Aortic root calcification and cardiac risk factors in patients with coronary calcium score greater than zero using multidetector computed tomography
- DOI
- 10.1016/j.artres.2015.02.002How to use a DOI?
- Keywords
- Aortic root; Coronary atherosclerosis; Risk factors; Calcification
- Abstract
Background: Vascular calcification is a marker of atherosclerotic burden and is associated with increased risk of cardiac events. The aim of this study was to investigate the relationship between clinical cardiac risk factors and aortic root calcification (ARC) in patients with a coronary calcium score (CCS) > 0, as assessed by multidetector computed tomography (MDCT).
Method: Between January and December 2013, 196 consecutive Iraqi patients who underwent MDCT for assessment of coronary disease were recruited. Of these, 69 patients with a CCS > 0 were enrolled in the study. For analytical purposes, patients were divided into two groups by ARC score: patients with ARC > 0 (ARC group, n = 32) and those with ARC = 0 (non-ARC group, n = 37).
Results: The overall prevalence of ARC was 46%. Mean ARC was 174 ± 28.5 (range, 10–500). A significant correlation was observed between ARC and male sex (r = 0.380, P = 0.032) and between ARC and age ≥65 years (r = 0.353, P = 0.047). These correlations persisted even after multivariate adjustment for other cardiac risk factors. There were no significant correlations between ARC and other cardiac risk factors, and the only significant between-group difference in the distribution of cardiac risk factors was in patient age.
Conclusion: ARC was significantly correlated with older age and male sex in patients with CCS > 0.
- Copyright
- © 2015 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Introduction
Arterial calcification is an active systemic process that involves multiple mechanisms responsible for calcium deposition in different arterial beds. It accompanies advanced atherosclerosis, which leads to increased cardiovascular morbidity and mortality.1
A growing body of evidence suggests that both thoracic aortic calcification and coronary calcification have histological relationships to atherosclerosis2 and that both have predictive value for atherosclerotic burden and cardiovascular disease morbidity and mortality.3,4
Because evaluation of calcifications of the aortic root and thoracic aorta is not a standard part of routine cardiovascular workup, little information exists regarding the association between aortic root calcification (ARC) and coronary atherosclerotic burden and risk factors. In our previous work, we found that ARC was significantly correlated with coronary calcification and atherosclerotic burden, suggesting that ARC can be used as an additional imaging marker for assessment of coronary atherosclerosis.5
In this study, we investigated the relationship of clinical cardiac risk factors (hypertension, smoking, diabetes mellitus, hyperlipidemia, family history of premature coronary disease, obesity, male sex, and older age) and ARC in patients with coronary atherosclerosis (CCS > 0) using multidetector computed tomography (MDCT).
Materials and methods
This cross-sectional study was carried out at the Cardiology Center at Al-Sader Teaching Hospital between January and December 2013. Informed consent was obtained from all study participants. The study was approved by our institution’s ethics committee.
Between January and December 2013, we recruited 196 consecutive patients who underwent 64-slice MDCT angiography for assessment of coronary artery disease (CAD) at our institution. All patients had intermediate pretest probability of ischemic heart disease, based on age, sex, and cardiac symptoms. Of 196 patients, 69 with coronary atherosclerosis (CCS > 0) were found to be eligible and were enrolled in the study.
For analytical purposes, patients were divided into two groups by ARC score: patients with ARC score >0 (ARC group, n = 32) and those with ARC score = 0 (non-ARC group, n = 37). A standardized questionnaire was employed by physicians at the time of coronary MDCT angiography to obtain a history of conventional cardiac risk factors for CAD from each patient. Risk factors included a family history positive for premature CAD (occurring before the age of 55 years in men and before 65 years in women); current smoking history (more than 10 cigarettes per day in the last year); history of hypertension or use of antihypertension medications; hyperlipidemia, defined as total cholesterol ≥ 200 mg/dL or a serum triglyceride ≥ 50 mg/dL or use of lipid-lowering drugs; history of diabetes mellitus or use of insulin or glucose-lowering drugs; and obesity (body mass index ≥ 30). Patients with two or more cardiac risk factors were considered to have multiple risk factors.
CT scan protocol
CT coronary angiography was performed with a 64-slice scanner (Aquilon 64, v. 4.51 ER 010; Toshiba Medical Systems, Tochigi, Japan). Before multi-slice CT angiography was performed, a non-contrast CT was acquired to measure the calcium score according to the Agatston method for total heart calcium (summed across all lesions identified within coronary arteries) using a sequence scan with a slice thickness of 3 mm. Coronary calcification area was defined as at least three contiguous voxels with a CT density >130 Hounsfield units. When the patient’s heart rate was more than 65 bpm, a β-blocker (metoprolol; 20–60 mg orally) was administered before the scan. A bolus of 80 ml contrast medium (Omnipaque; 350 mg/ml iodine) was injected intravenously at a rate 5 ml/s, followed by 30 ml of normal saline. The scan was obtained from the aortic arch to the level of the diaphragm during a single breath hold. Using retrospective ECG-gating and ECG-dependent tube current modulation, the following parameters were performed: collimation, width 32.5 × 32.5 cm; slice thickness, 0.5 mm; rotation time, 0.35 s; tube voltage, 120 kV; maximum effective tube current, 890 mA; and table feed, 0.3 mm/rotation at 75% of R–R cardiac cycle. Examination time took ~10 s.
CT images were reconstructed using a smooth kernel (B25f) with a slice thickness of 0.5 mm (increment of 0.3 mm). CT data sets were transferred to a dedicated workstation (Vitrea 2 Workstation; Vital Image, Plymouth, MN, USA) for image analysis.
Aortic root calcification analysis
The aortic root was defined as the part of the aorta lying within 3 cm from the caudal aspect of the aortic annulus containing sinuses of Valsalva and the sinotubular junction. The total calcium score of the aortic root was calculated using Agatston method according to this definition. Areas in the aortic root with an attenuation >130 Hounsfield units and an area >1 mm2 were considered to be calcified lesions. All MDCT images were assessed by two independent radiologists with more than 5 years’ experience in coronary MDCT angiography interpretation.
Statistical analysis
Data are presented as mean ± standard deviation or as numbers with percentages, as appropriate. Categorical data are expressed as frequencies and group comparisons were performed using Pearson’s chi-square test. Continuous variables are presented as mean ± standard deviation and were compared using the Student’s t-test or analysis of variance, as appropriate. Associations between cardiac risk factors, age, and sex of patients with ARC were examined using Pearson’s correlation analysis. Multiple logistic regression was used to analyze the association of clinical risk factors with ARC. A P-value of less than 0.05 was considered statistically significant. SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis.
Results
Patient characteristics are summarized in Table 1. The overall prevalence of ARC in our sample was 46% (mean 81 ± 139). The ARC group comprised 32 patients (18 were female [56%], 14 were male [44%]; mean age 64.7 ± 1.3 years). Mean ARC was 174 ± 28.5 (range, 10–500). The prevalence of risk factors in this group were as follows: hypertension, 23 (72%); smoking, 10 (31%); hyperlipidemia, 5 (16%); diabetes mellitus, 10 (31%); family history of premature coronary disease, 2 (6%); obesity, 8 (25%); multiple risk factors, 19 (59%). Of all cardiac risk factors, only male sex (r = 0.380, P = 0.032) (Fig. 1) and age ≥65 years (r = 0.353, P = 0.047) (Fig. 2) were significantly correlated with ARC. These correlations persisted even after multivariate adjustment for other cardiac risk factors (Table 2).
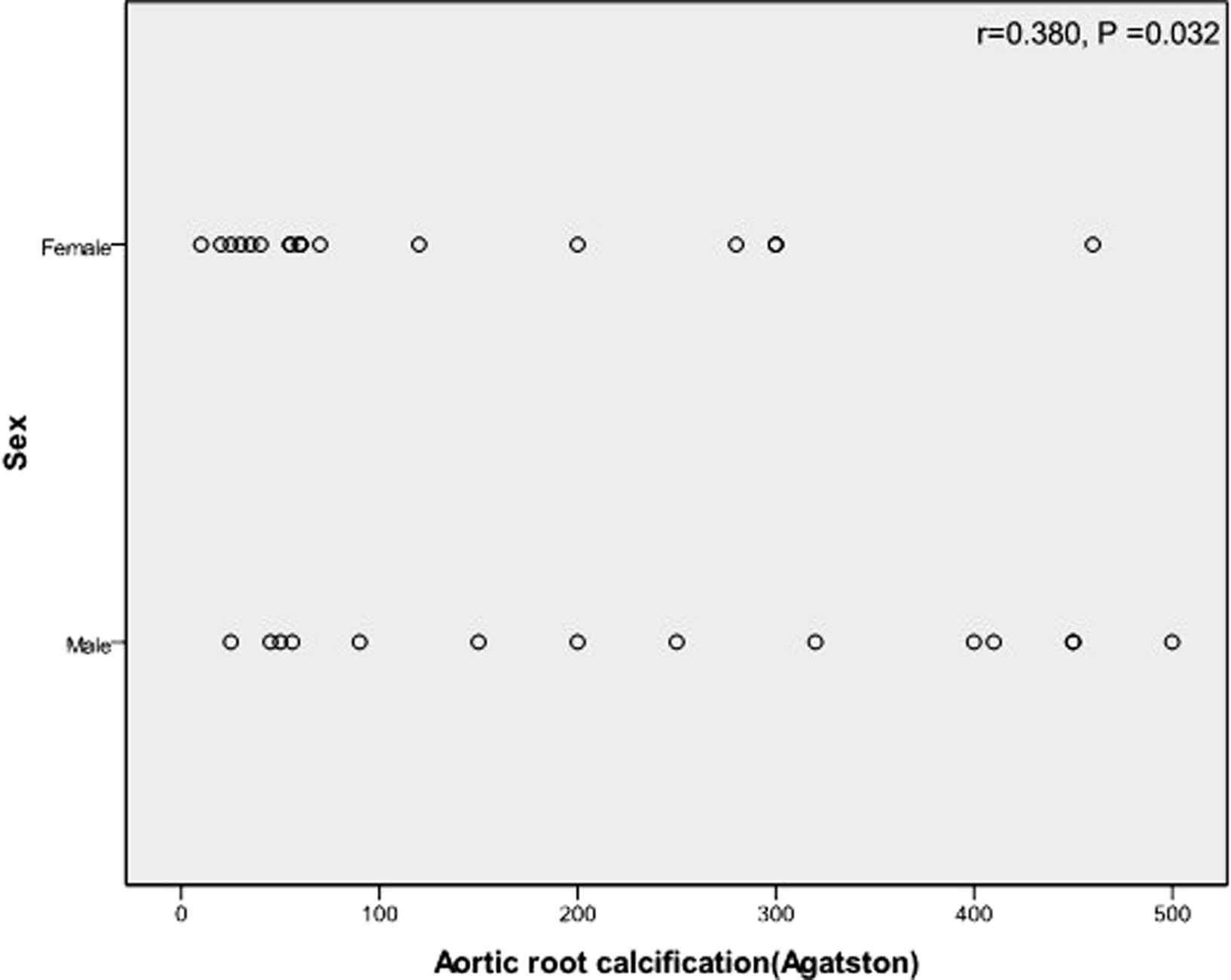
Graph showing a significant correlation between ARC and male sex.
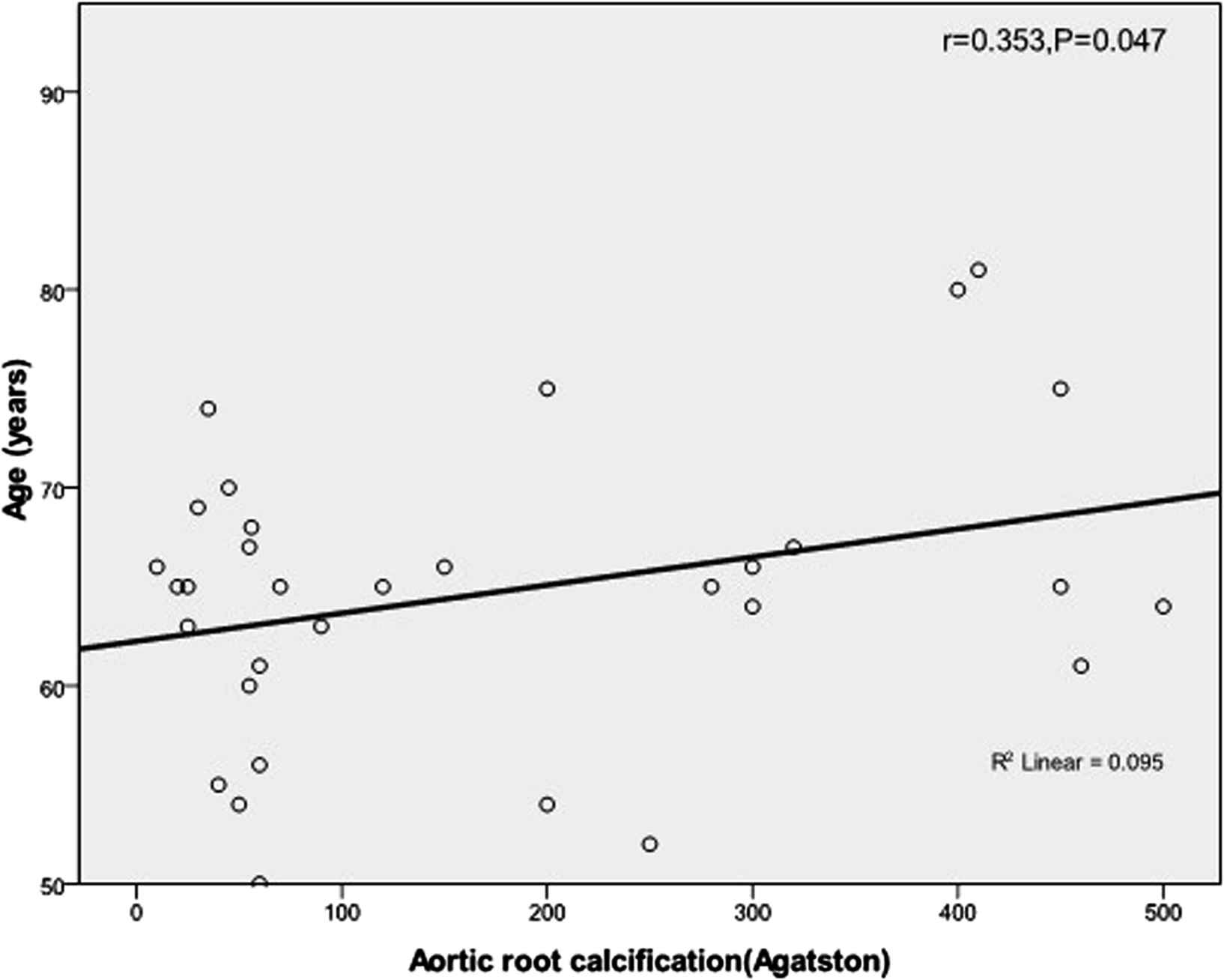
Graph showing a significant correlation between ARC and age ≥65 years.
| Parameter | No. (%) |
|---|---|
| Male | 34 (50.7) |
| Female | 35 (49.3) |
| Mean age (years) | 60.9 ± 1 |
| Risk factors | |
| Hypertension | 45 (65) |
| Smoking | 21 (30) |
| Diabetes mellitus | 20 (29) |
| hyperlipidemia | 16 (23) |
| Family history | 3 (4) |
| Obesity | 18 (26) |
| Multiple | 42 (61) |
Patients characteristics.
| Parameter | P Value | Un-standardized coefficients B |
|---|---|---|
| Male sex | 0.032 | 121.640 |
| Age | 0.038 | 7.194 |
| Hyperlipidemia | 0.05 | 177.48 |
| Obesity | 0.17 | 93.061 |
| Hypertension | 0.4 | 68.037 |
| Multiple | 0.6 | 28.837 |
| Smoking | 0.7 | 16.458 |
| Family history | 0.83 | 24.353 |
| Diabetes | 0.85 | 12.423 |
Clinical cardiac risk factors association with ARC by stepwise multiple logistic regression.
There was a significant association between age ≥65 years and ARC (P = 0.007) (Table 3) but no other significant differences in the distribution of cardiac risk factors between the ARC and non-ARC groups.
| Risk factor | ARC | Non ARC | P Value |
|---|---|---|---|
| Hypertension | |||
| Present | 23 | 22 | 0.8 |
| Absent | 9 | 15 | |
| Smoking | |||
| Present | 10 | 11 | |
| Absent | 22 | 26 | 0.89 |
| Diabetes mellitus | |||
| Present | 10 | 10 | |
| Absent | 22 | 27 | 0.7 |
| Hyperlipidemia | |||
| Present | 5 | 11 | |
| Absent | 27 | 26 | 0.16 |
| Family history | |||
| present | 2 | 1 | |
| Absent | 30 | 36 | 0.4 |
| Obesity | |||
| Present | 8 | 10 | |
| Absent | 24 | 27 | 0.84 |
| Multiple | |||
| Present | 19 | 23 | |
| Absent | 13 | 14 | 0.81 |
| Sex | |||
| Male | 14 | 20 | |
| Female | 18 | 17 | 0.393 |
| Age | |||
| ≥65 years | 19 | 10 | 0.007 |
| <65 years | 13 | 27 | |
Comparison between ARC and non-ARC groups in the distribution of cardiac risk factors.
Discussion
The aortic root is characterized by its close anatomical proximity to the cardiac chambers and the ostial origins of the right and left coronary arteries. The aortic root can be evaluated using MDCT without additional radiation exposure or the use of contrast, and aortic root lesions and calcification can be easily evaluated and followed using transthoracic echocardiography.
Assessment of the aortic root is likely to be used increasingly to evaluate the morphology of the aorta prior to transcatheter aortic valve implantation and for low-dose chest computed tomography examination.6 For these reasons, it is important to assess the aortic root in the clinical setting.
We studied the relationship of cardiac risk factors and ARC status in patients with coronary atherosclerosis based on the presence of coronary calcification. Coronary calcification has been reported to be highly specific for the presence of coronary atherosclerosis and aortic calcification (thoracic or abdominal) shares cardiovascular risk factors and clinical significance with CAD.7 Thoracic aortic calcification has been shown to be independently related to coronary calcification and increased cardiovascular morbidity and mortality.8 Therefore, patients with CAD are at higher risk for aortic calcification compared with those without coronary atherosclerosis.9
In the present study, there were significant correlations between ARC and age ≥65 years and between ARC and male sex, but no correlations between ARC and the other clinical cardiac risk factors evaluated despite the high prevalence of hypertension and the presence of multiple clinical risk factors in patients with ARC.
There have been conflicting results regarding the association of traditional cardiac risk factors and aortic calcification depending on the specific part of the aorta assessed (ascending, arch, descending, or abdominal aorta), the method used for evaluation of the aorta (X-ray, electron beam computed tomography, cardiac magnetic resonance imaging (MRI), or MDCT) and variations in study designs.
Moreover, we included in our study only patients with coronary atherosclerosis based on the presence of coronary calcification, which may explain our significant correlations, as aortic calcification may precede the development of coronary calcification.10 However, several studies reported no significant association between aortic calcification and clinical risk factors.11–13
In a cohort of asymptomatic older individuals, Chen et al. examined the relationship of aortic atherosclerosis burden to other coronary risk factors using MRI and found no significant associations between standard risk factors or Framingham global risk and descending aortic calcification, suggesting the possibility of different pathways for the progression of aortic atherosclerosis.11 A prospective study by Arai et al. did not detect a correlation between aortic calcification and systolic or diastolic blood pressure.12 Additionally, a study by Kim et al. demonstrated no significant association of diabetes or hypertension with aortic calcification in male subjects or of smoking pattern and aortic calcium score in female subjects.13
An important observation was reported by Owens et al., who found a significant correlation between dyslipidemia and aortic calcification only in a younger age group. Their results suggested that the role of risk factors early in life, rather than later in life, may be more important for future aortic calcification and vascular remodeling.14 Interestingly, the Rotterdam study15 reported that the same cardiac risk factors are present for atherosclerosis in the coronary and aortic circulation even though associations were not consistent across the different vessel beds or for men and women.
It has been suggested that treatments for hyperlipidemia, diabetes, and hypertension may underestimate or mask the association of these risk factors with ARC and that single assessments of cardiac risk factors may not adequately reflect a causal relationship between ARC and cardiac risk factors, suggesting that large prospective community-based studies with repeated measurements of risk factors may be necessary to overcome these limitations.16
Thoracic aortic calcium score has been shown to be independently associated with age ≥65 years and male sex, and abdominal aortic calcium score was shown to be independently associated with age ≥65 years in 315 patients assessed by positron-emission tomography/computed tomography.17 In addition, Takasu et al. found a higher prevalence of ascending aortic calcification in male patients aged 55 years and older.18
Other studies have reported age to be an important determinant of the presence and severity of abdominal aortic calcification. In a literature review carried out by Jayalath et al., no studies could be located that showed a negative or nil correlation between abdominal aortic calcification with age, highlighting the crucial role of age in the pathogenesis and progression of aortic calcification.19 Finally, results of a large cohort study by Iribarren et al. comprising 60,393 women and 55,916 men showed that aortic arch calcification seen on chest radiograph was independently associated with older age, and that this association was more strongly related to coronary artery disease among male subjects aged 65 years and older than among younger male subjects.20
There were several limitations to this study. First, the study was a single-center investigation and the population was not randomly selected, as it involved only patients with CCS >0. There is therefore the possibility of selection bias. Second, the number of patients was relatively small, especially when the study population was divided into subgroups. Third, a causal relationship between cardiac risk factors and ARC cannot be established because of the cross-sectional nature of our study.
Further studies using larger population sizes and including follow-up are needed to establish a causal relationship of cardiac risk factors and ARC. This will facilitate better risk stratification for cardiovascular diseases and help physicians to initiate appropriate interventions earlier, which in turn may arrest the progression of ARC and prevent irreversible changes in arterial hemodynamics.
Conclusion
In patients with CCS > 0, ARC was significantly correlated only with age ≥65 years and male sex. This correlation persisted even after adjustment for other cardiac risk factors.
Conflict of interest
The authors declare that they have no conflicts of interest.
Acknowledgments
There were no external funding sources for this study.
References
Cite this article
TY - JOUR AU - Hasan A. Al-Nafakh AU - Hussein Nafakhi AU - Mohammed Abd Kadhim Al-Jiboori AU - Abdulameer A. Al-Mosawi AU - Raad H. Tawfeq PY - 2015 DA - 2015/02/26 TI - Aortic root calcification and cardiac risk factors in patients with coronary calcium score greater than zero using multidetector computed tomography JO - Artery Research SP - 27 EP - 31 VL - 10 IS - C SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2015.02.002 DO - 10.1016/j.artres.2015.02.002 ID - Al-Nafakh2015 ER -
