Effects of aging on leg pulse wave velocity response to single-leg cycling
- DOI
- 10.1016/j.artres.2010.07.002How to use a DOI?
- Keywords
- Arterial stiffness; Endothelial function; Aging
- Abstract
There is increasing awareness that pulse wave velocity (PWV), an index of arterial stiffness, changes transiently via alteration of vascular smooth muscular tone. The aim of this study was to determine the effects of aging on the response of leg PWV to a low-intensity exercise bout. Ten older (69 ± 3 years) and 6 younger (21 ± 1 years) men were studied. Leg PWV in each subject was measured before and after a low-intensity single-leg cycling (20 W, 5 min). The younger subject group demonstrated a significant reduction in the exercised leg PWV (−8.0%) immediately after the exercise, whereas the non-exercised leg PWV did not change significantly (+2.2%). In the older subject group, no significant changes in PWV were observed in the exercised leg nor the non-exercised leg. There were no significant changes in other hemodynamic variables before or after the exercise bout in either younger or older subjects. These results indicate that the exercise-induced temporal reduction in leg arterial stiffness is blunted in older adults. The lack of exercise-induced reduction in leg PWV may be due to an age-related impairment of endothelial function.
- Copyright
- © 2010 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Pulse wave velocity (PWV), introduced by Bramwell and Hill in 1922,1 is an established index of arterial stiffness. PWV is a widely used research tool for the early detection and prevention of cardiovascular disease.2 It has been considered that PWV reflects mainly changes in structural properties of the arterial wall (i.e., wall stiffening or thickening with increased pulse wave velocity).3 However, there is increasing recognition that PWV changes transiently via employing vasoactive drugs or sympathetic nervous activation,4–6 suggesting that PWV may be altered with acute changes in vascular smooth muscle tone.
Exercise evokes vasodilatory substances in working muscle7–9 to increase blood flow and meet the muscular metabolic demand. Therefore, dynamic exercise may reduce smooth vascular tone and hence PWV of the exercised limb. We and others reported that low-, moderate-, and high-intensity cycling exercise decreases leg PWV.10–13 Sugawara et al.12,13 demonstrated that PWV decreases in the exercised leg, but not in the counterpart, after 5-min low-intensity single-leg cycling, suggesting that the decrease in arterial stiffness in the exercised leg was induced mainly by exercise-related regional factors (e.g., endothelial-derived relaxing factor). If the change in arterial stiffness is associated with endothelial function, the response of leg PWV to the exercise may be blunted with aging. However, the effect of aging of the acute change in PWV after the exercise has not been clarified. Accordingly, we tested the hypothesis that the exercise-induced decrease in PWV is blunted in older adult.
Methods
Ten older (69 ± 3 years old, 164 ± 2 cm of height, 57.7 ± 2.2 kg of body weight, 21.8 ± 0.4 kg/m2 of body mass index) and 6 younger (21 ± 1 year old, 168 ± 1 cm of height, 62.3 ± 1.3 kg of body weight, 22.2 ± 0.7 kg/m2 of body mass index) men were studied. Participants were recruited from the city and its surrounding community as well as the University using flyers. Highly trained endurance athletes, smokers, and patients with cardiovascular disease or orthopedic impairment in the lower limbs were excluded. All participants were sedentary or recreationally active. Two elderly men were prescribed anti-hypertensive medicine and 1 elderly man was prescribed medicine for diabetes mellitus. The study was reviewed and approved by the Institutional Review Board at The University of Tsukuba. All subjects gave their written informed consent to participate.
The subjects abstained from alcohol, caffeine, and intense exercise for at least 24 h before the experiments. All experiments were carried out in a temperature-controlled room (25 °C). Each subject performed 5 min of single-leg (left) cycling at 20-W workload on a cycle ergometer (232C-EX, Combi, Tokyo, Japan) in the supine position. Before (baseline) and after (2 min and 5 min) the single-leg cycling, heart rate, 4-extremities blood pressure, and PWV in both legs were measured, as we previously reported.12,13 Heart rate and brachial blood pressure were also monitored during the exercise test. Heart rate and 4-extremities blood pressure were acquired with ECG and oscillometric devises (form-PWV/ABI, Colin, Komaki, Japan). PWV (= arterial path length/pulse transit time) between the common femoral to the posterior tibial arteries was evaluated with the automatic PWV measurement system equipped an applanation tonometry probe and cuffs connected to a plethysmographic sensor. The applanation tonometry probe was placed at the right inguinal region to record pressure waveforms of the right common femoral artery. Cuffs were wrapped over both ankles to record pressure waveforms of the posterior tibial arteries. These pressure waveforms were simultaneously recorded at 1200 Hz (common femoral artery) or 240 Hz (posterior tibial arteries). The delay times between the sharp systolic upstroke starts of the right femoral and both posterior tibial arterial pulse waves were determined by the automatic waveform analyzer.12,13 Arterial path length was assumed the straight distance between 2 sensors and measured manually with a tape measure. The day-to-day coefficient of variation for leg PWV in our laboratory was 2.3 ± 0.6%.
All values are expressed as means ± SE. Results were analyzed by repeated-measures ANOVA. With regard to significant F-values, Newman–Keuls post hoc test was used to identify significant differences among mean values. Statistical significance was set at P < 0.05 for all comparisons.
Results
At baseline, there were no significant differences in brachial blood pressures and heart rate between groups (Table 1). Heart rate and blood pressure increased during the exercise and returned to the baseline level in both groups. Brachial systolic blood pressure and mean arterial pressure during the exercise were significantly higher in elderly men compared with young men. There were no significant differences in ankle blood pressure before and after the exercise in either young or elderly men (Table 2).
| Variables | Group | Before exercise | During exercise | 2-min after exercise | 5-min after exercise |
|---|---|---|---|---|---|
| Heart rate, bpm | Young | 53 ± 4 | 78 ± 3* | 55 ± 3 | 54 ± 3 |
| Elderly | 68 ± 5 | 83 ± 4* | 67 ± 5 | 64 ± 5* | |
| Brachial SBP, mmHg | Young | 111 ± 3 | 121 ± 2 | 112 ± 3 | 108 ± 3 |
| Elderly | 120 ± 4 | 140 ± 5*† | 121 ± 4 | 118 ± 4 | |
| Brachial MAP, mmHg | Young | 83 ± 2 | 91 ± 2 | 83 ± 2 | 81 ± 3 |
| Elderly | 93 ± 3 | 104 ± 3*† | 90 ± 3 | 90 ± 3 | |
| Brachial DBP, mmHg | Young | 65 ± 2 | 70 ± 1* | 67 ± 1 | 63 ± 2 |
| Elderly | 76 ± 3 | 80 ± 3* | 74 ± 3 | 73 ± 2 |
SBP = systolic blood pressure, MAP = mean arterial pressure, DBP = diastolic blood pressure. Data are mean and SE.
P < 0.05 vs. before exercise.
P < 0.05 vs. young group.
Responses of heart rate and brachial blood pressure to the single-leg cycling.
| Variables | Group | Non-exercised leg | Exercised leg | ||||
|---|---|---|---|---|---|---|---|
| Before exercise | 2-min after exercise | 5-min after exercise | Before exercise | 2-min after exercise | 5-min after exercise | ||
| Ankle SBP, mmHg | Young | 125 ± 3 | 127 ± 3 | 123 ± 3 | 126 ± 3 | 125 ± 4 | 124 ± 2 |
| Elderly | 134 ± 6 | 137 ± 7 | 137 ± 6 | 135 ± 4 | 136 ± 5 | 136 ± 6 | |
| Ankle MAP, mmHg | Young | 87 ± 3 | 88 ± 2 | 86 ± 4 | 87 ± 2 | 84 ± 2 | 82 ± 3 |
| Elderly | 93 ± 3 | 95 ± 5 | 94 ± 3 | 93 ± 3 | 95 ± 3 | 92 ± 3 | |
| Ankle DBP, mmHg | Young | 69 ± 3 | 70 ± 2 | 67 ± 3 | 67 ± 2 | 65 ± 2 | 65 ± 3 |
| Elderly | 75 ± 3 | 73 ± 3 | 74 ± 3 | 72 ± 3 | 72 ± 3 | 72 ± 2 | |
Data are mean and SE. SBP = systolic blood pressure, MAP = mean arterial pressure, DBP = diastolic blood pressure.
Responses of ankle blood pressure to the single-leg cycling.
PWV of both legs was significantly greater in elderly than young men before and after the exercise (Fig. 1). Younger group demonstrated a significant reduction in the exercised leg PWV (−8.0%) immediately after the exercise, whereas the non-exercised leg PWV did not change significantly (+2.2%) (Fig. 1). PWV of both legs gradually decreased thereafter, with the PWV of the exercised leg significantly lower. The ratio of the exercised and non-exercised leg PWV was significantly lower after the exercise compared with before the exercise (Fig. 2). In older subjects, no significant changes in PWV were observed in the exercised leg or the non-exercised leg (Fig. 1). And hence, the ratio of the exercised and non-exercised leg PWV did not alter (Fig. 2).
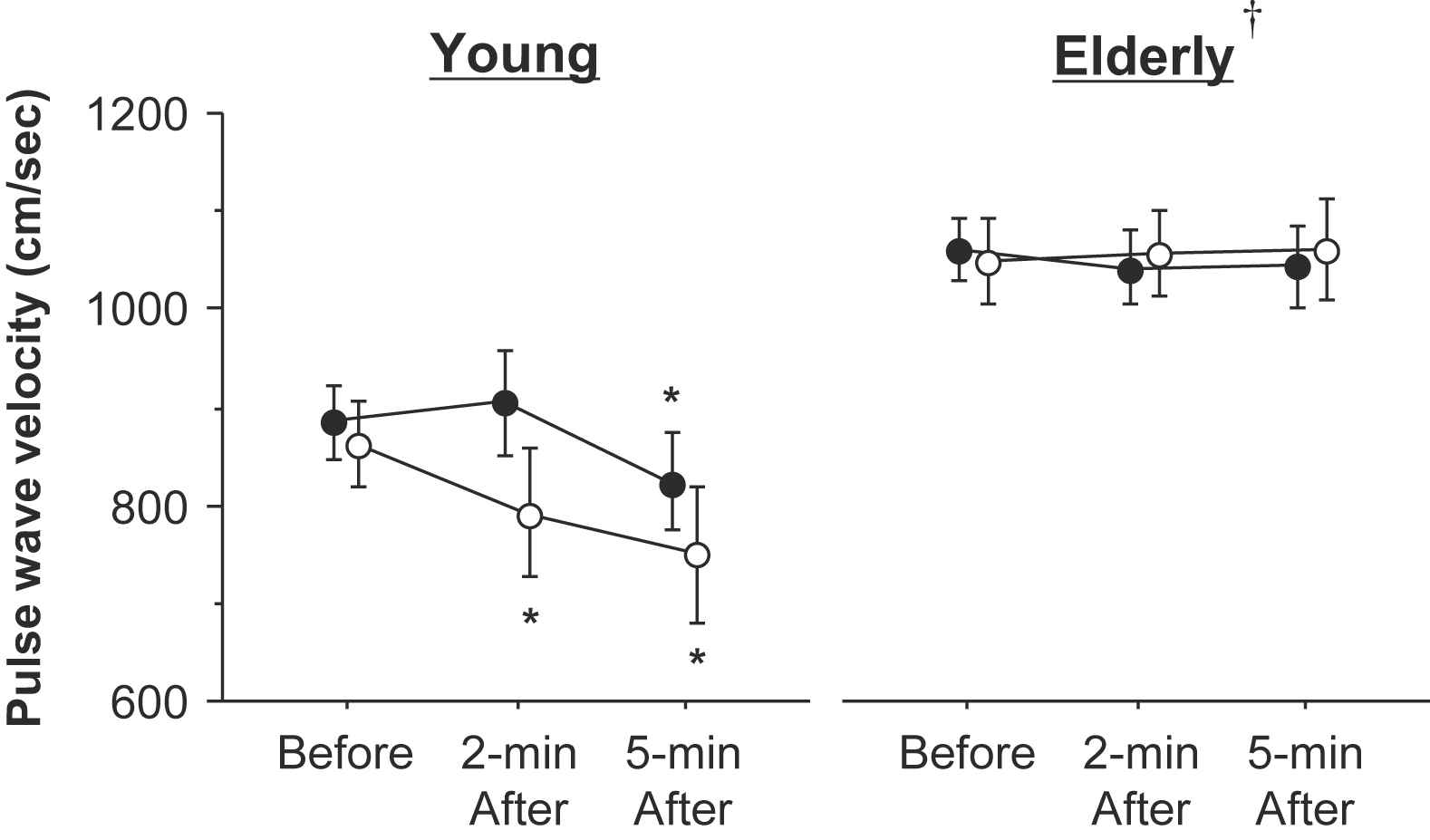
Responses of leg pulse wave velocity (PWV) to the single-leg cycling. Open circles are exercised leg and closed circles are non-exercised leg. †: PWV of both legs was significantly greater in elderly than young men before and after the exercise. *: P < 0.05 vs. before exercise.
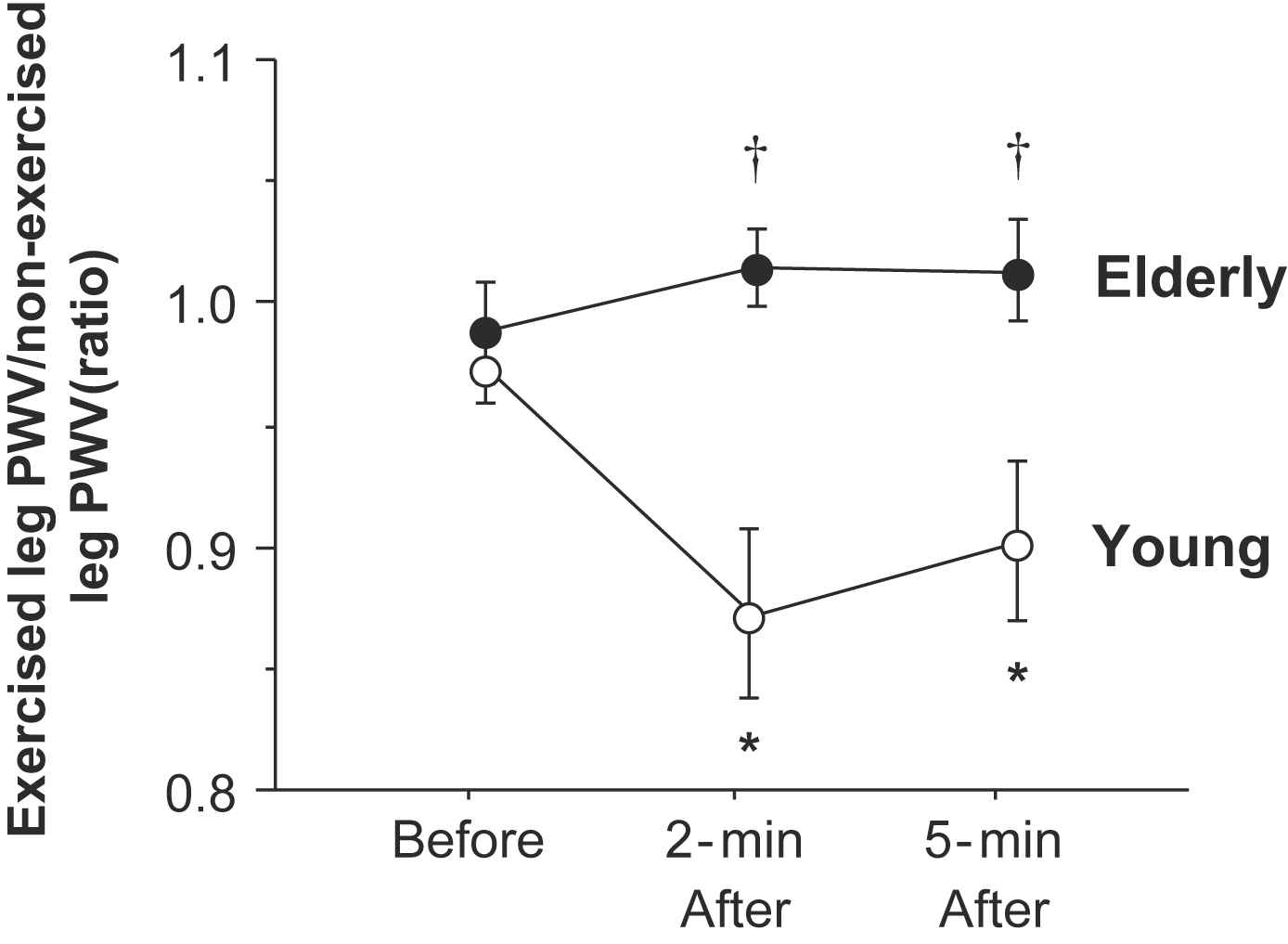
Changes in the ratio of the exercised and non-exercised leg pulse wave velocity (PWV) with the single-leg cycling. †: The ratio of the exercised and non-exercised leg PWV was significantly greater in elderly than young men. *: P < 0.05 vs. before exercise.
Discussion
We previously identified in young healthy adults that pulse wave velocity of the exercised leg, not of the non-exercised leg, decreases after the low-intensity, 5-min single-leg cycling. These results suggest arterial stiffness or vascular smooth muscular tone is lowered mainly by the exercise-related regional factors (e.g., endothelial-derived relaxing factor). If such phenomena are associated with endothelial function, the reduction in exercised leg PWV would be blunted in older adults because of the decrease in endothelial function associated with aging.14–16 Accordingly, we tested this hypothesis using a cross-sectional study design. Young subjects demonstrated a significant reduction in the exercised leg PWV immediately after the exercise, but not in the older counterpart. The non-exercised leg PWV decreased slightly 5 min after the exercise, which might be due to the other systemic factors (i.e., sympathetic nervous activity, hormonal factor, circulating vasodilatory metabolites). However, the decreased ratio of the exercised and non-exercised leg PWV was comparable between 2 min and 5 min after the exercise. These results suggest that the influence of the regional factor remained constant. In the older subject cohort, there were no significant changes in PWV observed either in the exercised leg nor the non-exercised leg. These results indicate that exercise-induced temporal reduction in leg arterial stiffness is blunted in older adults.
Based on these findings, it is important to consider the underlying mechanism of the reduction in exercised leg PWV. Nitric oxide (NO) appears to be the most likely reason for the change in PWV because of several factors: NO is produced from the endothelial cell by the increased shear stress and lowers vascular smooth muscular tone. Such flow-mediated vasodilatory response is attenuated by the administration of NO synthase inhibitor.17–19 NO is evoked in working muscle during exercise,8,9 whereas NO production and its bioavailability decrease with aging.14–16 However, we previously observed that systemic inhibition of NO synthase did not alter the exercise-induced reduction in leg PWV.12 Is not the absence of the decrease in the exercised leg PWV associated with the lower NO production and bioavailability? In this context, a recent study20 showed that radial artery flow-mediated vasodilation (FMD) was preserved even when the intraarterial NO synthase inhibitor was employed, suggesting that NO may not be obligatory for radial artery FMD in healthy volunteers. Although FMD has been assumed to reflect selectively NO bioavailability, it is plausible that other shear-evoked dilator mechanisms (i.e., prostacyclin and endothelium-derived hyperpolarizing factor) can compensate for impaired NO production. Together, the lack of the reduction in the exercised leg PWV observed in elderly men might be associated with the aging-related impairment of endothelial function.
Endothelial dysfunction is a risk factor for cardiovascular disease and is becoming a focal point in the efforts for early detection and prevention of cardiovascular disease.17–19 Although the FMD technique has been established as a noninvasive evaluation of endothelial function, this measure requires high levels of technical expertise and an expensive ultrasound machine and may be burdened by considerably large intra- and inter-observer variability. Thus, alternative or complementary approaches to evaluate endothelial function have been introduced. In this line, the response of PWV to the exercise may be used as a noninvasive and nonintrusive method for measurement of endothelial function. Further study to examine the reliability and usefulness is warranted.
Several limitations of this study should be noted. First, we studied small number of subjects as well as a heterogeneous population including patients with hypertension and diabetes mellitus. Second, we did not run blood biochemistry analysis. Hypertension and metabolic irregularities might influence blood pressure response to the exercise,21 which might be a confounding factor. However, responses of leg PWV in these patients were similar to the other healthy adults.
In conclusion, we determined the effects of aging on responses of leg PWV to the low-intensity, short term single-leg cycling. The salient finding is the absence of the exercise-induced decrease in PWV in older men. These results might be attributed to the age-related impairment of endothelial function.
Acknowledgement
This work was supported by the
References
Cite this article
TY - JOUR AU - Jun Sugawara AU - Takeshi Otsuki AU - Seiji Maeda PY - 2010 DA - 2010/08/06 TI - Effects of aging on leg pulse wave velocity response to single-leg cycling JO - Artery Research SP - 94 EP - 97 VL - 4 IS - 3 SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2010.07.002 DO - 10.1016/j.artres.2010.07.002 ID - Sugawara2010 ER -
