Reliability of Finger Photoplethysmogram Assessment: Effect of Mental Stress and Day-to-Day Variability

- DOI
- 10.2991/artres.k.210208.001How to use a DOI?
- Keywords
- Arterial stiffness; augmentation index; finger photoplethysmogram; aging; cardiovascular disease risk
- Abstract
Frequent assessment of vascular health (e.g., arterial stiffness) may predict the incidence of cardiovascular disease. The Second Derivative of the finger Photoplethysmogram Aging Index (SDPTGAI) may be used as an index of vascular aging and a screening tool for arteriosclerotic disease. To test its reliability as a measurement of arterial stiffness, we compared SDPTGAI with aortic Augmentation Index (AIx) at rest and during short-term mental stress (study 1). In addition, the day-to-day variability of SDPTGAI was evaluated (study 2). In study 1, a total of 31 apparently healthy adults were measured with the photoplethysmogram on the right index finger in the sitting resting condition. Simultaneously, the applanation tonometry was used to record blood pressure waveforms from the left radial artery (for aortic pressure waveform estimation via a general transfer function). Subsequently, 22 subjects underwent a 30-s arithmetic test (double-digit subtraction). In study 2, 10 young adults were measured with SDPTGAI for five consecutive days. In study 1, we found that SDPTGAI was significantly correlated with AIx (r = 0.682, p < 0.001). During the arithmetic task, heart rate and SDPTGAI were significantly increased from the baseline values (p < 0.05 for both) whereas AIx remained to be unchanged. In study 2, SDPTGAI showed 12.0 ± 9.9% of Coefficient of Variation (CV) across all subjects, which is comparable to CV of heart rate (12.5 ± 5.4%). These findings suggest that SDPTGAI has the potential for evaluating arterial stiffness and wave reflection at the resting condition, but it needs to be measured under well-rested relaxed condition because the finger photoplethysmogram may easily be affected by mental stressor.
- Copyright
- © 2021 The Authors. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
The frequent assessment of vascular health may contribute to increased awareness and prevention of cardiovascular events in general populations. It has been well recognized that arterial stiffness and wave reflection measured by the aortic pulse wave velocity and Augmentation Index (AIx) are the strong predictors of future Cardiovascular events and all-cause mortality [1,2]. However, these measures require technical expertise and knowledge. In this context, the Second Derivative waveform of fingertip Photoplethysmography (SDPTG) can be measured easily from a fingertip placed on the photoplethysmography (PTG) sensor and has the potential for self-monitoring of vascular health during daily living [3]. Previously, several studies have demonstrated clinical and pathophysiological importance of SDPTG indices such as the SDPTG Aging Index (SDPTGAI) [4–6]. Since SDPTGAI is strongly correlated with age, it can be rescaled to years of age which is easily comprehended by general populations [3]. For these reasons, SDPTG indices including the vascular aging index have recently been implemented for ambulatory monitoring devices, but its usability and reliability are not well documented.
Mental stress is an external stimulus that can affect physiological parameters such as arterial tone [5,7], blood viscosity [8], and heart rate [9]. It is reported that pulse wave velocity and AIx are increased with acute mental stress [10,11]. Moreover, skin blood flow shows transient reflex changes in response to various external stimuli (e.g., arousing or painful stimuli, emotional stress) [12]. Since photoplethysmogram optically evaluates blood volume changes in the microvascular bed of cutaneous tissue, SDPTG may be influenced by mental stressor independent of changes in vascular tone and stiffness of the relatively proximal vessels.
Therefore, the purpose of this study was to determine the usability and reliability of SDPTG indices. Specifically, we hypothesized that SDPTGAI is positively correlated with aortic AIx at rest and during short-term mental stress. Also, we investigated the day-to-day variability of SDPTG indices.
2. MATERIALS AND METHODS
2.1. Subjects and Protocol
In study 1, a total of 31 healthy adults (11 men and 20 women, 41 ± 2 years of mean age) were studied. In study 2, 10 young healthy adults (eight men and two women, 24 ± 2 years of mean age) were measured SDPTG for 4–5 consecutive days in the morning (at the same time of day as much as possible). All experimental procedures and protocols conformed to the Declaration of Helsinki and were approved by the Institutional Review Board (#2016-695, National Institute of Advanced Industrial Science and Technology). All subjects provided written informed consent before participation.
2.2. Measurements and Analysis
Study 1. After 5 min of quiet resting, all subjects underwent simultaneous recordings of the photoplethysmogram on the right index finger and the applanation tonometry to record blood pressure waveforms from the left radial artery in the sitting posture (resting). Then, a subgroup of subjects (n = 22) underwent mental arithmetic test which consisted of a control trial followed by an arithmetic trial (non-random order) with approximately a 5-min interval. In the control trial, participants read out two-digit numbers presented every 2 s on a computer screen for 30 s. In the arithmetic trial, participants verbally answered two-digit subtractions presented every 2 s on a computer screen for 30 seconds.
The intermittent brachial cuff and continuous radial blood pressure waveforms were recorded from the left arm during each trial using a vascular screening device (HEM-9010AI, Omron Healthcare, Kyoto, Japan). The brachial pressure was measured by the oscillometric method while the radial pressure waveforms were recorded by applanation tonometry (HEM-9010AI, Omron Healthcare). The SDPTG was collected from the right index finger using a customized finger PTG device (Alps, Tokyo, Japan). All of the measurements above were simultaneously recorded during the resting and task periods. Radial artery pressure waveforms were converted to aortic pressure waveforms via a validated generalized transfer function (SphygmoCor software, AtCor Medical, Sydney, Australia) as previously reported [13]. AIx was calculated as pressure wave above its systolic shoulder divided by pulse pressure [14]. AIx was adjusted for 75 bpm of heart rate (AIxHR75) was also obtained because it is affected by changes in heart rate independent of arterial stiffness and wave refection [15]. Heart rate was estimated from the averaged pulse interval.
Figure 1 presents sample PTG signals of the resting and the mental stress conditions. As shown in bottom panels, the SDPTG is characterized by five inflection points on finger PTG waves: the initial positive (A), early negative (B), re-increasing (C), late re-decreasing (D), and diastolic positive waves (E), respectively. Absolute values of these waves’ heights were obtained and used to calculate B/A ratio, D/A ratio, and SDPTGAI (= [B − C − D − E]/A) as previously reported [3]. The higher B/A ratio (= lower negative ratio) suggests low elasticity, vasoconstriction, and arteriosclerosis [5]. The D/A ratio is closely related to the augmentation of blood pressure in the aorta by wave reflection, an index to assess left ventricular (LV) afterload [5].
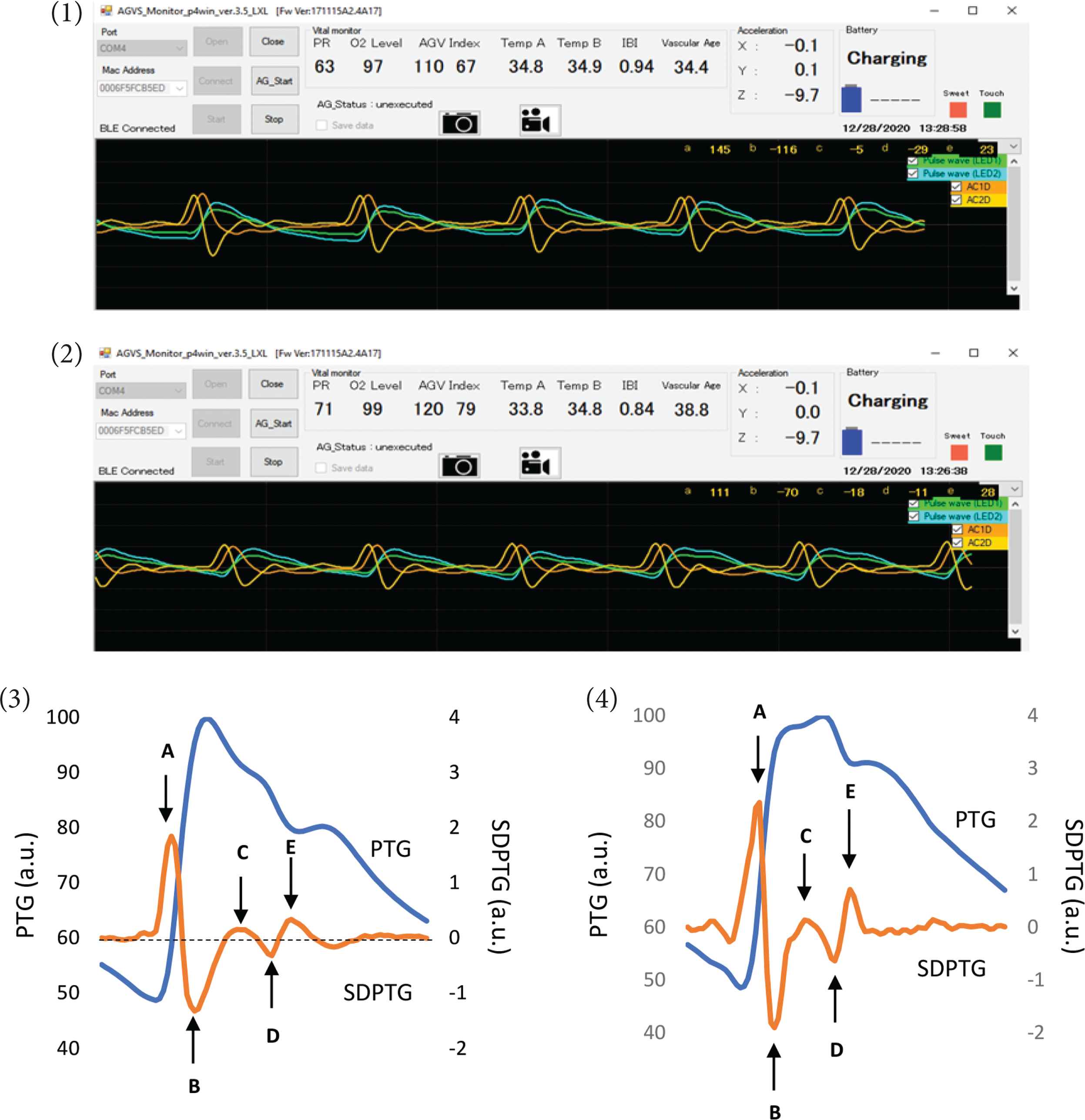
Samples of finger Photoplethysmogram (PTG) during the resting (1) and the mental stress (2) conditions. Bottom panels indicate synthesized 1-beat PTG (blue lines) and the Second Derivative of the finger Photoplethysmogram (SDPTG, orange lines) during the resting (3) and the mental stress (4) conditions, respectively. A–E are five inflection points on finger PTG waves characterized by the SDPTG: the initial positive (A), early negative (B), re-increasing (C), late re-decreasing (D), and diastolic positive waves (E). a.u. indicates arbitrary unit.
Study 2. To investigate the day-to-day variability of SDPG indices, each subject underwent measurement of SDPTG after a 5-min quiet resting for 4–5 consecutive days in the morning (at the same time of day as much as possible).
2.3. Statistical Analysis
In study 1, intra-observer reproducibility of the SDPTG indices and aortic AIx was examined by Intraclass Correlation (ICC) between baseline measurements of the control and arithmetic conditions. A simple correlation analysis was performed to determine the relationship between variables of interest. Baseline variables were compared by paired t-test. A generalized linear model of repeated measures analysis of variance was used to determine the interaction effect of condition (i.e., control vs. mental arithmetic) and time (i.e., pre vs. during task). In case of a significant F-test, post-hoc pairwise Bonferroni comparisons were performed. In study 2, the day-to-day variability of B/A ratio, D/A ratio, and SDPTGAI were evaluated by calculating the Coefficient of Variation (CV) from the Standard Deviation (SD) and average values. As a secondary analysis, each CV was compared between two groups based on the time of measurement (before 9:00 am vs. after 11:00 am). Data are presented as mean and SD. Statistical significance was set a priori at p < 0.05. All data analyses were performed using a commercial software (SPSS, Version 25, IBM Corp., Armonk, NY, USA).
3. RESULTS
Study 1. Excellent intra-observer reproducibility was observed on the B/A ratio (ICC = 0.868), D/A ratio (ICC = 0.793), SDPTGAI (ICC = 0.914), and AIx (ICC = 0.844) (p < 0.001 for all). Figure 2 depicts relationships between AIx and SDPTG indices. The B/A ratio (r = −0.531), D/A ratio (r = 0.740), and SDPTGAI (r = 0.682) were significantly correlated with AIx (p < 0.001 for all).
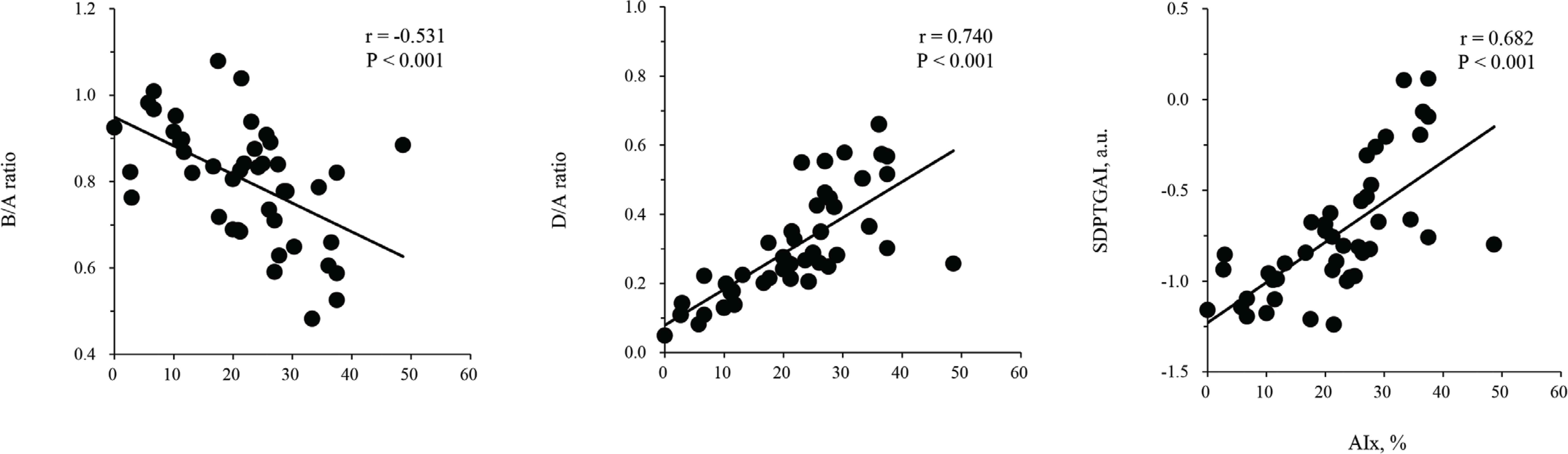
Scatterplots of Augmentation Index (AIx) and the Second Derivative of the finger Photoplethysmogram (SDPTG) indices. a.u. indicates arbitrary unit.
There were no significant differences in the baseline blood pressure, heart rate, SDPTG indices, AIx, and AIxHR75 between the control and arithmetic trials (Table 1). As shown in Figure 3, heart rate significantly increased during the control (+3.6 ± 5.2 bpm, p = 0.008) and arithmetic (+8.4 ± 4.9 bpm, p < 0.001) tasks from their corresponding baseline values. Moreover, heart rate during the arithmetic task was significantly higher than that during the control task (p = 0.001). During the arithmetic task, D/A ratio significantly increased from the baseline (p < 0.001). SDPTGAI also significantly increased from the baseline (p = 0.002) and was significantly higher than that during the control task (p = 0.006). The B/A ratio significantly decreased by 9% from the baseline (p < 0.001) during the arithmetic task and was significantly lower than that during the control task (p = 0.004). Significant interaction between trial and time was not seen in either AIx (p = 0.437) or AIxHR75 (p = 0.351).
| Variables | Control trial | Arithmetic trial | p-values |
|---|---|---|---|
| Heart rate, bpm | 76 ± 7 | 75 ± 8 | 0.936 |
| Systolic BP, mmHg | 121 ± 10 | 121 ± 10 | 0.976 |
| Mean BP, mmHg | 91 ± 10 | 91 ± 9 | 0.923 |
| Diastolic BP, mmHg | 74 ± 10 | 74 ± 9 | 0.923 |
| AIx, % | 22.0 ± 10.1 | 21.8 ± 12.1 | 0.969 |
| AIxHR75, % | 21.9 ± 9.7 | 21.8 ± 10.8 | 0.972 |
| B/A ratio, ratio | 0.79 ± 0.13 | 0.82 ± 0.14 | 0.493 |
| D/A ratio, ratio | 0.33 ± 0.16 | 0.29 ± 0.14 | 0.404 |
| SDPTGAI, a.u. | −0.72 ± 0.36 | −0.77 ± 0.36 | 0.635 |
Data are mean and SD. p-values were obtained by the paired t-test.
BP, blood pressure; AIx, augmentation index; AIxHR75, AIx adjusted by 75 beat/min of heart rate; B/A ratio, the ratio of the absolute height of the early negative wave to that of the initial positive wave of SDTPG; D/A ratio, the ratio of the absolute height of the late re-decreasing wave to that of the initial positive wave of SDTPG; SDPTGAI, SDPTG aging index.
Baseline hemodynamic variables, augmentation index, and the Second Derivative finger Photoplethysmogram (SDPTG) indices
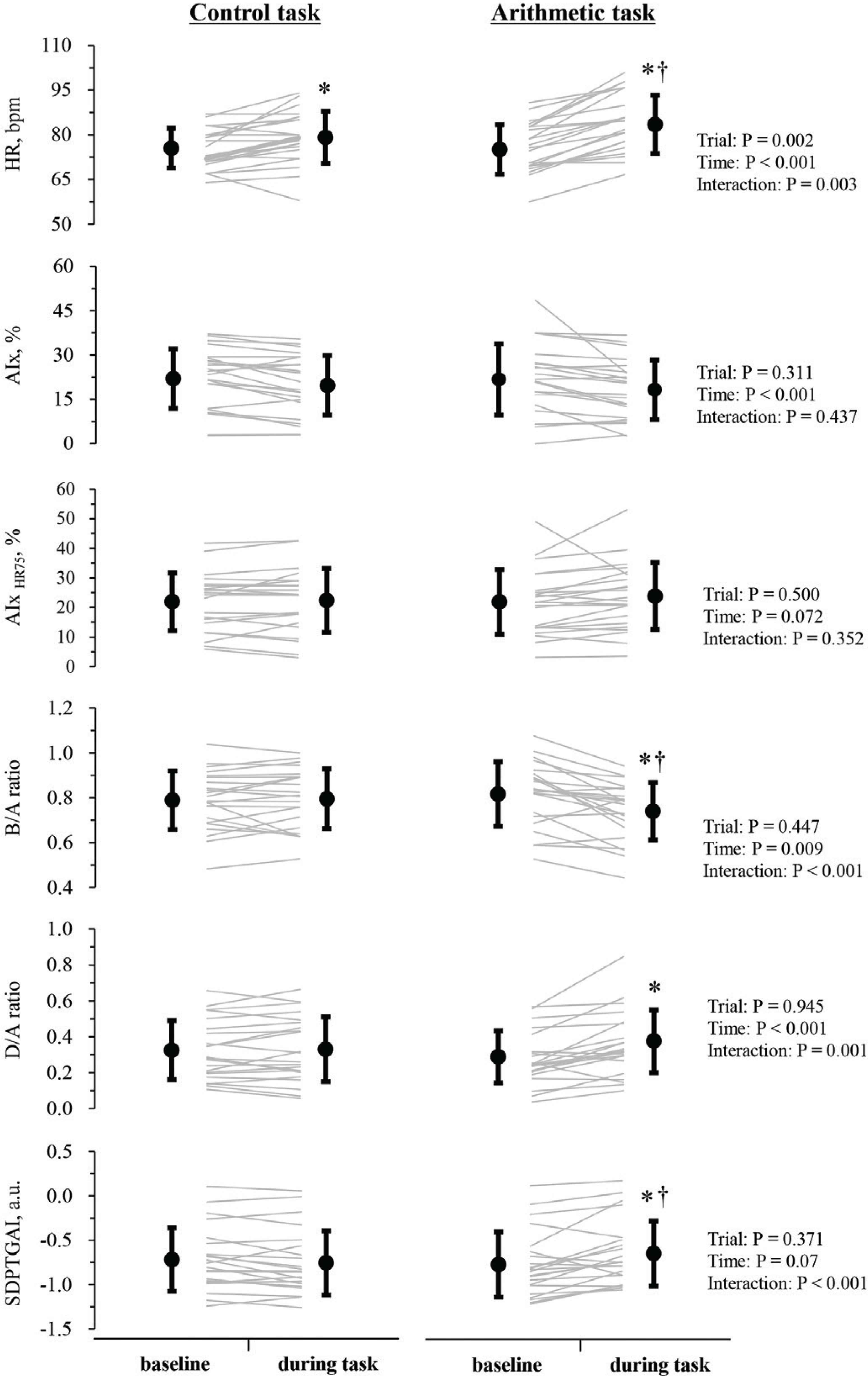
Responses of heart rate, Augmentation Index (AIx), and the Second Derivative of the finger Photoplethysmogram (SDPTG) indices to mental arithmetic. AIxHR75 indicates AIx adjusted by 75 beat/min of heart rate. Gray lines indicate individual data. Closed circles and error bars are mean and SD. *Indicates significant difference from the baseline. †Indicates significant difference with during task in the control condition. a.u. indicates arbitrary unit.
Study 2. Mean and SD of heart rate and SDPTG indices for five consecutive days were summarized in Table 2. CV of pulse rate, B/A ratio, D/A ratio, and SDPTGAI were calculated in each subject. The average CV across all subjects were 12.5 ± 5.4% for pulse rate, 10.6 ± 5.9% for B/A ratio, 128.7 ± 139.9% for D/A ratio, and 12.0 ± 9.9% for SDPTGAI. When subjects were divided into two group based on the time of measurement before 9:00 am (n = 6, mean time of day = 7:35 am) or after 11:00 am (n = 4, mean time of day = 11:45 am), the former group exhibited significantly smaller CV of the B/A ratio (7.6 ± 4.5 vs. 15.0 ± 5.0%, p = 0.043) and SDPTGAI (6.6 ± 4.4 vs. 20.1 ± 10.8%, p = 0.043) than the other groups, whereas no significant group-differences in CV of pulse rate (7.6 ± 4.5 vs. 14.8 ± 6.6%, p = 1.0) and D/A ratio (93.9 ± 66.1 vs. 181.0 ± 213.0%, p = 0.24) were observed.
| Pulse rate, beat/min | B/A ratio, ratio | D/A ratio, ratio | SDPTGAI, a.u. | |
|---|---|---|---|---|
| Day 1 (n = 10) | 65 ± 13 | −0.81 ± 0.11 | −0.14 ± 0.09 | −0.95 ± 0.21 |
| Day 2 (n = 10) | 70 ± 21 | −0.81 ± 0.11 | −0.10 ± 0.10 | −0.94 ± 0.23 |
| Day 3 (n = 10) | 69 ± 21 | −0.86 ± 0.13 | −0.16 ± 0.15 | −0.97 ± 0.17 |
| Day 4 (n = 10) | 74 ± 19 | −0.82 ± 0.10 | −0.06 ± 0.10 | −1.02 ± 0.15 |
| Day 5 (n = 9) | 63 ± 10 | −0.83 ± 0.10 | −0.11 ± 0.10 | −1.01 ± 0.18 |
| CV, % (n = 10) | 12.5 ± 5.4 | 10.6 ± 5.9 | 128.7 ± 139.9 | 12.0 ± 9.9 |
Data are mean and SD of across all subjects on each day. CV indicates mean and SD of individual the coefficient of variation for 5-day measurement. Abbreviations for SDPTG indices were indicated in Table 1. a.u. indicates arbitrary unit.
Day-to-day reproducibility of pulse rate and the Second Derivative finger Photoplethysmogram (SDPTG) indices
4. DISCUSSION
The main findings from this study are twofold: (1) SDPTGAI increased during a short mental arithmetic task (e.g., 30 s) although AIx and AIxHR75 remained unchanged; (2) SDPTGAI exhibited excellent reproducibility when it was measured within approximately 10 min, and was positively correlated with AIx. However, the day-to-day variability of SDPTGAI was about 12%. Collectively, these findings suggest that SDPTGAI has the potential for evaluating arterial stiffness and wave reflection, but it should be measured under the well-relaxed resting condition because the finger photoplethysmogram may easily be affected by external stimuli such as mental stress.
Several studies demonstrated clinical and pathophysiological importance of SDPTG indices [4–6]. The B/A ratio, D/A ratio, SDPTGAI can be acquired in a short time and easily by placing a fingertip on the photoplethysmogram sensor. Therefore, this technique has been proposed as a self-monitoring device for healthcare in non-clinical settings such as homes and offices. However, evidence supporting the usability and reliability of SDPTG indices has remained sparse and inconclusive.
Photoplethysmogram optically measures blood volume changes in the microvascular bed of tissue. Since vasoconstriction of microvascular bed may occur instantly with elevation of blood pressure and reduction of skin blood flow during arousing or emotional stress [12], SDPTG may largely be influenced by mental stressor independent of changes in vascular tone and stiffness of the proximal blood vessels. In this study, SDPTG indices changed drastically by a short-term mental stress whereas AIx and its heart rate-adjusted value remained unchanged. Several studies reported that acute mental stress evoked increases in arterial stiffness and wave reflection evaluated by pulse wave velocity and AIx [10,11]. Such inconsistency might be due to a duration of mental stress as previous studies conducted 3–5 min of mental arithmetic task. In general, the B/A ratio, D/A ratio, and SDPTGAI have been considered as markers of the distensibility of large arteries, the intensity of the reflected wave from the periphery, and vascular aging, respectively [5]. Indeed, at the baseline (resting state), SDPTG indices were strongly correlated with AIx. These results suggest that SDPTG indices partly reflect arterial stiffness and wave reflection under the resting condition.
Augmentation index is affected by changes in heart rate independent of arterial stiffness and wave refection [15]. Of note, the mental arithmetic stimulation increased heart rate but AIx and AIxHR75 did not change significantly. Nevertheless, SDPTG indices significantly altered by the mental arithmetic stimulation. Therefore, alterations in SDPTG indices during acute mental stress is likely to reflect changes in microvascular blood volume and vasoconstriction to a greater extent than arterial stiffness and wave reflection.
In study 1, we obtained ICC of the SDPTG indices and aortic AIx based on the first (e.g., control task) and second (e.g., arithmetic task) baseline values. These measures exhibited excellent reproducibility when they were measured within approximately 10 min. On the other hand, the day-to-day variability of B/A ratio and SDPTGAI were 10–12% and comparable to that of pulse rate. The D/A ratio showed substantially poor day-to-day variability, shown by 128.7 ± 139.9% of CV. This might be attributed to the small height of D wave which can easily be affected by peripheral vascular tone [5].
Interestingly, SDPTG indices measured after 11:00 am showed significantly larger CV of the B/A ratio and SDPTGAI than the those measured before 9:00 am. These results suggest that SDPTG may have diurnal variation and be influenced by external stimuli such as daily life events and mental stress as shown in study 1. Therefore, it is recommended that the measurement should be performed under the stress-free environment in a quiet room at comfortable room temperature after at least 10 min of rest, as recommended by an expert consensus document of aortic stiffness measurement [16]. In addition, to ensure the reliability of the SDPTG indices, the results of repeated measurements (ideally, in the early morning) may need to be referenced.
5. CONCLUSION
We determined the usability and reliability of SDPTG indices by comparing between SDPTG indices and AIx at rest and during a short-term mental stress test. We also investigated the day-to-day variability of SDPTG indices. Our findings suggest that SDPTGAI has the potential for evaluating arterial stiffness and wave reflection, but it should be measured under the well-relaxed resting condition because the finger photoplethysmogram may easily be affected by external stimuli such as mental stress. Therefore, to ensure the reliability of the SDPTG indices, the results of repeated measurements (ideally, in the early morning) may need to be referenced.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
MF contributed in data collection, data analysis, drafting of the manuscript. TY contributed in data collection. TT contributed in data collection, data analysis, and editing of the manuscript. JS contributed in conceptualization of the study, supervision of the project, data analysis, and editing of the manuscript. All authors contributed in final approval.
ACKNOWLEDGMENT
The authors deeply thank Ms. Mitsuho Hanamoto for her technical assistance.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Marina Fukuie AU - Takashi Tarumi AU - Takayuki Yamabe AU - Jun Sugawara PY - 2021 DA - 2021/02/13 TI - Reliability of Finger Photoplethysmogram Assessment: Effect of Mental Stress and Day-to-Day Variability JO - Artery Research SP - 107 EP - 111 VL - 27 IS - 3 SN - 1876-4401 UR - https://doi.org/10.2991/artres.k.210208.001 DO - 10.2991/artres.k.210208.001 ID - Fukuie2021 ER -
