Estimates of arterial stiffness and central blood pressure in patients with type 2 diabetes: A comparison of SphygmoCor and Arteriograph
- DOI
- 10.1016/j.artres.2016.08.041How to use a DOI?
- Keywords
- Arterial stiffness; Augmentation index; Central blood pressure; Diabetes; SphygmoCor; Arteriograph; Reproducibility
- Abstract
Background: The Arteriograph is a cuff-based oscillometric device for non-invasive assessment of central systolic blood pressure (cSBP), aortic augmentation index (Aix) and aortic pulse wave velocity (PWV). Reproducibility of Arteriograph measurements and the agreement with SphygmoCor in diabetic patients has never been assessed.
Methods: We compared Arteriograph reproducibility and agreement with SphygmoCor with data from two study populations: Study 1 (n = 17) was conducted in a research laboratory and Study 2 (n = 19) in a catheter lab. SphygmoCor PWV data was only available in study 1.
Results: Reproducibility: Mean differences (±Standard deviation of the difference (SDD)) between duplicate cSBP, Aix and PWV Arteriograph measurements were −0.6 ± 6.6 mmHg, −1.1 ± 3.3% and 0.1 ± 0.5 m/s in study 1 and −0.01 ± 4.3 mmHg, 1.5 ± 3.2% and −0.2 ± 0.6 m/s in study 2, all differences non-significant. Agreement: Mean differences between SphygmoCor and Arteriograph were −14 ± 10 mmHg, −8 ± 7% and 2.4 ± 1.8 m/s, (p < 0.001 for all) in Study 1 and −5 ± 10 mmHg, p = 0.04 and −10 ± 8%, p = <0.001 in Study 2. In study 1, a significant correlation was observed between the mean and the difference for cSBP, r = −0.75, p < 0.001 and for Aix, r = −0.67, p < 0.001.
Conclusions: In type 2 diabetics, Arteriograph data were reproducible yet systematically overestimated cSBP, Aix and PWV compared with SphygmoCor. Hence, the two devices cannot be used interchangeably in type 2 diabetics.
- Copyright
- © 2016 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Introduction
In recent years, pulse wave analysis (PWA) indices and carotid-femoral pulse wave velocity (cf-PWV) have received attention as markers of cardiovascular (CV) risk potentially providing information beyond conventional risk markers.1–3
Patients with type 2 diabetes are characterized by a high CV risk and have been shown to have significantly increased arterial stiffness as evaluated by cf-PWV when compared to non-diabetic individuals.4,5 PWV is an independent predictor of CV mortality in patients with diabetes,6 whereas the added prognostic potential of central blood pressure (BP) and augmentation index (Aix) remains to be determined.
Several devices provide non-invasive measurements of central systolic blood pressure (cSBP), Aix and PWV. The SphygmoCor system (AtCor Medical, Sydney, Australia) was one of the first devices and remains commonly used. The system is based on applanation tonometry and this method is often considered the gold standard. However, the method is time-consuming, and the data acquisition is dependent on a skilled investigator. Recently, the Arteriograph (TensioMed, Budapest, Hungary) has been introduced. The Arteriograph uses a brachial cuff for measurements of cSBP, Aix and PWV based on an oscillometric occlusive method. Thus, using the Arteriograph, information on arterial stiffness indices can be obtained quickly and without investigator training.
The reproducibility of the Arteriograph has been assessed in a hypertensive population,7,8 showing good agreement between measurements. However, the reproducibility of office measurements with Arteriograph in patients with type 2 diabetes has not been assessed. Furthermore, even though Arteriograph and SphygmoCor have been compared in a number of different patient populations8–12 none of the studies have focused on diabetic patients, a high-risk population with potentially different vascular characteristics compared to the other populations.4 Thus, the aim of the present study was to determine the reproducibility of Arteriograph measurements and to assess the agreement between the SphygmoCor and the Arteriograph in patients with type 2 diabetes.
Methods
Patients
We compared data obtained from measurements with Arteriograph and SphygmoCor in two different studies conducted in our research group.
In Study 1, 19 patients with type 2 diabetes were invited to participate. The study was conducted in our research laboratory in connection with screening for participation in a randomised study investigating the effects of bedtime administration of antihypertensive drugs.13 Data on the reproducibility of the SphygmoCor device in this patient sample has previously been published.14 For the current study, two valid consecutive Arteriograph measurements were available in 15 patients. These were used to assess Arteriograph reproducibility. Inter-device agreement was assessed based on the first valid measurement from each device. Paired data on cSBP, Aix and PWV from the Arteriograph and the SphygmoCor devices were available in 17, 17 and 16 patients, respectively.
Study 2 was conducted in the catheter laboratory at the department of cardiology, and included patients with type 2 diabetes referred for elective coronary angiography.15,16 Data regarding the agreement between invasively measured aortic BP and measurements performed with Arteriograph and the SphygmoCor, respectively, have previously been published.15,16 Data regarding PWV was not obtained in this second study. Duplicate Arteriograph measurements were available in 11 patients. The first Arteriograph and SphygmoCor recordings were used to assess inter-device agreement. Paired cSBP and Aix data from the Arteriograph and the SphygmoCor devices were available in 19 patients.
Inclusion and exclusion criteria as well as the recruiting process have previously been described in detail.14–16 The Research Ethics Committee of Central Denmark Region and the Danish Data Protection approved both studies. The studies were conducted in agreement with the Declaration of Helsinki. All patients gave their written informed consent.
SphygmoCor
The PWA measurements in both studies were performed by applanation tonometry at the radial artery using an applanation tonometer (Millar, SPT-301B, Houston, Texas, USA) and the SphygmoCor device software version 8.0 (Study 1) and 8.2 (Study 2) (AtCor Medical, Sydney, Australia) after a minimum of 5 min rest in the supine position. The SphygmoCor was calibrated in both Study 1 and 2 with brachial systolic and diastolic BP as recommended by the manufacturer. Brachial BP was measured using a Riester Champion N automatic blood pressure device (Riester GmbH, Jungingen, Germany). In Study 1, the mean of three BP measurements was used for calibration. In Study 2, the SphygmoCor was calibrated both with one and the mean of three BP measurements.
In Study 1, PWV was also assessed. After a minimum of 5 min of rest in the supine position, sequential electrocardiogram-referenced recordings of the pulse wave at the carotid and the femoral artery determined the carotid-femoral PWV by the tonometer. The transit time was determined by the intersecting tangent algorithm method. The travel distance of the pulse wave was calculated by subtracting the distance from the sternal notch to the carotid measurement site from distance between the sternal notch to the femoral artery recording site.
Arteriograph
Arteriograph (TensioMed, Budapest, Hungary) uses a brachial cuff with a high fidelity sensor to record oscillations at the upper arm. The device makes an initial inflation during which the brachial BP is measured, and immediately thereafter a second inflation occurs, reaching a pressure of 35–40 mmHg above the systolic pressure, which is held for 8 s. During the second inflation, the device records the pressure waves and uses them to calculate cSBP, Aix and PWV.
Arteriograph calculates cSBP on the basis of the brachial diastolic and mean arterial BP (considered equal to the aortic values) and the aortic Aix, which is calculated from brachial Aix based on an empiric correlation.17 The brachial Aix, is calculated using the formula Aix= ((P1–P2)/PP) × 100 where P1 is the amplitude of the direct and P2 the amplitude of the reflected wave and PP is the pulse pressure.17
PWV is calculated using the time difference between the two systolic peaks in the pulse waveform. The first peak is the direct pulse wave generated by the cardiac systole, and the second peak is the reflected wave. For calculation of travel distance, the site of wave reflection is assumed to be the aortic bifurcation, and the distance is estimated by measuring the distance from the jugular notch to the pubic symphysis. Hence, the formula for PWV is: PWV (m/s) = jugular-symphysis distance (m)/((travel time)/2).
Using the brachial circumference, the appropriate cuff was chosen according to the manufacturer’s instructions. Software version 3.0.0.0 was used.
Statistical analysis
Data distribution was assessed by histograms and QQ-plots. Normally distributed data are presented as mean values ± standard deviation (SD) and skewed data as median (range). Agreement between intra- and inter device variation was assessed by Bland–Altman analysis.18 Intra- and inter-device differences were assessed by paired t-tests and are reported as mean difference ± standard deviation of the difference (SDD). Correlation was assessed by Pearson’s correlation coefficient. Data analyses were performed using Stata software (Stata 14, StataCorp LP, Texas, USA).
Results
Patient characteristics
The patient characteristics are shown in Table 1. No significant differences were observed between the two study groups regarding sex, age, duration of diabetes, systolic and diastolic BP or antidiabetic medicine. A higher proportion of patients in study 2 received beta-blocking agents, whereas the distribution of other antihypertensive agents was comparable in the two studies.
| Parameter | Mean (SD)/median (range) | p | |
|---|---|---|---|
| Study 1 | Study 2 | ||
| N | 17 | 19 | |
| Male sex (n (%)) | 13 (76) | 14 (74) | 0.58 |
| Age (years) | 64 ± 8 | 67 ± 10 | 0.30 |
| Diabetes duration (years since diagnosis) | 9 (2–44) | 9 (0–31) | 0.69 |
| HbA1c (mmol/mol) | 54 (37–100) | 51 (36–99) | 0.95 |
| Body mass index (kg/m2) | 30 ± 4 | 30 ± 4 | 0.95 |
| Tobacco use (never/previous/present) (n (%)) | 6/10/1 (35/59/6) | (3/8/7) (17/44/39)c | 0.64 |
| Brachial systolic BP (mmHg)a | 136 ± 9 | 140 ± 17 | 0.34 |
| Brachial diastolic BP (mmHg)a | 80 ± 9 | 79 ± 13 | 0.83 |
| Total P-cholesterol (mmol/l) | 3.8 ± 0.7 | 3.8 ± 0.9 | 0.92 |
| P-creatinine (mikromol/l) | 74 (55–146) | 78 (48–524) | 0.51 |
| Anti-diabetic treatment (n (%)) | |||
| -Oral anti-diabeticsb | 15 (88) | 17 (89) | 1.00 |
| -Insulin | 3 (18) | 7 (37) | 0.27 |
| -Glucagon-like peptide 1 (GLP-1) agonist | 4 (24) | 2 (11) | 0.39 |
| Lipid lowering therapy (n (%)) | 15 (88) | 17 (89) | 1.00 |
| Antihypertensive treatment (n (%)) | |||
| Beta-blocker | 5 (29) | 12 (64) | 0.04 |
| ACE-inhibitor/ARB | 17 (100) | 18 (94) | 0.21 |
| CCB | 8 (47) | 9 (47) | 0.99 |
| Diuretics | 12 (71) | 12 (63) | 0.64 |
| Central systolic BP, Arteriograph | 138 ± 18 | 132 ± 17 | 0.37 |
| Central systolic BP, SphygmoCor | 123 ± 11 | 127 ± 20 | 0.49 |
| Aortic augmentation index, Arteriograph | 30 ± 15 | 33 ± 11 | 0.50 |
| Aortic augmentation index, SphygmoCor | 22 ± 10 | 23 ± 10 | 0.84 |
| Pulse wave velocity, Arteriograph (m/s)d | 8.2 ± 1.7 | 9.1 ± 1.2 | 0.14 |
| Pulse wave velocity, SphygmoCor (m/s) | 10.7 ± 2.3 | NA | |
BMI; body mass index, HDL; high density lipoprotein, LDL; low density lipoprotein, ACE-inhibitor: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; CCB; calcium channel blocker. Some patients received more than one antihypertensive drug.
Brachial BP; mean of 3 BP measurements.
Oral antidiabetics: metformin and/or sulphonylureas and/or dipeptidyl peptidase 4 inhibitors.
n = 18.
Study 2: n = 11.
Patient characteristics.
Reproducibility of Arteriograph measurements
Study 1: The mean difference (±SDD) in cSBP, Aix and PWV were −0.6 ± 6.6 mmHg, p = 0.73, −1.1 ± 3.3%, p = 0.20 and 0.1 ± 0.5 m/s, p = 0.31, respectively (Fig. 1, upper panel). No significant correlation was observed between the mean and the difference of the measurements.
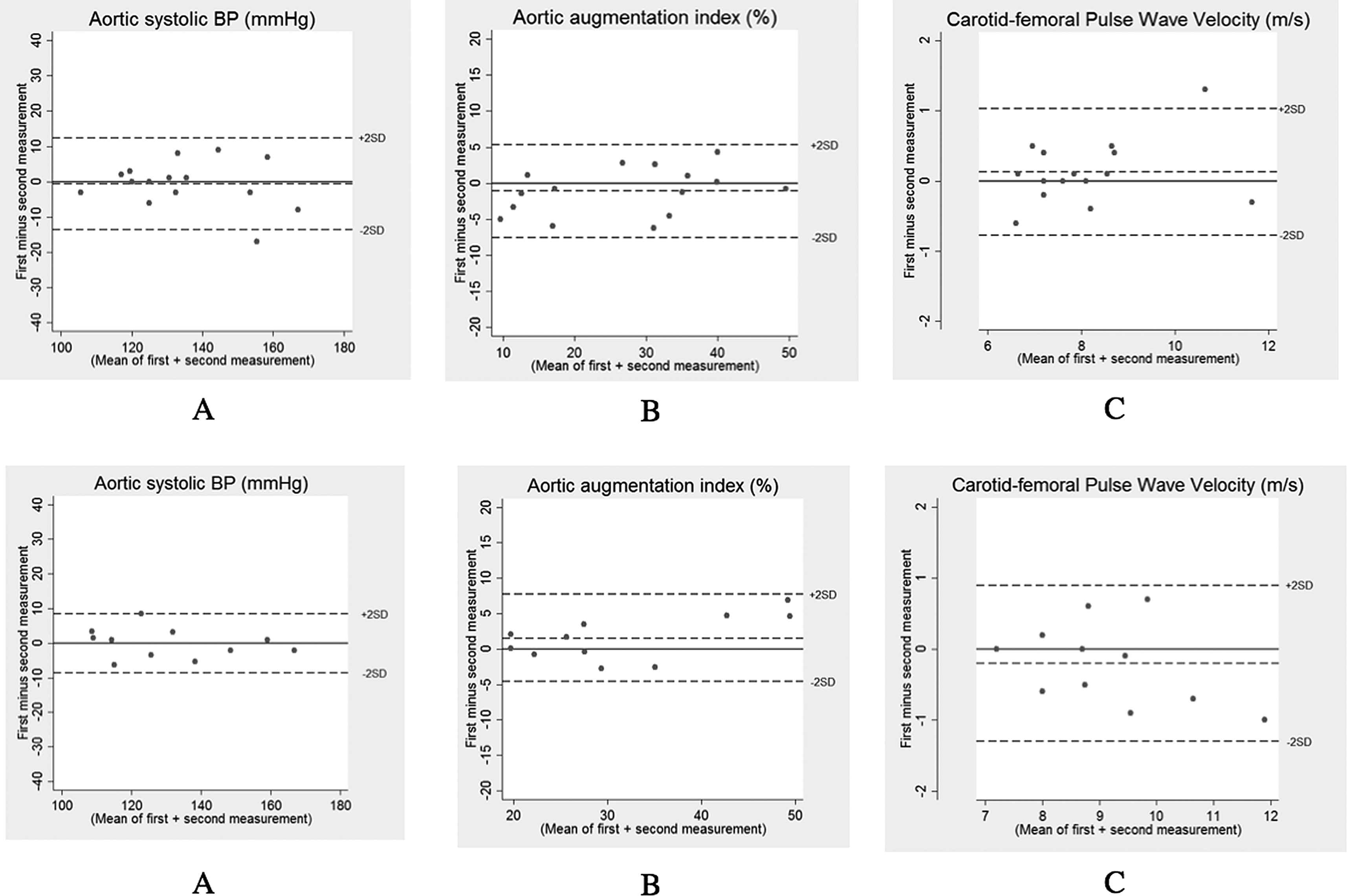
Reproducibility of Arteriograph measurements. Upper panel: study 1. Lower panel: study 2. Panel A: central systolic BP. Panel B: augmentation index. Panel C: pulse wave velocity.
Study 2: The mean difference in cSBP, Aix and PWV were −0.01 ± 4.3 mmHg, p = 0.96, 1.5 ± 3.2%, p = 0.14 and −0.2 ± 0.6 m/s, p = 0.26 (Fig. 1, lower panel). No significant correlation was observed between the mean and the difference of the measurements except for Aix, r = 0.61, p = 0.047.
Comparison of Arteriograph and SphygmoCor
Inter-device variation was evaluated by comparing the first Arteriograph measurement and the first SphygmoCor measurement.
Study 1
The mean difference in cSBP (SphygmoCor minus Arteriograph) was −14 ± 10 mmHg, p < 0.001 (Fig. 2A). A significant correlation between the difference in cSBP and the mean cSBP was observed, i.e. the cSBP estimates of the Arteriograph became increasingly higher as compared to the SphygmoCor as mean BP increased, r = −0.75, p < 0.001.
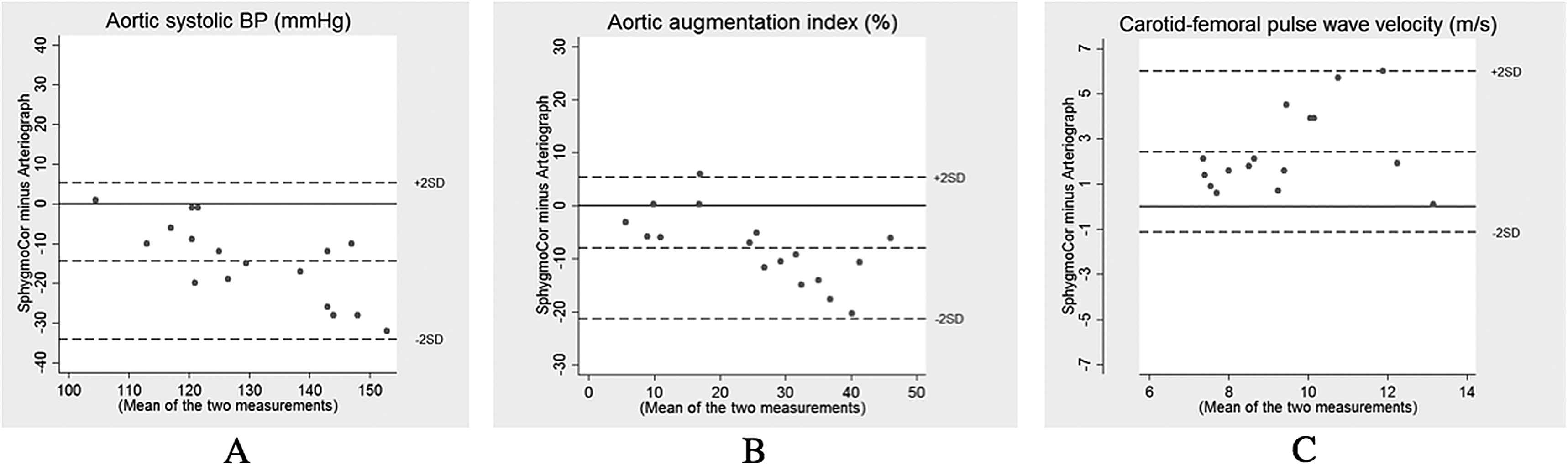
Inter-device variation in study 1. Panel A: central systolic BP. Panel B: augmentation index. Panel C: pulse wave velocity.
The mean difference in Aix (SphygmoCor minus Arteriograph) was −8 ± 7%, p < 0.001 (Fig. 2B). A significant correlation between the Aix differences and the mean Aix was observed, r = −0.67, p < 0.001. The mean difference in PWV (n = 16) (SphygmoCor minus Arteriograph) was 2.4 ± 1.8 m/s, p < 0.001 (Fig. 2C). A non-significant correlation between the PWV difference and the mean PWV was observed, r = 0.33, p = 0.21.
Study 2
The mean difference in cSBP (SphygmoCor minus Artheriograph) was −5 ± 10 mmHg, p = 0.04 (Fig. 3A). No significant correlation between the cSBP difference and the mean cSBP was observed, r = 0.29, p = 0.23.
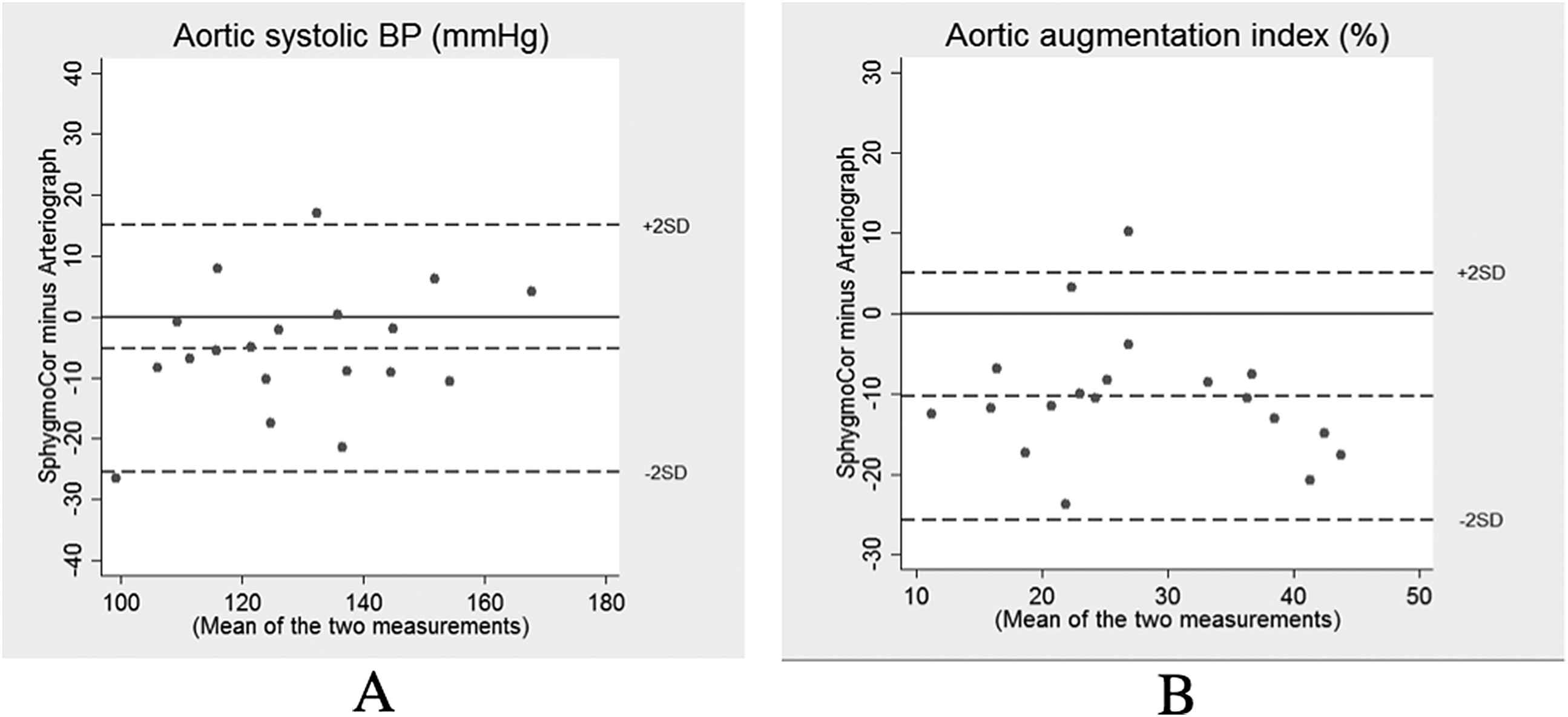
Bland–Altman plot: Inter-device variation in study 2. Panel A: central systolic BP. Panel B: augmentation index.
When the SphygmoCor was calibrated with the mean of three brachial systolic and diastolic BP, the mean difference in cSBP (SphygmoCor minus Artheriograph) was −6 ± 8 mmHg, p = 0.004, r = −0.001, p = 1.00.
The mean difference in Aix was −10 ± 8%, p < 0.001. No correlation between the Aix difference and the mean Aix was observed, r = −0.11, p = 0.68.
Bland–Altman plots are shown in Fig. 3.
The correlation between systolic BP differences and underlying mean BP in study 1 (r = 0.75) was significantly higher than the correlation observed in study 2 (r = −0.11), p < 0.001, whereas the correlation between Aix differences and mean Aix in study 1 (r = −0.67) and 2 (r = −0.11) were not significantly different, p = 0.056.
The difference between estimated and invasively measured aortic systolic BP was comparable in the SphygmoCor and the Arteriograph with a difference between the two devices of 3 ± 9 mmHg, p = 0.11.
Discussion
PWV, central BP and Aix are receiving increasing attention as potential novel markers of cardiovascular events. Several devices for non-invasive measurements have been marketed. In this study we assessed the reproducibility of the Arteriograph device and the agreement with the SphygmoCor in two diabetic populations.
The overall finding in this study was a good reproducibility of measurements using the Arteriograph. However, we found significant differences between Arteriograph and SphygmoCor. In Study 1, the Arteriograph gave higher estimates of cSBP and Aix than the SphygmoCor. Furthermore, the difference between the two devices increased at higher values of cSBP and Aix. Similarly, the Arteriograph gave systematically lower estimates of PWV compared to the SphygmoCor.
In Study 2, a systematic difference between the two devices was also observed. In this study, no trend towards greater differences at higher values was observed for cSBP and Aix.
A number of studies comparing Arteriograph and SphygmoCor have been conducted. A study in hypertensive patients8 showed good correlation between measurements obtained by Arteriograph and SphygmoCor, but poor agreement and wide limits of agreement. In a study on healthy individuals,11 the Arteriograph recorded higher values of cSBP as compared to the SphygmoCor. A close correlation was observed between Aix values obtained by Arteriograph and SphygmoCor, but the Arteriograph systematically recorded higher Aix values. A good agreement was seen regarding PWV in the low range, but significant differences were observed for higher values.
A study examining 1012 persons recruited for an epidemiological study, showed overall good correlation between Arteriograph and SphygmoCor.19 However, further analysis of the data identified three distinctive clusters of data according to age and diastolic BP characteristics of the participants. The measurements varied greatly between the different patient clusters where the best agreement between the two devices was found for brachial Aix and cSBP in younger participants.
In a study including 35 males,20 the authors found results similar to those we found in Study 1, i.e. higher values of cSBP and Aix obtained with Arteriograph compared with the SphygmoCor with an increasing difference at higher values. When the SphygmoCor was calibrated using mean and diastolic BP instead of systolic and diastolic BP the differences were greatly reduced and narrower limits of agreement were obtained.
A study performed on elderly patients, median age 72.5 years,12 showed results similar to those obtained in our Study 1, with higher Arteriograph-derived estimates of cSBP and Aix, and lower values of PWV, the latter only in patients with SphygmoCor PWV > 12 m/s. The difference between the devices in Ref. [12] widened with increasing age and arterial stiffness.
To the best of our knowledge, we are the first to compare Arteriograph with SphygmoCor in patients with type 2 diabetes. We examined two groups in the same population, and as in previous studies we found significant differences between the two devices.
The differences in cSBP observed when comparing the Arteriograph and SphygmoCor in study 1 could potentially have been due to differences in the brachial BP used for calibration. However, a post-hoc analysis showed that the brachial BPs from the two oscillometric devices (Riester and Arteriograph) were not significantly different. Furthermore, our results did not change when we used the brachial BP from Arteriograph to calibrate the SphygmoCor. The differences in PWV could potentially be influenced by the distance measurement, as SphygmoCor PWV was calculated using the subtracted distance method. However, post-hoc recalculation of the SphygmoCor PWV using 0.8*the estimated direct carotid-femoral distance as described by Vermeersch et al.21 tended to increase the SphygmoCor minus Arteriograph difference (2.9 ± 1.9 m/s, p < 0.001).
Regarding PWV, several explanations for the observed inter-device differences in previous studies have been explored. Rajzer et al.10 compared three different devices and found a significant difference in the measured travelled length of the pulse wave of 0.05 m between SphygmoCor and Arteriograph when the Arteriograph was calibrated with the distance from the sternal notch to the pubic symphysis and the SphygmoCor was calibrated with the distance from the sternal notch to the carotid artery subtracted from the distance between the sternal notch and the femoral artery. However, this significant difference in travel distance did not result in significant differences in PWV between Arteriograph and SphygmoCor.
Based on a numerical model of the arterial tree, Trachet et al.22 argued that the pressure waveforms recorded by the Arteriograph origins from wave reflections in the brachial artery rather than reflection from the aortic bifurcation, and this may be the reason for the observed differences. Overall, the causes underlying the discrepancy between Arteriograph and SphygmoCor cSBP, Aix and PWV remain undetermined.
The reason for the increasingly greater differences in estimated cSBP at higher mean values in Study 1, but not in Study 2, is unclear. The study populations were very similar and the same devices were used in both studies. The examination conditions varied, Study 1 being performed in our research lab and Study 2 in the catheter lab. Selection bias could potentially influence the results in study 2, as Arteriograph data were not recordable in 12 patients with SphygmoCor data.15,16 If Arteriograph data were missing preferentially in patients with high BP, this could induce bias. However, a post-hoc analysis of the patients in Ref. [15, 16] showed that brachial calibration BP, obtained by the Riester BP monitor, were not significantly different in patients with and without Arteriograph data. Three BP were used for calibration of the SphygmoCor in Study 1. The Arteriograph is calibrated with one BP. Hypothetically, regression towards the mean could thus potentially contribute to the observed correlation between mean and difference when comparing the SphygmoCor and the Arteriograph in Study 1. However, post-hoc recalibration of the SphygmoCor with BP from the Arteriograph did not affect our findings. Moreover, no significant correlation was observed between the difference and the mean for the SphygmoCor and Arteriograph in Study 2, neither when the SphygmoCor was calibrated with one or three BP. In two of the previous studies a similar tendency of increasing difference at higher values seems to be present.12,20 It is interesting that our results from study 1 are comparable with results obtained from a group of much older non-diabetic patients.12 This may be due to accelerated vascular ageing in diabetic patients making their CV physiology similar to that of elderly people.
Both the Arteriograph and the SphygmoCor have previously been validated.15,16,23 Yet, in our study we found that in a diabetic population the measurements obtained by tonometry and oscillometry were not comparable.
Based on our findings, the Arteriograph systematically overestimates cSBP and Aix and underestimates PWV compared with the SphygmoCor. We also found that the difference in measurements seemed to change with the examination environment, since we observed different degrees of agreement in the two studies despite of quite similar study populations.
In conclusion, our data indicate that the two techniques cannot be used interchangeably in patients with type 2 diabetes. This is in agreement with the results of the previous studies comparing the two devices. Furthermore this could imply that the widely used cut-off PWV value for increased CV risk of 10 m/s is device-specific and thus may not be feasible as a common reference value.
Funding
This work was supported by University of Aarhus, Denmark; Regional Hospital Silkeborg, Denmark; Ministry of Science, Technology and Innovation, Denmark; The Health Research Fund of Central Denmark Region; The Danish Diabetes Association; and The Danish Diabetes Academy supported by the Novo Nordisk Foundation.
Conflicts of interest
None.
References
Cite this article
TY - JOUR AU - Christoffer Krogager AU - Niklas B. Rossen AU - Klavs W. Hansen AU - Søren T. Knudsen AU - Christian D. Peters AU - Hans Erik Bøtker AU - Per L. Poulsen AU - Esben Laugesen PY - 2016 DA - 2016/09/24 TI - Estimates of arterial stiffness and central blood pressure in patients with type 2 diabetes: A comparison of SphygmoCor and Arteriograph JO - Artery Research SP - 18 EP - 24 VL - 16 IS - C SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2016.08.041 DO - 10.1016/j.artres.2016.08.041 ID - Krogager2016 ER -
