Skin diseases in patients with primary psychiatric conditions: A hospital based study
- DOI
- 10.1016/j.jegh.2013.03.005How to use a DOI?
- Keywords
- Infectious; Parasitic skin diseases; Psychiatric; Psychocutaneous; Skin diseases
- Abstract
Background: Although the relationship between skin diseases in patients with primary psychiatric conditions is important for patient management, studies on this issue are limited.
Objective: To detect the frequency and type of cutaneous disorders among patients with primary psychiatric conditions.
Subjects and methods: This analytic cross-sectional study was conducted on a total of 400 subjects – 200 patients with primary psychiatric disorders and 200 age and sex matched individuals free from primary psychiatric disorders. Patients included in the study were diagnosed according to The Diagnostic and Statistical Manual of Mental Disorders (DMS IV) Criteria. A specially designed questionnaire including socio-demographic data, medical history, family history and dermatological examination was applied. The data were statistically analyzed.
Results: There was a significant statistical increase in the prevalence of skin diseases in general and infectious skin diseases in particular in psychiatric patients compared with non-psychiatric patients (71.5% versus 22%, P < 0.001) and (48% versus 11%, P < 0.001), respectively. Parasitic infestations (42.7%) were the most common infectious skin diseases in psychiatric patients (P < 0.001). Infectious skin diseases in psychiatric patients were seen most in patients diagnosed with schizophrenia (83.6%) and least in obsessive compulsive disorders (30%)(P < 0.001). Psychogenic skin disorders were found in 8.4% of psychiatric patients with skin diseases; delusional parasitosis was the most common (50%).
Conclusion: Health education of psychiatric patients and/or of their caregiver and periodic monthly inspection of psychiatric patients are highly indicated for the prevention and control of infectious skin diseases in primary psychiatric patients.
- Copyright
- © 2013 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- Open access under CC BY-NC-ND license. http://creativecommons.org/licenses/by-nc-nd/4.0/
1. Introduction
It is important to consider the consequences of the interrelation between skin disorders and psychiatric condition. Psychiatric disorders are any pattern of psychological or behavioral symptoms that cause an individual significant distress impairing their ability to function in life and/or significantly increase their risk of death, pain, disability or loss of freedom. Psychiatric disorders are also known as psychiatric condition or mental illness [1]. Some primary psychiatric disorders may be expressed in the skin, such as delusional parasitosis [2]. The influence of psychological factors on skin diseases is fairly common, although it is not much studied and debated. Dermatology holds a distinct position in psychosomatic medicine because it deals with an organ that can be readily seen and touched [3].
The psychological state of a patient can produce manifestations in the skin. Stress has been found to contribute to the severity of chronic inflammatory dermatosis, like psoriasis, atopic dermatitis, and acne [4]. Stress and psychological disturbances are accompanied by reduced natural killer cell cytotoxicity, suppressed lymphocyte proliferative responses and blunted humoral responses to immunization [5].
Psychiatric patients often have a defensive need to deny their psychopathology and seek dermatological care for their prominent cutaneous symptoms [6]. It has been estimated that the effective management of at least one third of the patients in dermatological departments depends, to some extent, upon the recognition of the emotional factor. However, there is very little published data on the incidence of dermatoses in patients with a primary psychiatric condition [7].
The aim of this work is to detect the frequency and type of cutaneous disorders among patients with primary psychiatric conditions.
2. Subjects and methods
2.1. Technical design
A hospital-based analytic cross-sectional study was conducted over a period of five months (October 2010–February 2011) on a total of 400 subjects (200 patients with primary psychiatric disorders and 200 individuals apparently free from psychiatric disorders, age and sex matched). Sample size was calculated by using the Epi Info version 6 statistical program, taking into consideration the prevalence of psychiatric disorders among patients with skin diseases to be about 30% [8] at 95% confidence level and power of 80%.
2.1.1. Sampling technique
2.1.1.1. Selection of psychiatric patients
Patients included in the study were those suffering from primary psychiatric disorders according to a psychiatric consultation. Patients were obtained from the outpatient clinics of the Psychiatric Department at Al-Zahraa University Hospital, Cairo, Egypt, which is a general multidepartment hospital, and Abbassia Mental Hospital, Cairo, Egypt, which is a psychiatric and mental hospital. The outpatient service is offered three days per week by Al-Zahraa University Hospital and daily at Abbassia Mental Hospital (public hospital). Al-Zahraa Psychiatric Department Outpatient Clinic serves on average about 15 new patients and 30 old patients per day for follow-up, while Abbassia Mental Hospital serves on average about 30 new patients and 40 old patients per day for follow-up which serves all types of psychiatric diseases. These hospitals serve a large population of low and mid-class psychosocial composition, near the center of the capital, and Abbassia Mental Hospital is considered the largest mental hospital in Egypt.
A fixed day out of the three days of the outpatient psychiatric clinic at Al-Zahraa University Hospital was chosen randomly. Also, for Abbassia Mental Hospital Outpatient Clinic, a fixed day was chosen randomly out of the six days of the week. All of the patients fulfilling inclusion criteria were selected for a total of 200 outpatients.
2.1.2. Inclusion criteria for psychiatric patients: Patients with primary psychiatric disorders
- •
Aged between 18 and 50 years old.
2.1.3. Exclusion criteria for patients with psychiatric disorders
- •
Any patient not fulfilling the previous inclusion criteria.
- •
Patient with secondary psychiatric disorders.
- •
Patients with any systemic disorders associated with these chronic diseases, such as diabetes mellitus, liver and renal diseases in order to exclude cutaneous manifestations of them.
- •
Patients on long-term bed rest.
2.1.3.1. Selection of subjects free from psychiatric disorders
Individuals not suffering from psychiatric disorders were recruited from those accompanying the patients. Also, they were recruited from individuals accompanying patients of other outpatient clinics of Al-Zahraa University Hospital. After explaining the purpose of the study to the psychiatric patients or their relatives and psychiatric disease-free individuals, verbal consents were taken.
2.1.4. Inclusion criteria for controls are
- •
Individuals free from psychiatric disorders according to psychiatric consultation.
- •
Age, sex and social class matched to patient’s group.
2.1.5. Exclusion criteria for controls are
- •
Individuals with any systemic disease, such as diabetes mellitus, liver and renal diseases.
- •
Relatives of psychiatric patients.
2.1.6. All participants were subjected to
- 1-
Psychiatric consultation by a psychiatrist using The Diagnostic and Statistical Manual of Mental Disorders (DMS IV) Criteria that describes the symptoms for all mental disorders and the criteria that must be met to receive a diagnosis of each disorder [9] or exclude psychiatric disease in healthy controls after taking a medical history of psychiatric disease of each patient regarding type, duration of disease, type of medication and duration and type of antipsychotic drug intake.
- 2-
A specially designed questionnaire including items about socio-demographic data: age, sex, origin, residence, marital status, smoking and special habits, education, occupation and social class. Assessment of social class of the subject was estimated according to the modified Fahmy and El-Sherbini [10] scoring system.
- 3-
Dermatological examination: A complete dermatological examination was carried out by three independent highly qualified dermatologists, and special investigations were done when needed (e.g. scrapping for fungus, biopsy.). A consensus was done if there was any discrepancy or doubtful diagnosis.
- 4-
General clinical examinations and investigations to exclude systemic diseases were done (complete blood count, liver and renal function tests, fasting and post-prandial blood glucose, etc.). Hormonal assessment was done for suspicious patients.
2.2. Statistical design
Data collected were reviewed and coded. The numerical codes were fed into the computer where statistical analysis was done using the statistical package of social science version 13 (SPSS 13.0) (SPSS Inc., Chicago, Illinois, USA). Data were expressed as mean ± standard deviation for continuous numerical data or number and percentage for discrete data. Student’s t test was used to compare between two groups for quantitative parametric data and the Chi-square test was used to compare between percentages. The level of significance was taken at P value of ⩽0.05.
2.3. Administrative design
Formal permissions from the authorities of both hospitals were obtained after clarifications of the aim of the study. The study was approved by the Research Ethics Committee of Faculty of Medicine for Girls, Al-Azhar University.
3. Results
The total number of subjects was 400–200 patients with primary psychiatric disorders, 78 males and 122 females, with mean age of 33.04 ± 8.67 years; and 200 patients free from primary psychiatric disorders (controls), 70 males and 130 females with mean age of 33.09 ± 7.90 years. The number of subjects collected from Abassia Hospital was 101 (50.5%) patients and 100 (50%) controls. Subjects collected from Al-Zahraa University Hospital were 99 (49.5%) patients and 100 (50%) controls. The social class showed no statistically significant difference between both groups (P = 0.1).
The primary psychiatric disorders in the studied group are shown in Table 1. A significantly higher percentage of primary psychiatric patients with skin diseases (143 patients [71.5%]) than the number of non-psychiatric controls with skin diseases (44 patients [22%]) was found (P < 0.001) (Table 2).
| Psychiatric diseases | Total no. = 200 | Male no. = 78 | Female no. = 122 | ||
|---|---|---|---|---|---|
| No. | (%) | No. | (%) | ||
| Schizophrenia | 76 | 21 | 26.9 | 55 | 45.1 |
| Depression | 67 | 33 | 42.3 | 34 | 27.9 |
| Anxiety | 15 | 8 | 10.3 | 7 | 5.7 |
| Mood disorders | 25 | 11 | 14.1 | 14 | 11.5 |
| Obsessive compulsive | 17 | 5 | 6.4 | 12 | 9.8 |
Primary psychiatric disorders in the studied group.
| Dermatological patients | Patients with primary psychiatric disorders (no. = 143) | Patients free from psychiatric disorders (no. = 44) | Significance test | P value | ||
|---|---|---|---|---|---|---|
| Skin diseases | No. | % | No. | % | ||
| Infectious | 96 | 66.9 | 22 | 50 | X2 = 4.24 | 0.04* |
| Non-infectious | 47 | 33.1 | 22 | 50 | ||
P value <0.05 → significant.
Infectious and non-infectious skin diseases among dermatological patients of both studied groups.
The number of psychiatric patients with infectious skin diseases was 96 patients (48% of all psychiatric patients and 66.9% of psychiatric patients with skin diseases). The number of non-psychiatric controls with infectious skin diseases was 22 patients (11% of all non-psychiatric patients and 50% of non-psychiatric patients with skin diseases). The infectious skin diseases are significantly higher (P < 0.001) in patients with primary psychiatric disorders than from patients free from psychiatric disorders (Table 3). Patterns of all skin diseases in both groups are shown in Table 4.
| Patients with infectious skin disease | Patients with primary psychiatric disorders (no. = 96) | Patients free from psychiatric disorders (no. = 22) | Significance test | P value | ||
|---|---|---|---|---|---|---|
| Skin disease | No. | % | No. | % | ||
| Parasitic | 41 | 42.7 | 0 | 0 | X2 = 13.6 | <0.001* |
| Fungal | 36 | 37.5 | 15 | 68.2 | ||
| Bacterial | 10 | 10.4 | 5 | 22.7 | ||
| Viral | 9 | 9.4 | 2 | 9.1 | ||
P value <0.05 → significant.
Types of infectious skin diseases among both studied groups.
| Skin diseases | Patients with primary psychiatric disorders | Subjects free from psychiatric disorders | ||
|---|---|---|---|---|
| No. | % | No. | % | |
| Parasitic | (N = 41) | (N = 0) | 0 | |
| Pediculosis capitis | 26 | 63.4 | 0 | 0 |
| Scabies | 15 | 36.6 | 0 | 0 |
| Viral | (N = 9) | (N = 2) | ||
| Verruca vulgaris | 8 | 88.9 | 2 | 100 |
| Herpes simplex labialis | 1 | 11.1 | 0 | 0 |
| Fungal | (N = 36) | (N = 15) | ||
| Pityriasis versicolor | 14 | 38.9 | 8 | 53.3 |
| Tinea pedis | 15 | 41.7 | 7 | 46.7 |
| Tinea circinata | 6 | 16.7 | 0 | 0 |
| Candidal intertrigo | 1 | 2.7 | 0 | 0 |
| Bacterial | (N = 10) | (N = 5) | ||
| Acne vulgaris | 8 | 80 | 4 | 80 |
| Pyogenic infections (boils) | 2 | 20 | 1 | 20 |
| Psychogenic | (N = 12) | (N = 0) | ||
| Delusion of parasitosis | 6 | 50 | 0 | 0 |
| Trichotillomania | 3 | 25 | 0 | 0 |
| Neurotic excoriation | 3 | 25 | 0 | 0 |
| Non infectious | (N = 35) | (N = 22) | ||
| Diffuse hair loss | 24 | 68.6 | 12 | 54.6 |
| Itching | 6 | 17.14 | 1 | 4.5 |
| Eczema | 2 | 5.7 | 1 | 4.5 |
| Psoriasis | 2 | 5.7 | 2 | 9 |
| Post inflammatory hyperpigmentation | 5 | 14.3 | 6 | 27.4 |
| Freckles | 2 | 5.7 | 2 | 9 |
| Skin tags | 2 | 5.7 | 1 | 4.5 |
Pattern of skin diseases among dermatological patients of both studied groups.
Schizophrenic patients with skin diseases were 61/76 (80.2%); 83.6% of them had infectious skin diseases. Patients with depression with skin diseases were 44/67 (65.6%); 59% of them had infectious skin diseases. Patients with anxiety with skin diseases were 12/15 (80%); 50% of them had infectious skin diseases. Patients with mood disorders with skin diseases were 16/25 (64%); 62.5% of them had infectious skin diseases. Patients with obsessive compulsive disorders with skin diseases were 10/17 (59%); 30% of them had infectious skin diseases (Fig. 1). The frequency of infectious versus non-infectious skin diseases in different psychiatric disorders was significant (P < 0.001).
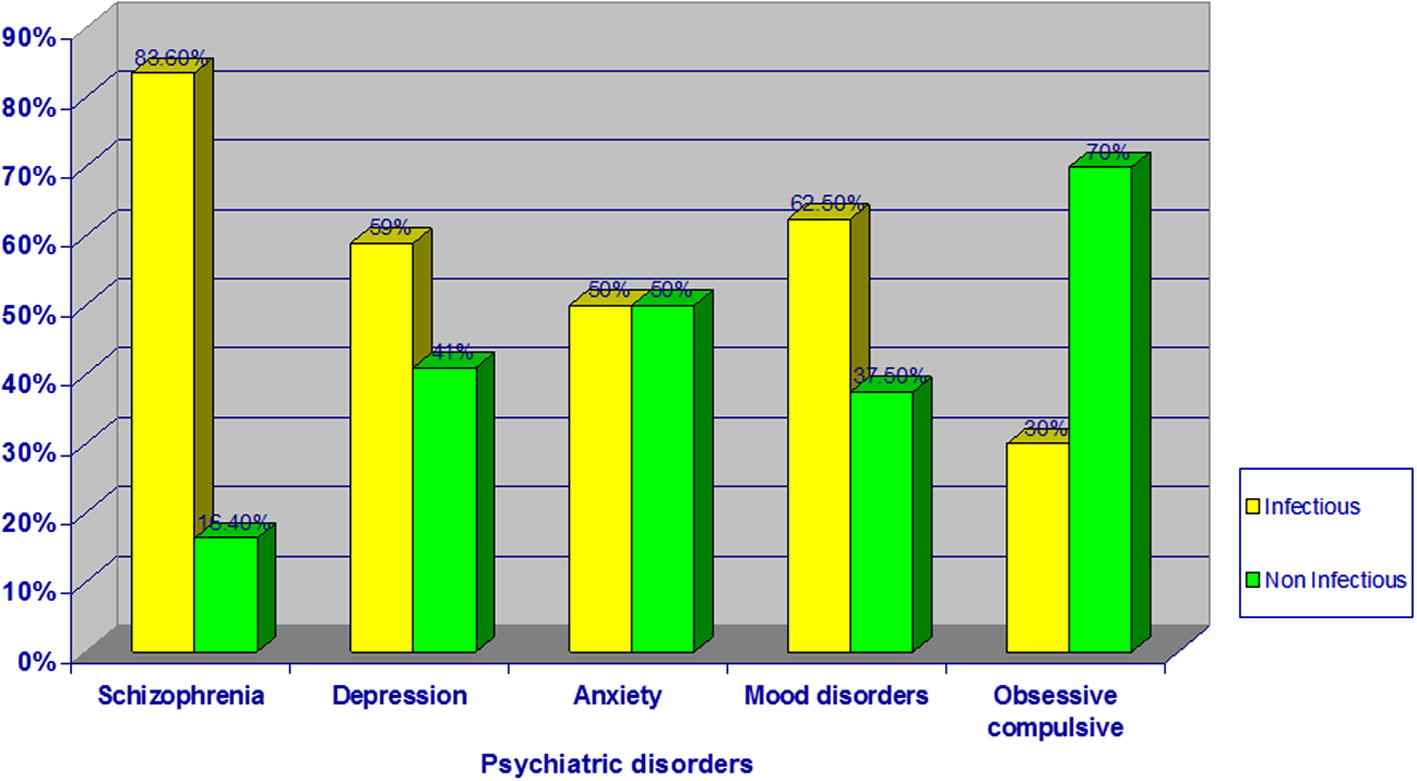
Frequency of infectious versus non-infectious skin diseases in relation to psychiatric disorders among psychiatric patients.
The number of female psychiatric patients was 122/200; 97 of them had skin diseases. Infectious skin diseases affected 60.8% of the 97 patients. The number of male psychiatric patients was 78/200; 46 of them had skin diseases. Infectious skin diseases affected 80.4% of the 46 patients (Table 5). Infectious skin diseases were significantly more in low social class of primary psychiatric patients (74.5%) compared with high social class (50%) (P = 0.01).
| Skin diseases sex | Infectious | Non infectious | Total no. = 143 | Significance test | P value | |||
|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |||
| Females | 59 | 60.8 | 38 | 39.2 | 97 | 79.5 | X2 = 5.44 | 0.01* |
| Males | 37 | 80.4 | 9 | 19.6 | 46 | 58.9 | ||
P value <0.05 → significant.
Frequency of infectious versus non-infectious skin diseases in relation to sex in patients with primary psychiatric disorders.
4. Discussion
The present study sample of patients was chosen on a certain single day per week in each hospital. Accordingly, this is a pseudo-randomized study. However, selection bias of patients did not exist as every day, similarly, showed various types of psychiatric diseases and all the patients of the day fulfilling inclusion criteria are included in the study. Controls were recruited from those accompanying the patients, and from individuals accompanying the patients of other outpatient clinics of Al-Zahraa University Hospital so as to be of the same social class as the patients. Relatives of psychiatric patients were excluded to avoid genetic susceptibility of skin diseases.
In the present study, a clear positive relation was detected between psychiatric disorders and the presence of skin diseases, as skin diseases were detected in 71.5% of psychiatric patients and in only 22% of non-psychiatric controls with significant difference. This is in agreement with Mookhoek, et al. [11] who found that skin diseases were more common in psychiatric patients (77%). However, a later study was undertaken on inpatients and not excluding patients with systemic diseases, such as diabetes mellitus, in contrast to the present study. This study was performed using psychiatric outpatients. Patients with systemic diseases such as diabetes, liver and renal diseases were excluded in the current study to eliminate the possibility that the cutaneous diseases were associated with the systemic diseases rather than with the psychiatric disorders.
The current study showed that infectious skin diseases were more common in psychiatric patients (66.9%) than in non-psychiatric controls (50%) with significant difference, which is reflected as an increase in the percentage of skin diseases in psychiatric patients as a whole. This is in accordance with Kuruvila, et al. [7] who examined 300 psychiatric patients and 300 non-psychiatric healthy controls and found that the prevalence of infectious skin diseases in psychiatric patients was higher (68.7%) compared with non-psychiatric healthy controls (56.6%). Segerstrom and Miller [12] reported that psychiatric disorders and chronic stress in adults are consistently associated with decreased natural killer (NK) cell cytotoxicity and decreased lymphocyte proliferation leading to increased susceptibility to infectious skin diseases. The most common types of infectious skin diseases in psychiatric patients in the current study was parasitic infestations, followed by fungal, then bacterial, and lastly viral infections. This was in contrast with non-psychiatric controls in which fungal infections were the commonest type followed by bacterial then viral infections with a significant difference between psychiatric and non-psychiatric controls. In the current study, it was found that the most common parasitic infestations in psychiatric patients were pediculosis capitis and scabies, respectively, in comparison with non-psychiatric patients in whom the parasitic infestations were absent. This is in agreement with another study by Chosidow [13] who found that scabies and pediculosis are highly contagious diseases with scabies affecting immunocompromised individuals or patients in mental hospitals.
Most infectious skin diseases in psychiatric patients, in this study, were seen in patients with schizophrenia (83.6%), then mood disorders (62.5%), and depression (59%). However, less infectious skin diseases were seen in patients with obsessive compulsive disorders (30%) and anxiety (50%). The high prevalence of skin infections in schizophrenic patients may be due to negligence of hygiene [14]. Schizophrenic patients were unable to carry out their normal daily activities or were unable to work, in addition to a poor level of personal awareness regarding personal hygiene and overall cleanliness [15]. Depression is one of the mood disorders that is characterized by loss of interest, lack of energy, low self-esteem and difficulty in experiencing pleasure, social problems and irritability which interfere with physical activity leading to lack of personal care which in turn increases the susceptibility to infection [16]. However, in obsessive compulsive patients, if compulsions include an irresistible urge to wash (particularly the hands) or clean, the patients frequently wash the hands and clean themselves [17], in turn making them less susceptible to infections; 4063 people with obsessive–compulsive disorder were studied. Among them, none (0.00%) had skin bacterial infections [18].
In the current study, it was found that the prevalence of infectious skin diseases was higher in males (80.4%) than in females (60.8%), with significant difference. This may be attributed to smoking, alcohol and drug abuse, which are more common in males, thereby leading to decreased immunity and increasing the susceptibility to infections. Men are much more likely to be addicted to alcohol and other substances than women. Alcohol has been shown to suppress selected functions of the immune system, thereby compromising host defenses against bacterial infections. It has an adverse effect on killer cells, which are important in the body’s defense system, and suppresses the B cells, which form antibodies [19]. In the present study, it was impossible to get data from the patients or their relatives about alcohol and drug abuse since it is prohibited in the country, and most people deny addiction. Thirty-two of the 37 male patients with skin infections were smokers. Cigarette smoking has an immunosuppressant effect. It includes both morphologic changes (atrophy of lymphoid tissue) and cell functional disorder of the immune system. Cell-mediated response Th1-type, which is responsible for pathogen invasion, is depleted, whereas Th2-type is increased and has its effect on higher frequency of allergic diseases [20].
In the current study, the prevalence of infectious skin diseases in psychiatric patients of very low social class was much higher than in the high social class, and these results were statistically significant. This is in accordance with Heinrich et al. [21] who reported that the prevalence of infectious skin diseases is higher in low social class than in high social class, and this is quite expected because persons belonging to the low social class stay more frequently in polluted and/or an overcrowded environment with poor water supply and lack of personal hygiene than those belonging to the high social class. In addition, proper healthcare and healthy nutrition are more available to the high social class than to the low social class.
5. Conclusion
Infectious skin diseases are the most common skin disease categories in psychiatric patients. Although psychogenic skin disorders occur exclusively in primary psychiatric disorder patients, it is much less frequent than the infectious skin diseases overall.
Accordingly, it is recommended that health education with a focus on special hygiene measures be made available to psychiatric patients and their caregivers for prevention and control of infections, and periodic monthly inspections of psychiatric patients should be carried out for early detection of any infectious skin diseases.
References
Cite this article
TY - JOUR AU - Nayera H. Moftah AU - Abeer M. Kamel AU - Hussein M. Attia AU - Mona Z. El-Baz AU - Hala M. Abd El–Moty PY - 2013 DA - 2013/05/09 TI - Skin diseases in patients with primary psychiatric conditions: A hospital based study JO - Journal of Epidemiology and Global Health SP - 131 EP - 138 VL - 3 IS - 3 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2013.03.005 DO - 10.1016/j.jegh.2013.03.005 ID - Moftah2013 ER -
