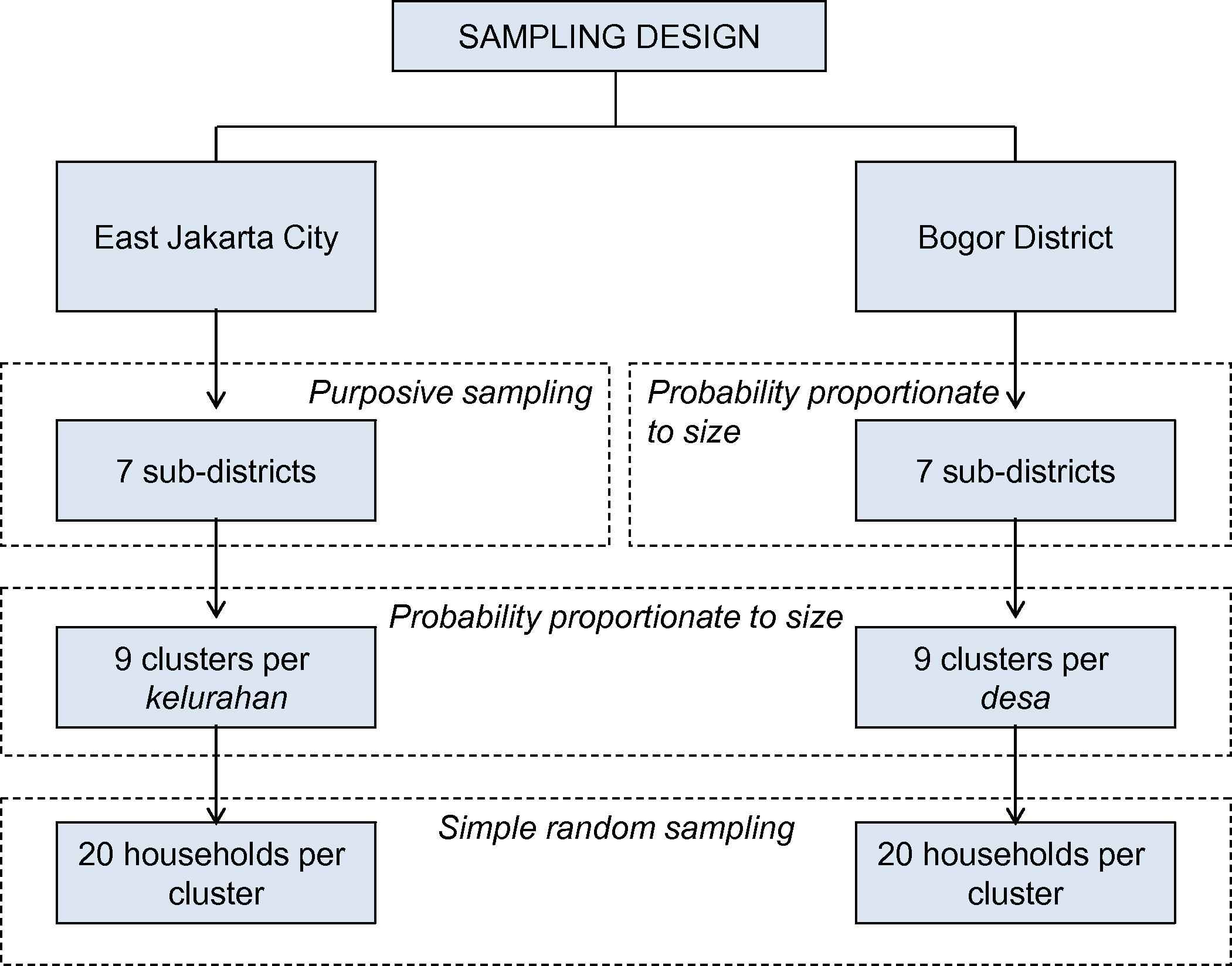
Flow chart of study sampling design, by district.
2.2. Data collection and analysis
For each enrolled household, the adult member who self-identified as the most knowledgeable about the health conditions of household members was interviewed. Face-to-face interviews were conducted in each household by trained interviewers using a structured questionnaire in the Indonesian language (Bahasa Indonesia) or local language (Bahasa Sunda). Key data collected included demographic details on all household members, as well as recent medically attended acute illnesses (over the previous 2 weeks) and hospitalizations (over the previous 12 months). Additionally, respondents were asked about general care-seeking behavior and barriers to seeking care for mild and severe acute respiratory illnesses.
Survey data were reviewed for completeness and double entered into EpiData version 3.1 (EpiData Association, Odense, Denmark), and data analysis was performed using IBM SPSS Statistics 19 (IBM Co., Somers, NY, USA). District-level population-normalized weights, based on the sampling design used, were calculated and used for all analyses; results reported are the weighted estimates (both counts and percentages). Recent illnesses were classified as respiratory based on a report of one or more acute respiratory symptoms: cough, sore throat, runny nose, nasal congestion, chest pain while breathing, difficulty breathing, shortness of breath, or a physician diagnosis as pneumonia/respiratory infection. Recent respiratory illnesses were classified as severe if they reported cough or sore throat as well as difficulty breathing, shortness of breath, or chest pain while breathing. Hospitalizations were also classified as respiratory if they included any of the symptoms listed above. Respiratory hospitalizations that included chronic lung disease/tuberculosis were classified as chronic, while all other respiratory hospitalizations were considered acute. Statistical comparisons were performed by Chi-square and Mann–Whitney U (2-sample median) tests. Human participant review for the study was conducted and approved by the Ethics Committee of the Faculty of Public Health, Universitas Indonesia, Depok, West Java, Indonesia, with additional approval by the Centers for Disease Control and Prevention Institutional Review Board, Atlanta, GA, USA.
3. Results
From February 8, 2012 to March 1, 2012, individuals from 2520 households were interviewed, 1260 households per district. These households included 11,326 residents: 5533 in East Jakarta and 5793 in Bogor. Twelve percent of households recruited for the study declined to participate; refusal was higher in East Jakarta than Bogor (19% vs. 4%). Survey respondents were most commonly the spouse of the head of household; respondents were slightly younger in East Jakarta than in Bogor (median of 38 years vs. 45 years, p < 0.001; Table 1). East Jakarta households had higher levels of education than those in Bogor, with 32% reporting at least one individual attending academy/university as compared to 12% of households in Bogor (p < 0.001). Travel time to nearest health facilities was significantly shorter in East Jakarta (p < 0.001), except for dukuns, which had the shortest median travel time of any facility at 5–7 min. Hospitals were the facility type with the longest median travel time (15 min in East Jakarta and 30 min in Bogor). Approximately half of all households reported someone who had been diagnosed with an underlying chronic health condition. The most frequently reported chronic health conditions included asthma, diabetes, and stroke or cerebrovascular accident. Asthma was the most common diagnosis in Bogor (8% of households) and diabetes was the most common diagnosis in East Jakarta (9% of households).
| East Jakarta District | Bogor District | p | |
|---|---|---|---|
| District total population | 2,687,027 | 1,349,533 | |
| Individuals by age group (y) | |||
| 0–4 | 459 (8) | 574 (10) | <0.001 |
| 5–17 | 1193 (22) | 1644 (28) | |
| 18–64 | 3587 (65) | 3374 (58) | |
| ⩾65 | 294 (5) | 201 (4) | |
| Male | 2716 (49) | 2972 (51) | 0.02 |
| Median (IQR) time to nearest facility (min) | |||
| Hospital | 15 (10–30) | 30 (20–60) | <0.001 |
| Puskesmas | 10 (5–15) | 15 (10–20) | <0.001 |
| Private | 5 (5–10) | 10 (5–15) | <0.001 |
| Dukun | 5 (5–10) | 7 (5–15) | 0.6 |
| Someone in household has been diagnosed with an underlying health condition | 601 (48) | 608 (48) | 0.8 |
| Asthma | 63 (5) | 103 (8) | 0.002 |
| Diabetes | 115 (9) | 38 (3) | <0.001 |
| Stroke/cerebrovascular accident | 71 (6) | 28 (2) | <0.001 |
| Other | 503 (40) | 525 (42) | 0.4 |
| Someone in household is currently on treatment for an underlying health condition | 333 (27) | 228 (18) | 0.4 |
| Asthma | 39 (3) | 38 (3) | 1.0 |
| Diabetes | 87 (7) | 27 (2) | <0.001 |
| Stroke/cerebrovascular accident | 52 (4) | 13 (1) | <0.001 |
| Other | 243 (19) | 180 (14) | <0.001 |
| Highest education completed in household | |||
| None | 15 (1) | 64 (5) | <0.001 |
| Primary | 131 (10) | 604 (48) | |
| High school | 708 (56) | 440 (35) | |
| Academy/University | 402 (32) | 153 (12) | |
| Median (IQR) total household size | 4 (3–5) | 4 (4–6) | <0.001 |
| Children | 1 (0 –2) | 2 (1–3) | <0.001 |
| Adults | 3 (2–4) | 2 (2–4) | 0.003 |
| Elderly | 0 (0–0) | 0 (0 –0) | 0.003 |
| Median (IQR) age of survey respondent | 38 (31–48) | 45 (35–55) | <0.001 |
| Relationship of respondent to head of household | |||
| Self | 383 (25) | 310 (30) | <0.001 |
| Spouse | 751 (68) | 860 (60) | |
| Child | 87 (5) | 69 (7) | |
| Other | 39 (2) | 19 (3) | |
Data are presented as n (%) unless otherwise specified, all data reported in the table are weighted estimates.
IQR = interquartile range.
Denominator for household level questions is 1260 for each district; denominator for resident level questions is 5533 for East Jakarta and 5793 for Bogor. The p-values are Chi-square for categorical variables or Mann–Whitney U for median values. Other health conditions include chronic lung disease, heart disease, tuberculosis, cancer, chronic kidney disease, chronic liver disease, seizures/neurological disorders. Elderly is defined as age ⩾65 years; 80% of households in East Jakarta and 86% of households in Bogor did not have any individuals in this age group.
Description of study households, by district.a
Within the 2 weeks prior to the survey, 403 individuals (4%) from 365 households (14% of households) had seen a healthcare provider for an episode of acute respiratory illness, and 40 (10%) of these episodes were classified as severe (Table 2). Illnesses among those aged ⩾65 years were more frequently severe than those in younger age groups (7/23 episodes, or 30%, among those ⩾65 years vs. 33/380 episodes, 9%, among those <65 years). Children younger than 5 years were more likely to have recent illnesses with respiratory symptoms, as compared to other age groups combined (p < 0.001). Government and private clinics were the most commonly reported providers for all respiratory episodes, including severe illness, among all age groups.
| <5 years | 5–17 years | 18–64 years | ⩾65 years | Total | |
|---|---|---|---|---|---|
| Total individuals surveyed | 1033 | 2837 | 6961 | 495 | 11,326 |
| Individuals with a respiratory episode | 101 (10) | 113 (4) | 166 (2) | 23 (5) | 403 (4) |
| Public hospital | 6 | 7 | 8 | 3 | 24 |
| Private hospital | 7 | 5 | 13 | 3 | 28 |
| Government clinic | 33 | 51 | 45 | 5 | 134 |
| Private clinic | 35 | 51 | 84 | 8 | 178 |
| Other | 22 | 6 | 17 | 3 | 48 |
| Individuals with a severe respiratory episode | 5 (0.5) | 9 (0.3) | 19 (0.3) | 7 (1) | 40 (0.4) |
| Public hospital | 3 | 0 | 2 | 2 | 7 |
| Private hospital | 0 | 0 | 4 | 3 | 7 |
| Government clinic | 2 | 5 | 7 | 2 | 16 |
| Private clinic | 1 | 6 | 9 | 0 | 16 |
| Other | 2 | 0 | 2 | 1 | 5 |
Data are presented as n or n (%). All data reported in the table are weighted estimates.
Three individuals reported more than one respiratory episode in the previous 2-week period, but these were collapsed for the analysis. Multiple locations for care-seeking allowed for each illness episode. Hospital visit for recent illness could include outpatient and/or inpatient services. Other includes pharmacy, traditional healer, health posts, and other providers.
Reported acute respiratory illnesses in the previous 2 weeks resulting in a visit to a healthcare provider, by age group.a
In the previous 12 months, 362 individuals [3%, 95% confidence interval (CI) 3–4%] had a reported hospitalization, although this percentage was higher among adults aged ⩾65 years (Table 3). Overall, respiratory hospitalizations accounted for 45 of 382 (12%) admissions, although its relative contribution to total hospitalizations was highest among extremes of age (23% of admissions among children aged <18 years and 18% of admissions among adults ⩾65 years). The majority of all-cause (238/362, 62%) admissions were to private hospitals, while respiratory hospitalizations were more frequently admitted to public hospitals (24/45, 53%). East Jakarta residents were more likely than Bogor residents to use a public facility: 47% of reported all-cause admissions in East Jakarta were to public hospitals vs. 24% of all-cause admissions in Bogor (p < 0.001), with similar district-level trends for respiratory admissions. Sixty percent of individuals (95% CI: 55–65%) sought medical care before hospitalization, with median time from onset to admission of 2 days for all-cause admissions and 3 days for respiratory admissions, and no difference in this time to care-seeking by education level. The median length of stay was 4 days for both all-cause and respiratory hospitalizations.
| <5 years | 5–17 years | 18–64 years | ⩾65 years | Total | |
|---|---|---|---|---|---|
| Total individuals surveyed | 1033 | 2837 | 6961 | 495 | 11,326 |
| Total individuals hospitalized | 47 (5) | 48 (2) | 229 (3) | 38 (8) | 362 (3) |
| Total all-cause hospitalizations | 48 | 48 | 246 | 40 | 382 |
| Admitted at public hospital | 19 | 23 | 90 | 12 | 144 |
| Admitted at private hospital | 29 | 25 | 156 | 28 | 238 |
| Sought care before hospitalization | 33 | 33 | 141 | 24 | 231 |
| Median time from onset to admission (d) | 2 | 3 | 2 | 1 | 2 |
| Median length of stay (d) | 3 | 6 | 4 | 6 | 4 |
| Respiratory hospitalizations | 11 (1)a | 7 (0.2) | 20 (0.3) | 7 (1) | 45 (0.4) |
| Admitted at public hospital | 4 | 4 | 12 | 4 | 24 |
| Admitted at private hospital | 7 | 3 | 8 | 3 | 21 |
| Sought care before hospitalization | 9 | 2 | 17 | 5 | 33 |
| Median time from onset to admission (d) | 3 | 2 | 7 | 0 | 3 |
| Median length of stay (d) | 4 | 3 | 7 | 5 | 4 |
Data are presented as n or n (%). All data reported in the table are weighted estimates.
Percent of total individuals; although there were individuals with more than one all-cause hospitalization during the 12-month period, there were no individuals with more than one respiratory hospitalization during this window.
Reported all-cause and respiratory hospitalizations in the previous 12 months, by age group.
When asked about general healthcare seeking behavior for mild respiratory illnesses, 39% of households sought care at a health facility, 30% received only home care, and 31% obtained medicine from a pharmacy or shop for self-treatment. Among households who used health facilities, 87% sought care at a primary health center, while 13% went immediately to hospital (5% of all households). Households in East Jakarta that used health facilities were more likely than those in Bogor to do so within the first 2 days of illness (84% vs. 60%, respectively, p < 0.001), with quality of medicines and accessibility listed as the most common factors influencing health facility selection. Reasons for not seeking care most commonly included not feeling sick enough or improving without any treatment.
Almost half (47%) of households reported that they treated severe respiratory illnesses at home, with 24% receiving only home care, and an additional 23% obtaining medicine from pharmacy or shop. An equal percentage (47%) sought care at a health facility: 37% at a health clinic, 10% at a hospital, and the remaining 6% sought care elsewhere, such as a traditional healer. There were no differences in care-seeking by education level, either overall or by district. Among those seeking care, quality and cost of medicines were the most common factors in health facility selection. Reasons for deciding not to go to hospital include perceived lower severity of illness or a preference to manage severe illness at home, with or without treatment from pharmacy, or to visit a government or private clinic.
4. Discussion
In the two communities surveyed, illnesses were prevalent during the survey period, with 14% of households reporting recent respiratory illness requiring a visit to any healthcare provider during the prior two weeks. Respiratory hospitalizations, however, were not common, with <1% of individuals having been hospitalized for respiratory causes in the past year. Instead, many reported respiratory illnesses were managed through self-treatment at home or at an outpatient clinic. Among those that were admitted to hospital, private facilities were more commonly used and time of onset to time of admission was typically short (⩽3 days). East Jakarta residents were twice as likely to be admitted to a government-based hospital (vs. a private hospital) as Bogor residents. Among those seeking care at hospitals, cost and quality of care were listed as key factors in facility selection. Despite the relatively short time from onset to admission, the majority of individuals sought care at outpatient clinics before hospitalization.
These findings highlight the variety of healthcare options available in this part of Indonesia, and suggest that over half of patients with severe acute respiratory illness in these communities are not seen at a formal health facility, and instead receive care at home, pharmacy, or traditional healer. This is consistent with the findings of the Indonesian National Socioeconomic Survey, which show that only a small proportion of the population was hospitalized in the past 12 months (2.9% nationwide and 3.2% in Jakarta) [33]. Among those who are admitted to hospital, however, the short median time from onset to admission and high care seeking before hospitalization suggest that although hospitalization for respiratory illness was uncommon among the study population, those that did seek care did so relatively quickly.
The higher proportion of hospitalizations at public facilities among East Jakarta residents vs. Bogor residents highlights additional variability in care seeking by district that may be driven by multiple factors, including socioeconomic status (SES), access and distance to different care options, as well as cost and patient-perceived quality of treatment. While we did not collect household indicators of wealth, the significantly higher education level of East Jakarta households compared to Bogor households may be a proxy of higher SES in this community. Clinical criteria for admission of a patient may also vary between public and private hospitals. Data from the National Socioeconomic Survey show that across Indonesia, the volume of patients hospitalized in public hospitals is almost equal to that in private hospitals [33], although this survey did not account for variability in care-seeking at the district level. One important issue related to care-seeking patterns in these communities and throughout Indonesia is the recent policy of Universal Health Coverage, or Jaminan Kesehatan Nasional [37]. This policy, which took effect in 2014, ensures that both public and private healthcare services are available to individuals who need them free of charge, and encourages early care seeking at Puskesmas-level clinics.
These results are consistent with a recent study of healthcare-seeking among confirmed human cases of HPAI A (H5N1) virus infection in Indonesia, which identified no delay in care-seeking among the study population [21], although our questions on respiratory illness were not limited to any specific respiratory pathogen. Our findings are also consistent with HUS surveys in Kenya and Guatemala, which found that a large fraction of clinically defined pneumonia cases did not result in hospitalization [23,27,29]. In Guatemala, in contrast to the current findings, the majority of hospitalizations were at government hospitals [29]. In contrast to the current findings, an HUS conducted in Thailand during 2002–2003 found that 80% of all reported pneumonia cases sought some form of care at a hospital [25]. These differences may be due to population-level disparities in access to care at hospitals between these settings, and highlight the need for local data to understand healthcare seeking patterns.
There are several limitations to this study. Although these findings describe both urban and rural households, they are only from communities in Western Java during a time of year when respiratory viruses are most prevalent, and therefore may not be representative of other regions in Indonesia or of annual averages for recent respiratory illness. Although the sampling strategy was designed to obtain a representative sample of the study areas, there may be some differences between the households that agreed to participate and those that refused, such as socioeconomic status or other factors. Also, the sampling approach was slightly different in the two districts, limiting our ability to conduct a more robust cluster survey analysis, which may have more accurately depicted the uncertainty around each of the estimates and reduced the significance of some of the district-level differences. Further, all data on illness and care-seeking behavior, including illness severity, were based on self-report, rather than on medical records. Data were also collected from only one respondent per household, and are subject to participants’ knowledge of and ability to recall the relevant information. Interviewers sought primary caregivers within a household to improve knowledge of others’ illnesses, and timeframes for any respiratory illness were limited to 2 weeks prior to the HUS interview in order to minimize the potential for reduced recall. While hospitalizations were considered a major event and therefore more easily recalled over a longer period, some of the details related to hospitalizations, such as admission dates and reasons for hospitalization, may not have been recalled. Additionally, although the impact of respiratory illness is most pronounced among the extremes of age, small sample sizes for some analyses limit our power in assessing these patterns.
5. Conclusions
Public health programs targeting respiratory disease in Indonesia (particularly in Western Java) should account for care beyond that which is received at public hospitals and puskesmas, since many sick individuals seek care at private facilities, or receive informal treatment at home, with important differences by age group. Research efforts to describe the epidemiological and economic impact of influenza viruses and other causes of acute respiratory illness of public health importance should also include care sought at private facilities and nonmedically attended disease, in order to capture the true burden of illness in these communities. To provide further context for these findings, etiological studies should be conducted to identify respiratory pathogens responsible for treatable or vaccine-preventable severe acute respiratory disease in this region. This information could then be used to help guide prevention and control activities.
Conflicts of interest
All authors declare no conflicts of interest. The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Acknowledgments
The authors would like to thank Yudarini and colleagues at the Center for Health Research, Universitas Indonesia for their contributions in data collection and study coordination, and Kendra Chittenden for her contributions to the study design and implementation. This work was supported by the United States Agency for International Development, under the auspices of the Strategies Against Flu Emergence (SAFE) project, managed by Development Associates International (DAI).
References
Cite this article
TY - JOUR AU - Catharina Y. Praptiningsih AU - Kathryn E. Lafond AU - Yunita Wahyuningrum AU - Aaron D. Storms AU - Amalya Mangiri AU - Angela D. Iuliano AU - Gina Samaan AU - Christiana R. Titaley AU - Fitra Yelda AU - Jennifer Kreslake AU - Douglas Storey AU - Timothy M. Uyeki PY - 2016 DA - 2016/03/10 TI - Healthcare-seeking behaviors for acute respiratory illness in two communities of Java, Indonesia: a cross-sectional survey JO - Journal of Epidemiology and Global Health SP - 77 EP - 86 VL - 6 IS - 2 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2016.01.002 DO - 10.1016/j.jegh.2016.01.002 ID - Praptiningsih2016 ER -
