The Curious Case of a Missing Coeliac Trunk: A Case Report and Review of the Literature
- DOI
- 10.2991/artres.k.200422.001How to use a DOI?
- Keywords
- Coeliac trunk; gastrosplenic trunk; paraneoplastic syndrome
- Abstract
Introduction: The anatomy of the coelic trunk is highly variable. An understanding of the variations is important in general and vascular surgery due to the implications of disruption and consequent visceral ischaemia.
Case Description: A case is described of a 69-year-old woman presenting with undifferentiable abdominal pain, eventually leading to a diagnosis of aortitis and uterine cancer. Computed tomography (CT) angiography revealed a unique coeliac trunk variation with the common hepatic artery (CHA) arising directly from the abdominal aorta, and a splenogastric trunk, a relatively rare variant.
Discussion: The clinical picture was unique, with the anatomical variant complicating case. There are several clinical consequences of these anomalies, but it is critical for operative surgeons to understand the normal anatomy as well as variants to reduce surgical risks. The literature describes various classification methodologies, which assist in approaches intraoperatively. Predominantly stenting, chemoembolisation and catheterisation based procedures require a rigid understanding of the various anomalies that can be encountered, even though this case (Morita Class III) only presents in 0.23% of cases. This is sufficiently often enough that it is important to bring to light variations in the anatomy of the coeliac trunk.
- Copyright
- © 2020 Association for Research into Arterial Structure and Physiology. Publishing services by Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
There is extensive study on the anatomy of the coeliac trunk due to its significant splachnic branches and thus essential supply of supracolic abdominal organs. Described as the Tripus Halleri” [1], a strong understanding of the normal anatomy is required for an operative surgeon; however, it is important to appreciate potential variants due to their variety and commonality, being present in 15% of cases [2]. A standard coeliac trunk is a trifurcation at the level of T12 of the Common Hepatic Artery (CHA), Left Gastric Artery (LGA) and Splenic Artery (SA). Anomalies include subtractive variants which involve these arteries projecting from the abdominal aorta separate from the main trunk, hence given names based on the related arteries. Sometimes there is complete absence of a trunk. There are multiple classification standards for these variations; for this report, Morita’s classification of the coeliac trunk will be used [1].
Furthermore, additive formations have been described, with even as far as a hexafurcation of the trunk being documented in the literature [2,3]. Clinical concern attached to variation in coeliac trunk is minimal though can be identified in rare conditions. Steal syndrome has been described when the inferior phrenic and supra-renal arteries act as collaterals for the coeliac trunk with this circulation being occluded, particularly if the phrenic artery origin is distal to the site of occlusion [2,4]. Additionally, compression of the coeliac trunk by the median arcuate ligament of the diaphragm in Dunbar’s syndrome where the coeliac trunk can be longer than normal due to the coeliac origination of the inferior phrenic arteries [2,5,6].
Significantly more pertinent to a surgical patient is an understanding of the anatomy by the operating surgeon, particularly in difficult pancreatic and splenic procedures, as well as resections. Understanding and being able to identify arteries that supply the organs distal to the pancreas in order to determine if clipping or redirection of blood flow is necessary in the case of resections [2]. Risks of damaging arteries in cases of abnormal vasculature are also increased in abdominal surgeries.
Asymptomatic anatomical anomalies are poorly documented in the literature even though they are relatively common, particularly in living patients due to the inherent lack investigation need. Usually they are found in autopsies or cadavers, but it is rarely documented in complex medical scenarios even though it is not the cause of presenting symptoms. In this case report a rare anatomical anomaly of the coeliac trunk is documented with a solitary CHA and a gastrosplenic trunk present, as an incidental finding in the diagnosis of aortitis as an incredibly rare paraneoplastic syndrome of metastatic uterine cancer.
2. CASE REPORT
Mrs. Je was a 69-year-old Arabic speaking lady who presented to the emergency department of a large tertiary hospital in Sydney, Australia, with a 4-days history of nausea, vomiting and loss of appetite. Additionally there was generalised abdominal pain that was not peritonitic. She had opened her bowels normally throughout this period as well as on the morning of admission. There was a significant background history of Polymyalgia Rhematica (PMR) diagnosed 2 years ago, chronic obstructive pulmonary disease (COPD), hypertension, dilated cardiomyopathy, atrial fibrillation and a history of complex migraines (following the course of the PMR).
On examination, there was a mild fever, she was tachycardic, normotensive, slightly tachypnoiec but saturating well on room air. There were no cardiac or pulmonary symptoms. The abdomen was soft yet with general abdominal pain, but particularly isolated to the epigastrium, which did not radiate. On deep palpation there was some guarding, and bowel sounds were present on auscultation.
Review of prior documentation revealed that the PMR initially presented as weakness and pain in the upper limbs associated with pain in the hips and a concurrent headache about 2 years prior to this admission. This was considered to be giant cell arteritis but was never diagnosed due to Mrs. Je’s apprehension with anaesthetic during the temporal artery biopsy. She was thus steroid dependent for 2 years with a flare up 6 months prior to this admission, with the PMR never truly resolving.
A psychosocial history was unremarkable with Mrs. Je coming from home, was independently mobile with independent activities of daily living, and a moderate smoking history.
Investigations were multimodal with an initial abdominal X-ray yielding no significant results. The Computed Tomography (CT) scan with contrast presented an interesting picture of aortitis with inflammation of the wall of the aorta. Initially considered an infective picture, she was started on empirical antibiotics, but an obvious source was unable to be located. Eventually a positron emission tomography (PET) scan was arranged which revealed an asymptomatic uterine cancer which had metastasised to the vertebrae and liver (Figure 1). With an obvious shock to Mrs. Je, their family, and frankly the treating team, the patient was placed on a palliative pathway. It was likely that the aortitis and PMR were a paraneoplastic syndrome, following the time course of the pathogenesis of a metastatic uterine cancer.

PET scan revealed a large uterine cancer with metastases to the liver and vertebrae.
In investigating the aortitis, an adherent arrangement of the coeliac trunk was noted. At the level of vertebra T12, the CHA separated directly from the abdominal aorta, while a splenogastric trunk leading to an early bifurcation of the LGA and SA, sat slightly left of the CHA (Figure 2a and 2b). The CHA travelled anteriorly 19 mm to the course infero-laterally to the right for 26 mm. At this point the right gastric artery branched anteriorly to run over the antero-superior border of the stomach commencing at pylorus. Very shortly thereafter the gastroduodenal artery branched anteriorly to run posterior to the first part of the duodenum. The hepatic artery proper then travelled supero-laterally toward the porta hepatis. The LGA branched within 8 mm from the commencement of the gastrosplenic trunk, initially from the superior right side of the trunk, to then travel supero-laterally on toward the left to reach the cardiac portion of the lesser curvature of the stomach. The SA branch continued anteriorly for another 18 mm where it sharply turned to the right and tortuously travelled on the posterior side of the pancreas on its traditionally described course until the hilum of the spleen. This variation is schematically demonstrated in Figure 3.

Demonstration on abdominal CT with contrast of the common hepatic artery and splenogastric trunk. The left gastric artery exits out of the inferior portion of the gastrosplenic trunk (a), with the splenic artery continuing forward (b).
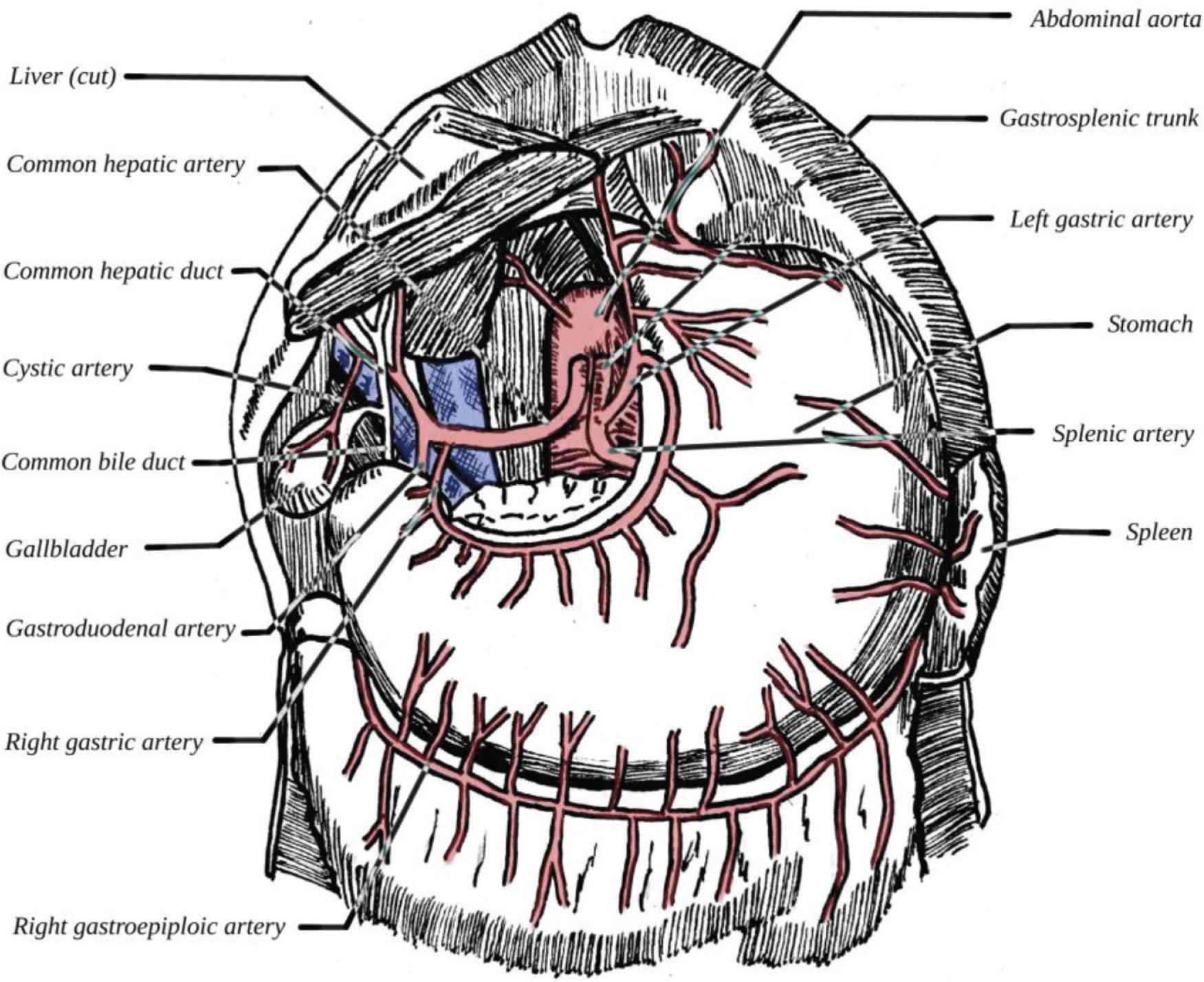
Schematic and labelled diagram of coeliac trunk variant with surrounding viscera included.
Additionally, an accessory left renal artery was noted, approximately 4.5 cm below the origin of the right renal artery (Figure 4) though this likely had no clinical bearing.

An accessory left renal artery can be appreciated about 4.5 cm inferior to the origin of the right renal artery, of which there is only one.
3. DISCUSSION
There are a variety of classifications of coeliac trunk anomalies. Using the Morita’s classification (Table 1) of the coeliac trunk, this is a relatively rare form defined as Type III. Across 9829 patients, a systematic review found that this was present in only 0.23% of patients, and specifically the rarest variant where the CHA arises as a solitary branch from the abdominal aorta and also the rarest form where a gastrosplenic artery is present. Other similar variants include a splenogastric trunk with the CHA arising from the superior mesenteric artery (1.13%) of cases or a hepatomesenteric trunk (1.90%) [1].
| Class | Description |
|---|---|
| Type I | Typus Halleri; trifurcation of the coeliac trunk |
| Type II | Hepatosplenic trunk; LGA arising from the abdominal aorta |
| Type III | Splenogastric trunk; CHA arising from the abdominal aorta |
| Type IV | Hepatogastric trunk; SA arising from the abdominal aorta |
| Type V | Complete absence of a coelic trunk |
Morita’s classification of the coeliac trunk [1]
A potential explanation for these anatomical anomalies can be given by investigating the embryology of the abdominal aorta and splanchnic arteries. The abdominal aorta is formed as a fusion of two dorsal aortae at the end of the 1st month of gestation. Each of these aortae produce branched paired vitelline arteries which are termed primitive digestive trunks. Three groups are defined as the dorsal, lateral and ventral branches with the ventral branches fusing in the median to then become the four roots of the gut. There is an extensive ventral longitudinal anastomosis initially, but the fusion of the first three roots forms the coeliac trunk. The fourth root forms the superior mesenteric artery and later migrates inferiorly, tracking with the natural shift of the organs that are supplied. Inappropriate fusion or movement of supplied organs can lead to anomalous arterial supply [1,7,8].
While there is rarely a clinical relevance to these anatomical anomalies aside from steal syndrome and Dunbar’s syndrome as previously described [2,4–6], an operative surgeon requires an understanding of the potential for the abnormality and the have the ability to identify them. For the interventional radiologists, understanding the branching pattern as well as pathways to relevant organs is critical for both diagnostic and therapeutic angiography. This is also relevant in embolisation and when the treatment requires coeliac trunk-hepatic artery catheterisation.
Pseudoaneurysms can present in various procedures involving the pancreas and in pancreatitis itself. These may require selective embolisation for appropriate treatment. A poor understanding of the anatomy could lead to complications and unexpected difficulties (the axiom of measure twice, cut once, is valid here, suggesting prior visualisation or imaging of the anatomy when the coeliac trunk is relevant to the procedure). Finally, specific to interventional radiology, defining the coeliac trunk anatomy in transarterial hepatic artery chemoembolisation when it is an appropriate treatment modality is essential [1,6,9].
In the context of vascular surgery, it is increasingly common for patients with giant cell arteritis (GCA) to present with abdominal aneurysm. An endovascular aneurysm repair, particularly if a fenestrated stent is used, would require an extensive understanding of the underlying aortic anatomy. In general surgery, procedures involving the pancreas or spleen require and understanding of the vascular anatomy in order to prevent risk of damaging the essential arteries. Clipping or redirection of the blood flow can be necessary in the event of resections which needs an understanding of the complex vascular variations [1,8].
4. CONCLUSION
The coeliac trunk is a critical arterial branch of the abdominal aorta as it supplied blood flow to multiple supra-colic abdominal organs. While it is standard anatomy has been extensively described, anomalies are common and critical to identify in procedures that involve the vasculature or relevant relations of the abdominal aorta. A unique case was described of a patient with a paraneoplastic presentation of aortitis in the context of metastatic uterine cancer, leading to an incidental finding of a highly rare Morita Type III variant of the coeliac trunk, only seen in 0.23% of patients. While this did not present any complications in the context of the admission, it presented an important learning point for operative surgeons to be aware of the variations of the anatomy, particularly in the context of procedural intervention in interventional radiology, vascular and general surgery.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
ECS devised and wrote the presented manuscript and prepared the hand-drawn diagram in Figure 3. APH and AS both contributed to the review and edit of the entire manuscript.
Footnotes
REFERENCES
Cite this article
TY - JOUR AU - Erin Cihat Saricilar AU - Ashley Peter Heyworth AU - Animesh Singla PY - 2020 DA - 2020/04/28 TI - The Curious Case of a Missing Coeliac Trunk: A Case Report and Review of the Literature JO - Artery Research SP - 121 EP - 124 VL - 26 IS - 2 SN - 1876-4401 UR - https://doi.org/10.2991/artres.k.200422.001 DO - 10.2991/artres.k.200422.001 ID - Saricilar2020 ER -
