Outcomes of Guillain–Barré Syndrome Patients Admitted to Intensive Care Unit in Tertiary Care Hospital
- DOI
- 10.2991/dsahmj.k.191004.001How to use a DOI?
- Keywords
- Guillain–Barré syndrome; mortality; plasmapheresis
- Abstract
Despite the availability of plasmapheresis and intravenous immunoglobulin, the mortality and long-term morbidity from Guillain–Barré Syndrome (GBS) remains significant. This study aimed to determine the short-term outcomes in patients with GBS admitted to an intensive care unit. A total of 27 patients with a mean age of 31.67 ± 15.88 years were prospectively followed for 4 weeks after admission. Overall muscle power was graded using Medical Research Council (MRC) score 0–5, GBS disability was graded according to the Hughes scale, and tendon reflexes and features of dysautonomia were also noted. Plasma and cerebrospinal fluid biochemical parameters were analysed. Plasmapheresis sessions were done in all except one patient. Seven patients (26%) who died during follow-up showed a significantly higher proportion of dysautonomia features compared to those who survived. However, muscle power and plasma and cerebrospinal fluid biochemical features were similar between the two groups. Increasing age was associated with poor outcome [Unadjusted odds ratio (OR) 0.9270, 95% confidence interval (CI) 0.8598–0.9995, p = 0.027]. Plasmapheresis had no impact on the improvement of overall MRC score. Platelet count reduced significantly with plasmapheresis sessions (p = 0.014). Survival rate of patients decreased with prolonged preceding illness, hospital stay, and duration of mechanical ventilation >10 days. Only three patients were capable of independent survival at the end of 4 weeks’ follow-up. Plasmapheresis-only treatment does not improve overall MRC score in the short term in patients presenting with low MRC score.
- Copyright
- © 2019 Dr. Sulaiman Al Habib Medical Group. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Guillain–Barré Syndrome (GBS) is an immune-mediated acute inflammatory demyelinating polyneuropathy. It is the most common acute flaccid paralysis disorder manifesting as ascending motor weakness [1,2]. Worldwide reported incidence is one or two cases per 100,000, with a male preponderance [3]. In most but not all cases, onset of GBS is associated with preceding viral (cytomegalovirus or Epstein–Barr virus) or bacterial (Campylobacter jejuni or Mycoplasma pneumoniae) infections [4]. Among the known electrophysiological variants, acute motor axonal neuropathy is commonly reported in Asian countries [5–7] including Pakistan [8].
Various clinical, aetiological, electrophysiological, and immunological factors contribute to the prognosis of GBS both in adult [9] and paediatric [10] populations. Despite improvement in treatment, the mortality and long-term morbidity from GBS remain significant and have not changed in the past decade [11]. Among the known long-term predictors of poor prognosis, the most common include old age, previous diarrhoea, disability and weakness at admission, short interval between onset of symptoms and admission, mechanical ventilation, and absent or weak compound muscle action potentials [12].
Predictors of short-term outcome in GBS vary; some authors reporting absence of previous infections and lower Medical Research Council (MRC) score at presentation as predictors of poor prognosis in mechanically ventilated patients [13]; while others reporting old age and lower MRC score at nadir as risk factors for poor short-term prognosis [9]. However, this was studied in patients requiring mechanical ventilation [13] or in elderly age groups with severe GBS [9]. Other studies involved a cohort of patients whose mean MRC score was >30 and hence carried a better chance of resuming optimal muscle power over the treatment period [14]. Studies looking at the short-term outcome of disease with lower MRC score and its impact on mortality are therefore needed. Plasma exchange is generally offered in five sessions [15]. Whether plasmapheresis in patients presenting with lower mean MRC score improves overall muscle power is not known. Furthermore, the effect of lower MRC score at presentation, duration of mechanical ventilation, duration of hospital stay, and number of plasmapheresis sessions on mortality in the short term needs to be investigated. This study was aimed at determining the short-term outcomes in patients with GBS admitted to an intensive care unit of Khyber Teaching Hospital, Peshawar Pakistan.
2. MATERIALS AND METHODS
A prospective longitudinal study was conducted between January and December 2015 in the Intensive Care Unit, Khyber Teaching Hospital, Peshawar, Pakistan. Twenty-seven patients with GBS, age >15 years were recruited. National Institute of Neurological Communicative Disorders and Stroke (NINCDS) criteria were used to diagnose GBS [16]. Patients with hypo or hyperkalaemic paralysis, poliomyelitis, diabetic neuropathy, and history of potential toxic exposure were excluded.
Before being recruited, written informed consent was obtained from each patient or their relatives. The study protocol was approved by the Hospital Review Board (Ref. No. 25-8/05/19). History of respiratory tract infections, diarrhoea, recent surgery, or vaccination was obtained. Complete clinical nervous system assessment was done for all patients. Muscle power was assessed using summary scores for muscle power of six bilateral muscles in arms and legs according to the MRC scale from 0 to 5 [17]. Tendon reflexes were graded as absent, reduced, normal, or brisk. In addition, patients were also assessed for dysautonomia. GBS disability score was graded as 0–6 according to the Hughes scale [18]. Complete blood count, random blood glucose, blood urea nitrogen, serum electrolytes, creatinine, alanine aminotransferase, platelet count, prothrombin time, electrocardiogram, and chest radiograph were taken for each patient. Nerve conduction study was performed in all patients for whom it was logistically feasible. Cerebrospinal Fluid (CSF) examination was done in all patients.
Plasmapheresis was done for patients presenting within 14 days after the onset of illness. Fresh frozen plasma (1 L) was used as replacement fluid. Patients who were unable to maintain partial pressure of O2 > 60 mmHg and developing hypercarbia (partial pressure of CO2 > 50 mmHg) or abnormal pH on arterial blood gas analysis were mechanically ventilated [19]. Outcome at 4 weeks was categorized as (1) complete (independent for activities of daily living); (2) partial (needing help for activity of daily living); or (3) poor (bedridden or wheelchair bound) [20]. Death during this period and the causes of death were noted.
2.1. Statistical Analysis
Minitab version 17 (State College, PA, USA) was used for data analysis. Categorical variables were expressed as frequency and percentage, while numerical data were presented as mean and standard deviation. Two-sample t-test was used to determine differences in biochemical parameters between the outcome (alive versus dead) by the end of follow-up. The χ2 test or Fisher’s exact test was used to compare categorical variables. One-way analysis of variance was applied to determine the difference in biochemical parameters between different plasmapheresis sessions. Binary logistic regression (Unadjusted OR) was applied to estimate the association of disease outcome with different parameters. Kaplan–Meier curves were plotted to estimate percentage survival of patients, and the effect of preceding illness, duration of hospital stay, duration of mechanical ventilation, and number of plasmapheresis sessions.
3. RESULTS
Mean age of all participants was 31.67 ± 15.88 years, with no significant difference between women (n = 9, 29.11 ± 12.90 years) and men (n = 18, 32.94 ± 17.39 years) (p = 0.526). Except for serum alanine aminotransferase (male; 50.5 ± 35 IU versus female; 24.85 ± 9.89 IU, p = 0.011), no significant difference was found in any of the biochemical parameters, muscle power, and CSF between male and female patients.
During 4 weeks’ follow-up, seven (26%) patients died. Significant differences were found in the frequency of signs and symptoms at the time of presentation such as the presence of arrhythmia (p = 0.009), labile blood pressure (p = 0.0315), and increased sweating (p = 0.004) between those who were alive versus those who died during this period (Table 1). At presentation, prior nerve conduction studies were performed in only 10 patients who were reported to have motor axonal (n = 7), axonal (n = 1), or mixed (n = 2) neuropathies. A significantly higher percentage of patients who died during follow-up required mechanical ventilation compared to those who survived (p = 0.015). Ventilator-associated pneumonia was found in seven patients. Culture and sensitivity aspirate (cultured for 48 h) yielded growth of Pseudomonas aeruginosa in four aspirates (three samples from patients who were alive at the end of follow-up and one from the patient who died). Of those who survived (n = 17), only three (17.6%) patients could live independently at the end of follow-up.
| Parameter | Alive (n = 20) | Died (n = 7) | p | ||
|---|---|---|---|---|---|
| No | Yes | No | Yes | ||
| Preceding diarrhoea | 6 (46.15) | 7 (53.85) | 2 (50) | 2 (50) | 0.893 |
| Preceding respiratory disease | 7 (43.75) | 9 (56.25) | 2 (40) | 3 (60) | 0.882 |
| Neck flexion | 12 (75) | 4 (25) | 2 (50) | 2 (50) | 0.344 |
| Respiratory muscle involvement | 15 (83.33) | 3 (16.67) | 3 (50) | 3 (50) | 0.102 |
| Bulbar/cranial nerve involvement | 16 (80) | 4 (20) | 4 (57.14) | 3 (42.86) | 0.249 |
| Tachy/bradyarrhythmia | 18 (100) | 0 (0) | 3 (50) | 3 (50) | 0.009 |
| Labile blood pressure | 16 (100) | 2 (10) | 2 (50) | 2 (50) | 0.032 |
| Increased sweating | 19 (95) | 1 (5) | 3 (42.86) | 4 (57.14) | 0.004 |
| Urinary retention/incontinence | 14 (100) | 0 (0) | 5 (83.33) | 1 (16.67) | 0.300 |
| Mechanical ventilation required | 13 (72.22) | 5 (27.78) | 1 (16.67) | 5 (83.33) | 0.015 |
| CMV mode ventilator used | 5 (25) | 15 (75) | 5 (75) | 2 (25) | NC |
| SIMV mode ventilator used | 5 (25) | 15 (75) | 2 (25) | 5 (75) | NC |
| Tracheostomy needed | 4 (50) | 4 (50) | 2 (33.33) | 4 (66.667) | 0.531 |
| Ventilator associated pneumonia | 1 (20) | 4 (80) | 1 (25) | 3 (75) | NC |
CMV, continuous mechanical ventilation; NC, not calculable; SIMV, spontaneous intermittent mechanical ventilation.
Clinical features of Gullain–Barré syndrome patients who were alive at the end of 4 weeks’ follow-up versus those who died
Blood pressure, number of plasmapheresis sessions, duration of mechanical ventilation, haematological parameters, and parameters of CSF were not significantly different between those who were alive until the end of follow-up versus those who died in this period (Table 2).
| Variable | All patients (n = 27) | Alive (n = 20) | Died (n = 7) | p | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Age (years) | 31.67 | 15.88 | 28.40 | 14.03 | 41.00 | 18.25 | 0.135 |
| Duration of illness before admission (days) | 5.222 | 4.635 | 4.85 | 4.58 | 6.29 | 4.99 | 0.520 |
| Heart rate (per min) | 95.48 | 15.72 | 96.6 | 17.81 | 92.67 | 9.35 | 0.519 |
| Systolic blood pressure (mmHg) | 125.87 | 22.19 | 121.88 | 14.24 | 135.0 | 34.0 | 0.363 |
| Diastolic blood pressure (mmHg) | 77.39 | 12.87 | 75.00 | 10.95 | 82.86 | 16.04 | 0.271 |
| Plasmapheresis total sessions (n) | 3.769 | 1.142 | 3.895 | 0.875 | 3.429 | 1.718 | 0.515 |
| Ventilation required on day | 2.455 | 2.252 | 1.800 | 0.837 | 3.00 | 2.97 | 0.387 |
| Duration on CMV mode (days) | 19.22 | 18.03 | 16.20 | 18.09 | 23.00 | 19.92 | 0.615 |
| Duration on SIMV mode (days) | 25.7 | 26.0 | 18.00 | 20.15 | 64.000 | * | NC |
| Total duration on MV (days) | 33.8 | 42.1 | 25.20 | 19.56 | 48.0 | 70.3 | 0.638 |
| Hospital stay (days) | 15.13 | 11.63 | 15.56 | 10.10 | 14.57 | 14.19 | 0.880 |
| Power of muscles – MRC score | |||||||
| Deltoid – right | 1.852 | 1.262 | 2.000 | 1.170 | 1.429 | 1.512 | 0.390 |
| Deltoid – left | 1.778 | 1.251 | 1.900 | 1.165 | 1.429 | 1.512 | 0.474 |
| Biceps – right | 2.037 | 1.224 | 2.150 | 1.040 | 1.714 | 1.704 | 0.545 |
| Biceps – left | 2.000 | 1.271 | 2.050 | 1.099 | 1.857 | 1.773 | 0.795 |
| Wrist extensors – right | 1.815 | 1.111 | 2.000 | 1.076 | 1.286 | 1.113 | 0.171 |
| Wrist extensors – left | 1.815 | 1.145 | 1.950 | 1.099 | 1.429 | 1.272 | 0.360 |
| Illeopsoas – right | 1.222 | 0.974 | 1.350 | 0.998 | 0.857 | 0.900 | 0.250 |
| Illeopsoas – left | 1.148 | 0.949 | 1.250 | 1.250 | 0.857 | 0.900 | 0.351 |
| Quadricep femoris – right | 1.222 | 0.892 | 1.300 | 0.923 | 1.000 | 0.816 | 0.436 |
| Quadricep femoris – left | 1.148 | 0.949 | 1.200 | 1.005 | 1.000 | 0.816 | 0.610 |
| Tibialis anterior – right | 1.296 | 0.869 | 1.300 | 0.979 | 1.286 | 0.488 | 0.961 |
| Tibialis anterior – left | 1.296 | 0.823 | 1.300 | 0.923 | 1.286 | 0.488 | 0.959 |
| Total MRC score | 18.59 | 10.32 | 19.70 | 9.740 | 15.43 | 12.04 | 0.422 |
| Biochemical parameters | |||||||
| Haemoglobin (g/dL) | 13.49 | 2.396 | 13.38 | 2.502 | 13.829 | 2.207 | 0.664 |
| Total leukocyte count | 20368 | 36891 | 16291 | 23829 | 32015 | 62334 | 0.539 |
| Platelet count | 219762 | 95022 | 212781 | 92014 | 237714 | 107731 | 0.602 |
| PT – patient | 16.60 | 3.440 | 16.556 | 3.854 | 16.714 | 2.289 | 0.901 |
| PT – control | 13.36 | 0.907 | 13.278 | 1.018 | 13.571 | 0.535 | 0.360 |
| APTT – patient | 33.72 | 7.88 | 32.17 | 5.93 | 37.71 | 11.07 | 0.249 |
| APTT – control | 30.52 | 3.177 | 30.00 | 2.951 | 31.86 | 3.58 | 0.253 |
| RBS (mg/dL) | 140.2 | 64.1 | 145.9 | 68.8 | 120.8 | 44.9 | 0.314 |
| Na+ (mmol/L) | 137.67 | 3.32 | 137.6 | 2.74 | 137.86 | 4.88 | 0.898 |
| K+ (mmol/L) | 3.990 | 0.373 | 4.001 | 0.353 | 3.957 | 0.454 | 0.822 |
| SGPT/ALT (IU) | 42.31 | 31.55 | 37.46 | 24.39 | 57.7 | 47.6 | 0.363 |
| CSF R/E – cell count | 5.864 | 3.895 | 5.47 | 3.125 | 7.20 | 6.14 | 0.577 |
| CSF R/E – lymphocytes (%) | 83.75 | 33.47 | 80.63 | 36.82 | 96.25 | 7.50 | 0.134 |
| CSF R/E – protein (mg/100 mL) | 96.16 | 40.97 | 94.39 | 37.51 | 102.2 | 55.9 | 0.781 |
| CSF R/E – calcium | 8.617 | 1.002 | 8.511 | 0.930 | 8.933 | 1.232 | 0.467 |
| CSF R/E – albumin | 4.073 | 0.798 | 4.032 | 0.804 | 4.186 | 0.834 | 0.682 |
Duration on SIMV mode (days) is constant for died patients.
APTT, activated partial thromboplastin time; CSF R/E, cerebrospinal fluid routine examination; MRC, Medical Research Council; NC, not calculable; PT, prothrombin time; RBS, random blood sugar; SD, standard deviation; SGPT/ALT, serum glutamate phosphotransferase/alanine aminotransferase; CMV, continuous mechanical ventilation; SIMV, spontaneous intermittent mechanical ventilation.
Clinical and biochemical parameters of participants who were alive at the end of follow-up versus those who died during the study period
Binary logistic regression analysis showed a significant association of age with disease outcome (death considered as an event) (Unadjusted OR 0.9270, 95% CI 0.8598–0.9995, p = 0.027) and a tendency toward total MRC score (Unadjusted OR 1.0931, 95% CI 0.9783–1.2214, p = 0.086) (Table 3).
| Parameter | R2(%) | Unadjusted OR (95% CI) | p |
|---|---|---|---|
| Age | 9.65 | 1.0508 (0.9891–1.1164) | 0.027 |
| Total MRC score | 3.11 | 0.9583 (0.8789–1.0449) | 0.086 |
| Diastolic BP | 6.01 | 1.0478 (0.9739–1.1273) | 0.198 |
| Systolic BP | 5.42 | 1.0260 (0.9834–1.0704) | 0.222 |
| Haemoglobin (mg/dL) | 0.39 | 1.0654 (0.7449–1.5239) | 0.730 |
| Total leukocyte count | 2.79 | 1.0000 (1.0000–1.0000) | 0.358 |
| Platelet count | 1.42 | 1.0000 (1.0000–1.0000) | 0.521 |
| RBS | 4.60 | 0.9893 (0.9683–1.0108) | 0.260 |
| Serum Na+ | 0.05 | 1.0160 (0.7813–1.3211) | 0.906 |
| Serum K+ | 0.54 | 0.6138 (0.0569–6.6219) | 0.687 |
| ALT/SGPT | 5.77 | 1.0178 (0.9892–1.0472) | 0.212 |
| CSF cell count | 4.24 | 1.1329 (0.8836–1.4524) | 0.323 |
| CSF lymphocytes | 4.28 | 1.0227 (0.9594–1.0903) | 0.360 |
| CSF protein | 0.65 | 1.0049 (0.9802–1.0302) | 0.699 |
| CSF calcium | 2.62 | 1.5113 (0.5544–4.1198) | 0.405 |
| CSF albumin | 0.46 | 1.2315 (0.4059–3.7366) | 0.712 |
ALT/SGPT, alanine aminotransferase/serum glutamate phosphotransferase; BP, blood pressure; CI, confidence interval; CSF, cerebrospinal fluid; MRC, Medical Research Council; OR, odds ratio; RBS, random blood sugar.
Binary logistic regression analysis for the association of outcome of disease with blood pressure, total MRC score, and plasma and CSF parameters
Plasmapheresis sessions (n = 1–4) were done for all except one patient. Total MRC score remained similar throughout all these sessions (Figure 1). Compared to baseline measurements, significant differences were observed only in platelet count (p = 0.014) (Table 4 and Figure 2).
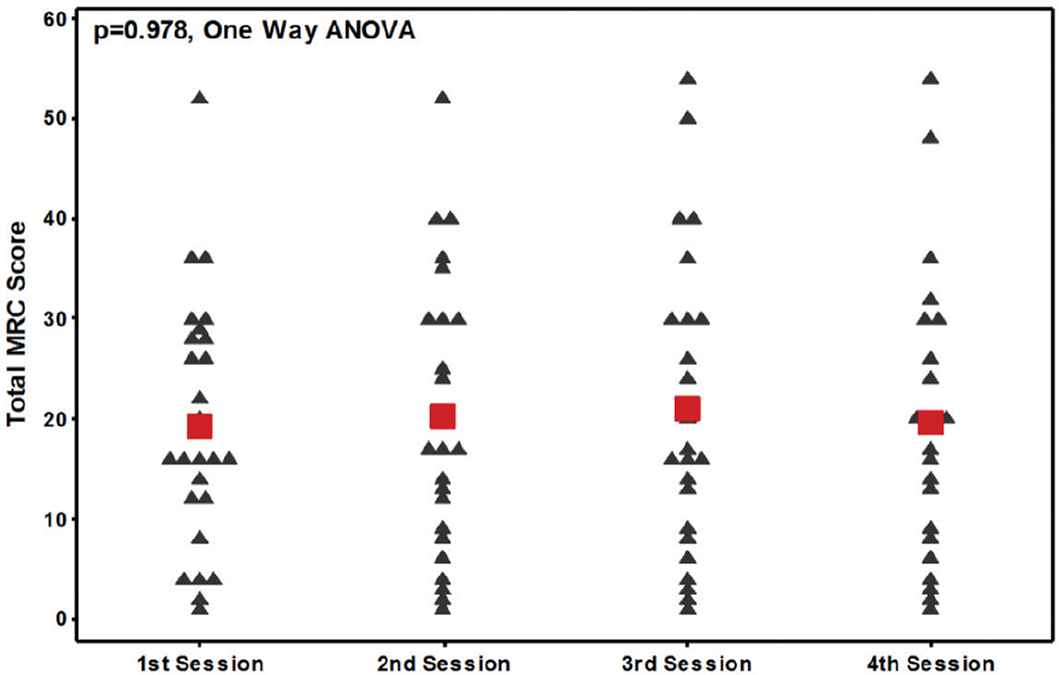
Trends in MRC scores in all plasmapheresis sessions. ANOVA, analysis of variance; MRC, Medical Research Council.
| Parameter | 1st Session | 2nd Session | 3rd Session | 4th Session | p | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | n | Mean | SD | n | Mean | SD | ||
| Platelets | 24 | 224417 | 57659 | 18 | 214111 | 77412 | 19 | 174579 | 50769 | 16 | 174813 | 47326 | 0.014 |
| PT | 21 | 17.3 | 4.231 | 18 | 19.033 | 3.169 | 16 | 17.762 | 3.393 | 10 | 16.75 | 3.29 | 0.352 |
| Albumin | 21 | 4.105 | 1.024 | 19 | 3.716 | 1.01 | 18 | 3.622 | 1.072 | 14 | 3.15 | 0.997 | 0.070 |
| Calcium | 23 | 8.074 | 1.069 | 20 | 7.525 | 1.095 | 18 | 7.461 | 0.889 | 16 | 7.531 | 0.962 | 0.174 |
| MRC score | 26 | 19.38 | 12.41 | 24 | 20.21 | 14.01 | 24 | 21.04 | 15.14 | 22 | 19.68 | 14.46 | 0.978 |
MRC, Medical Research Council; PT, prothrombin time; SD, standard deviation.
One-way analysis of variance for comparison of biochemical parameters and MRC score after four sessions of plasmapheresis
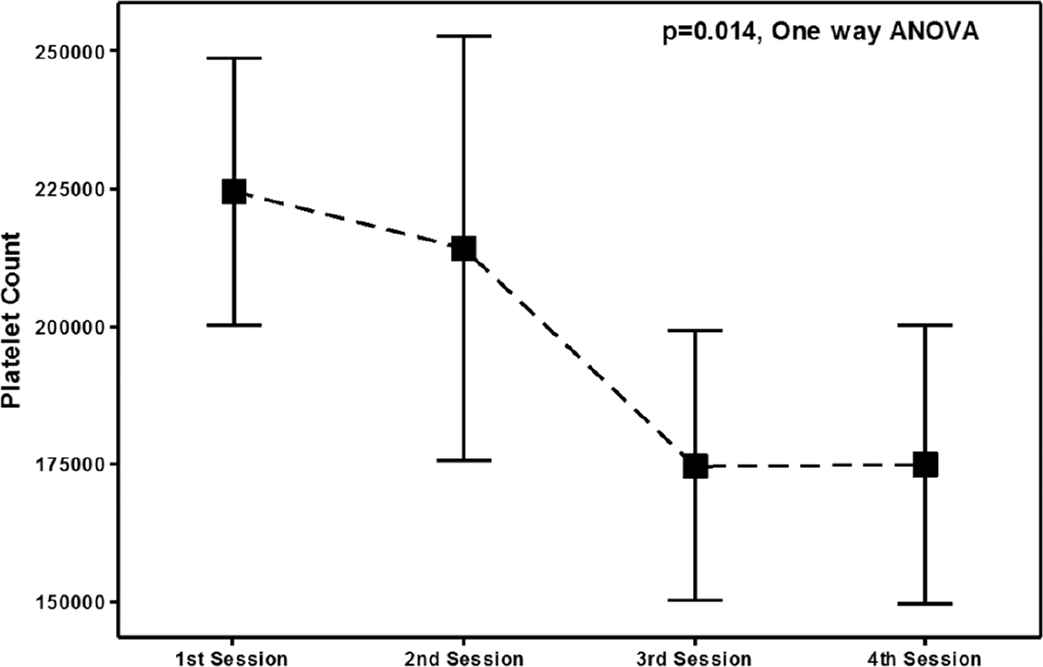
Interval plot for changes in platelet count with plasmapheresis sessions in all patients. Bars are based on 95% confidence interval calculated from standard deviation scores; small square boxes represent mean value. ANOVA, analysis of variance.
3.1. Survival Analysis of Outcome Predictors
Survival analysis showed mean survival of 15.56 days (95% Cl 8.95644–22.1547). A significant decrease in the survival of patients was observed with prolonged hospital stay (survival at day 3 was 88.89% versus 33.33% at day 14) and prolonged preceding illness (survival for duration of preceding illness at day 1 was 85% versus 15% at day 7). However, this was not affected by preceding illness such as diarrhoea and respiratory disorders (p = 0.99 and 0.253, log-rank test). Percentage survival of patients was 84.2% after three plasmapheresis sessions that decreased to 15.7% after four sessions. There was a tendency toward a significant difference in the survival of patients with and without mechanical ventilation (p = 0.085, log-rank test). When applied, the percentage survival of patients on mechanical ventilation decreased with increase in duration of mechanical ventilation (100% on day 10 versus 20% on day 19) (Figure 3a–d).
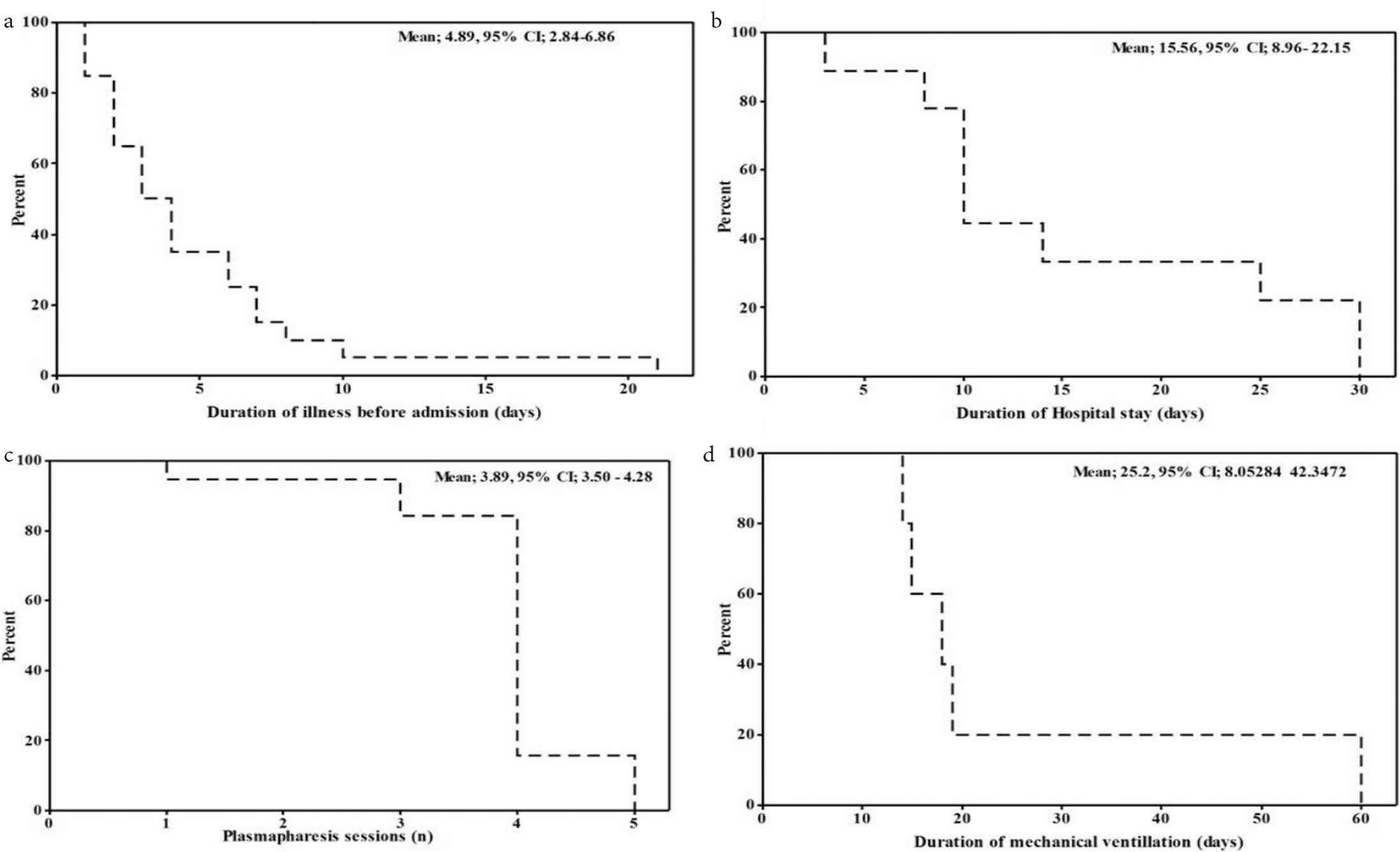
Kaplan–Meier plots for survival analysis of outcome predictors. CI, confidence interval.
4. DISCUSSION
With improvement in treatment support for GBS patients, mortality has reduced over time; however, it remains significant in patients presenting with poor prognostic signs. This was also seen in our study, which indicated 26% mortality by the end of 4 weeks. This is high given the overall mortality of 2–15% in GBS [21]. However, previous studies have reported high mortality particularly in patients requiring mechanical ventilation, older people, and those admitted to intensive care [22].
A significantly higher percentage of patients who died during follow-up had abnormal heart rhythm (tachy/bradyarrhythmia) and increased sweating at nadir, which are the features of autonomic dysfunction due to demyelination of neurons in the somatic and autonomic nervous systems. Autonomic function including heart rate, vasomotor stability, sweating, continence, and blood pressure are generally affected more commonly in children [23]. This may explain the severity of the disease status in patients leading to complications and ultimately death within 1 month. This was supported by the data indicating that cause of death in these patients was cardiac asystole (n = 4), pneumonia due to respiratory muscles paralysis (n = 2), and hypotension (n = 1).
Although GBS affects peripheral nerves, CSF being in close contact with the proximal nerve roots, may potentially reflect biochemical changes related to the disease. Accordingly, changes in the expression, post-translational modifications or turnover of proteins may be reflected as changes in CSF protein content [24]. Abnormalities in CSF protein concentration most frequently seen as isolated blood–CSF barrier dysfunction, as measured by elevated CSF protein concentration or elevated CSF/serum albumin quotient, without an elevated cell count, or intrathecally produced immunoglobulins, are characteristic of GBS and considered as initial evidence of biomarkers present in CSF [25]. In our study, although CSF proteins, calcium, and proportion of lymphocytes were significantly higher than upper-normal range, their levels were not significantly different between the two groups. This indicates a breach in the immune-mediated blood–CSF barrier function, irrespective of the disease outcome. Although evidence suggests that CSF protein may be normal within the first week after disease onset, and that severe increase in CSF protein and albumin may be seen after 2–3 weeks, there are randomized control trials showing that 50% of CSF samples within 1 week and 80% of CSF samples within 2 weeks showed an increase in protein and albumin content [26]. However, this lack of consistency in terms of its appearance makes CSF protein a poor diagnostic marker for GBS in the early days of the disease.
Mean MRC score at baseline is a measure of muscle power in limbs and is a proxy for the extent of peripheral nerve damage by disease process. There is plenty of evidence showing the association of low MRC score with poor disease prognosis. Our data indicate that although there was no difference in baseline MRC score between the two groups, MRC score at baseline had a tendency toward poor disease outcome. A nonsignificant likelihood in this study may be due to low patient numbers. It was however interesting to observe that mean MRC score at baseline did not improve with plasmapheresis sessions, indicating little improvement in the functional status of the patients. This might indicate that treatment with plasmapheresis alone is not sufficient to improve muscle power and hence independent survival in the short term, and that the overall benefit of plasmapheresis sessions and survival of patients depends on other factors [27]. This has been reported by Lin et al. [27] who found that although overall disability score of the patient improves with plasmapheresis sessions, the recovery was poor in patients with poor prognosis. Use of Intravenous Immunoglobulin (IVIG) apart from plasmapheresis is a standard practice and is associated with better survival and functional status of the patients [1]. However, the cost of IVIG prevents its application in resource-poor settings such as in the present study. We observed a significant reduction in platelet count with subsequent plasmapheresis sessions. Since plasmapheresis leads to separation and loss of plasma, it also results in unintentional loss of platelets. This has also been previously observed during plasmapheresis sessions for other diseases such as thrombotic thrombocytopenic purpura [28], and this loss varied with different makes of equipment.
Prolonged preceding illness was associated with reduced survival in our study. This was expected as previous evidence suggests that a delay of >2 days in the initiation of treatment in these patients leads to a poor outcome in terms of morbidity and mortality compared to those who present early [22]. Moreover, patients who present late are likely to require more aggressive and prolonged hospitalization and exhibit delayed recovery. This was supported by finding that percentage survival decreased with prolonged hospital stay.
Although mechanical ventilation has played a key role in improving the survival of patients presenting with respiratory muscle paralysis, our study shows that patients requiring mechanical ventilation for >10 days show a drastic decrease in percentage survival from 100% down to 20%. Patients requiring prolonged mechanical ventilation are at increased risk of poor outcome, decreased independent survival, slow recovery, and ventilator-associated respiratory complications [14,22,29]. Prolonged duration of mechanical ventilation may therefore indicate poor muscle potential and advanced disease state. In a study by Dhar et al., prolonged mechanical ventilation for >60 days was associated with complications. Moreover, pneumonia and sepsis were highly associated with duration of mechanical ventilation for >14 days [29]. However, the strongest predictors of mortality were age and significant comorbidity but not mechanical ventilation (only 8.5% mortality at 1 year) [29]. In another study, older age, increased ventilation time (>4 months), and upper limb paralysis were predictors associated with poor outcome at maximum recovery [22].
Despite some promising results, our study had some limitations. This was a single centre study with a small patient cohort, which might have resulted in some nonstatistical results. Furthermore, patients were not treated with IVIG due to poor resource availability in the study setting, which might have obscured the improvement in mean MRC score at the end of 4 weeks, despite plasmapheresis. Patients were referred to this tertiary care centre from far-flung areas that resulted in delayed onset of treatment tailored for GBS. Detailed data on the clinical and plasma biochemical parameters at the onset of symptoms would therefore have helped to explain the high mortality rate in this small cohort.
In conclusion, this study suggests that mortality in the short term is related to prolonged preceding illness, hospital stay, duration of mechanical ventilation, and increasing number of plasmapheresis sessions. Furthermore, overall MRC score does not improve with subsequent plasmapheresis sessions. It is recommended to carry out larger multicentre studies based on intensive care settings to validate these results.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
MI and FK contributed in study conception and design. AK contributed in acquisition of data. MJK contributed in analysis and interpretation of data. MI and FK contributed in drafting/write-up. WA and IA contributed in critical revision. All authors read and approved the final version of the paper.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Muhammad Ijaz AU - Faheemullah Khan AU - Muhammad Jaffar Khan AU - Asadullah Khan AU - Wiqar Ahmad AU - Iftikhar Ali PY - 2019 DA - 2019/10/07 TI - Outcomes of Guillain–Barré Syndrome Patients Admitted to Intensive Care Unit in Tertiary Care Hospital JO - Dr. Sulaiman Al Habib Medical Journal SP - 88 EP - 94 VL - 1 IS - 3-4 SN - 2590-3349 UR - https://doi.org/10.2991/dsahmj.k.191004.001 DO - 10.2991/dsahmj.k.191004.001 ID - Ijaz2019 ER -
