Carotid extra-media thickness increases with age, but is not related to arterial stiffness in adults
- DOI
- 10.1016/j.artres.2017.12.003How to use a DOI?
- Keywords
- Adventitia; Imaging; Ultrasound; Carotid wall thickness; Cardiovascular risk; Coronary artery disease
- Abstract
Background: Assessment of carotid artery perivascular adipose tissue through carotid artery extra-media thickness (EMT) ultrasonography has emerged as a novel assessment technique that might contribute unique information to comprehensive evaluations of arterial health. Currently, there is a lack of research examining relationships between EMT and existing measures of arterial health in adults. We investigated the relationships between EMT and established measures of arterial health, including aortic pulse wave velocity (aPWV), carotid distensibility, and intima-media thickness (IMT) in adults.
Methods: Using a cross-sectional, observational design, we assessed resting aPWV, carotid distensibility, IMT and EMT in 81 participants who were categorized as younger healthy adults (YHA; n = 51; 25 ± 6 years), older healthy adults (OHA; n = 15; 70 ± 5 years) or older adults with coronary artery disease (CAD; n = 15; 68 ± 9 years).
Results: EMT, IMT, and aPWV were higher while carotid distensibility was lower in OHA and CAD versus YHA (P < 0.05). EMT was correlated with age (r = 0.48; P < 0.01), aPWV (r = 0.43; P < 0.01), IMT (r = 0.41; P = 0.01), and distensibility (r = −0.37; P < 0.01). Despite significant correlations, EMT was not an independent predictor of any of the traditional measures of arterial health included in this study.
Conclusions: The novel finding of this study is that while EMT is elevated in older versus younger adults, in agreement with established indicators of arterial health, it is not a predictive factor in these existing measures. EMT may, however, still have clinical utility as a target for comprehensive monitoring of interventions specifically designed to impact arterial structure and function.
- Copyright
- © 2018 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Introduction
Cardiovascular disease, and more specifically, atherosclerosis and hypertension, dominate other pathologies as major contributors to death and disability, with a projected number one ranking for mortality by 2020.1 Hence, the study and analysis of the human cardiovascular system is vital to identify strategies to ameliorate this increasing burden. Many previous studies examining the development and progression of arterial dysfunction have focused on the quantification of the thickness of the inner layers of the common carotid artery wall, termed the carotid artery intima-media thickness (IMT),2 and have highlighted the predictive capacity of subclinical IMT thickening in individuals at risk for future cardiovascular events.3
While the carotid inner wall layers have been extensively examined, the assessment of the outer adventitia layer and the surrounding adipose tissue has been neglected. Preliminary studies suggest that the adventitial layer may be involved in the early pathogenesis of atherosclerosis and other arterial pathologies.4,5 Changes in the adventitial layer may occur before measurable pathological development in the intimal and medial layers,6–9 thereby leading to the development of subclinical manifestation of cardiovascular disease such as the stiffening of the central elastic arteries. However, as the border between the adventitia and surrounding tissues is indiscernible with standard imaging modalities, there are currently no techniques available to quantify the thickness of the adventitia alone. Alternatively, measurement of carotid artery extra-media thickness (EMT), which encompasses the thickness of the adventitial layer, as well as the perivascular adipose tissue and venous wall, may be useful in assessment of the early pathogenesis of atherosclerosis.10 EMT has been shown to have an independent relationship with traditional cardiovascular risk factors such as age and blood pressure, and has been proposed to mostly reflect adventitial thickness in older adults.11 Furthermore, EMT may be more feasible to assess in routine clinical examination as it only requires ultrasound imaging in the area of the carotid artery rather than the more complex assessments currently available for arterial stiffness.
Previous research indicates that aging and the presence of coronary artery disease (CAD) are negatively associated with measures of arterial health such as aortic pulse wave velocity (aPWV), carotid distensibility and IMT.12–14 While the link between EMT and subclinical vascular health, as indicated by the association between EMT and distensibility, has been demonstrated in children15 and young adults,16 these relationships have not been examined in adults. Therefore, the current study examines the relationships between EMT and traditional measures of arterial health, notably, aPWV, carotid distensibility, and IMT. We aimed to examine these relationships in both younger healthy adults, older healthy adults, and older adults with CAD. We hypothesized that older adults with CAD will have thicker EMT versus older healthy adults, with both older groups having thicker EMT than younger adults. We also hypothesized that EMT will be an independent predictor of aPWV, carotid distensibility, and IMT.
Methods
Participants and ethical approval
Eighty-one participants were recruited to take part in this cross-sectional observational study. The three populations included: younger healthy adults (YHA; n = 51; 25 ± 6 years), older healthy adults (OHA; n = 15; 70 ± 5 years) and older adults with coronary artery disease (CAD; n = 15; 68 ± 9 years). The inclusion and exclusion criteria for our CAD participants follow the guidelines from the New York Heart Association.17 All participants gave verbal and written consent prior to participation in the study. The study protocols were approved by the Hamilton Integrated Research Ethics Board and conform to the Declaration of Helsinki concerning the use of human subjects as research participants.
Study design
Participants were invited for a single visit to the Vascular Dynamics Laboratory in the Department of Kinesiology at McMaster University, Canada. After anthropometric measures were taken, participants were asked to rest in the supine position in a quiet, temperature-controlled room for 10 min. Following this rest period, four brachial artery blood pressure measurements were taken using an automated oscillometric blood pressure unit (Dinamap Pro 100, Critikon LCC, Tampa, Fla, USA). The first blood pressure measurement was discarded,18 and the average of the last three measurements was recorded. Continuous measurements of single-lead ECG and reconstructed brachial artery blood pressure waveforms from finger cuff plethysmography (Finometer MIDI, Finapres Medical Systems BV, Amsterdam, The Netherlands) were obtained simultaneously using a data acquisition system (Powerlab model ML795; ADInstruments, Colorado Springs, CO, USA), with a corresponding software program (Labchart 7; ADInstruments Inc., Colorado Springs, CO, USA).
Pulse wave velocity
The measurement of aortic stiffness was obtained through the measurement of carotid to femoral PWV, according to the latest standard guidelines.19 The equation for aPWV is as follows:
The time difference between the arrival of arterial pressure waveforms from the right carotid and right femoral arteries was denoted as the pulse transit time and measured using simultaneous applanation tonometry (model SPT-301; Millar Instruments, Houston, TX, USA). The tonometry signals were continuously processed with a band pass filter (5–30 Hz) to identify the foot of the waveforms.20 The distance between pulse measurement sites was estimated using a direct surface measurement with a non-elastic tape measure. Two sets of 10 waveforms were taken, and used to calculate the average pulse transit time for each set. If there was a difference of 0.5 m/s or greater between the two aPWV calculations, a third set of 10 waveforms was taken.
Carotid distensibility
Carotid artery stiffness was estimated from the determination of carotid distensibility. The calculation of carotid distensibility is as follows:
Carotid intima media thickness
The measurement of IMT was performed using B-mode ultrasonography (frequency: 13 MHz, frame rate: 40 fps, depth: 3.0 cm) on the far wall of the right carotid artery. A single 30 s video loop was saved in the DICOM (Digital Image and Communications in Medicine) format in a picture archiving and communication system (EchoPAC Clinical Workstation System 110.0.2; GE Medical Systems, Horten, Norway). End-diastolic IMT was determined using a semi-automated edge tracking software (Artery Measurement System Image and Data Analysis; Tomas Gustavsson; Gothenburg, Sweden) to analyze the frames acquired from the ultrasound imaging.23 At the end-diastolic image frame, a mean IMT measurement was displayed from an average distance between 100 points across the region of interest. A total of 10 end-diastolic frames were measured and the average of these 10 values each representing 100 individual IMT data points was reported for the IMT measurement.
Carotid extra media thickness
B-mode ultrasonography (frequency: 13 MHz, frame rate: 40 fps, depth: 3.0 cm) was performed on the right neck region in which the acoustic window included, from superficial to deep: the jugular vein lumen, jugular vein wall, perivascular adipose tissue, carotid adventitia, media, intima, and lumen. End-diastolic frames were extracted and compiled in one DICOM file (Sante DICOM Editor 3.1.13, Santescroft, Athens, Greece) and post-processed by inverting the gray scale. By inverting the shades of gray, the EMT is represented as dark and anechoic, allowing the edge tracking software to easily detect the borders (Artery Measurement System Image and Data Analysis; Gothenburg Sweden). A total of 10 end-diastolic frames were compiled and measured in a region of interest with 100 discrete measurement sites. The average EMT was calculated per frame and a total of 10 frames were averaged to produce the EMT measurements for each individual.
Statistical analysis
The Shapiro–Wilk test was used to determine normality of the variables and was confirmed with histogram plots. Age, SBP, DBP, MAP, aPWV, carotid distensibility and IMT were not normally distributed and were log-transformed for analysis. Age, DBP, MAP and IMT remained non-normal after transformation and therefore non-parametric tests were used to assess group differences in these variables. To determine group differences in arterial stiffness (aPWV, carotid distensibility) and wall thickness (IMT, EMT), we employed a one-way, between group analysis of variance with Tukey’s HSD post hoc tests (non-parametric Kruskal–Wallis with Mann Whitney U post hoc tests for Age, DBP, MAP and IMT). Relationships between EMT and aPWV, carotid distensibility, and IMT were assessed with Pearson’s r correlation (Spearman rank correlation with non-normal variables). To determine if EMT was a predictor of arterial health separate multiple regression analyses with a backward model was performed with aPWV, carotid distensibility, and IMT as dependent variables. A conservative deletion criterion of 0.5 was used for the backward model.24 Variables used for the aPWV model included EMT as the novel variable as well as age, sex, weight, height, SBP, DBP, and IMT, as they have been previously established to influence and affect arterial stiffness.25 In the model that predicts carotid distensibility, brachial blood pressures were excluded from the previous list because these variables are involved in the calculation of carotid distensibility. In modeling IMT, EMT was included as the novel variable in addition to age, sex, weight, height, SBP, and DBP, as these factors have been previously shown to influence the IMT.26 All statistical analyses were performed with SPSS software (SPSS 23 IBM, Armonk, NY, USA) with a minimum criterion alpha level of α = 0.05 to determine statistical significance.
Results
Participant characteristics and vascular outcome measures are reported in Table 1. Between the OHA and CAD groups, there were no differences in age, weight, height, resting heart rate, and brachial artery blood pressures (P > 0.05). There were differences in age (P < 0.05) and brachial artery blood pressures (P < 0.05) between the younger and older groups. Compared to YHA, both the OHA and CAD groups had higher aPWV, lower carotid distensibility, thicker IMT, and thicker EMT (P < 0.05) (Table 1).
| Young adults | Old healthy adults | Old adults with CAD | |
|---|---|---|---|
| Gender (M/F) | 38/13 | 8/7 | 15/0 |
| Age, yrs | 24.8 ± 5.5 | 70.7 ± 5.4a | 67.9 ± 8.7a |
| Height, m | 1.74 ± 0.09 | 1.69 ± 0.1 | 1.75 ± 0.06 |
| Mass, kg | 74.9 ± 18.2 | 78.7 ± 13.8 | 84.6 ± 16.4 |
| Body mass index, kg/m2 | 24.4 ± 4.3 | 28.3 ± 4.9a | 27.7 ± 5.2a |
| Resting heart rate, bpm | 62 ± 10 | 59 ± 9 | 53±8a |
| Resting systolic blood pressure, mmHg | 114 ± 9 | 129 ± 20a | 131 ± 23a |
| Resting diastolic blood pressure, mmHg | 67 ± 5 | 74 ± 12a | 76 ± 10a |
| Resting mean arterial pressure, mmHg | 86 ± 5 | 95 ± 14a | 99 ± 14a |
| aPWV, m/s | 6.2 ± 1.1 | 9.5 ± 2.7a | 9.9 ± 2.6a |
| Carotid distensibility, mmHg−1 | 5.9e−3±1.9e−3 | 3.4e−3±1.3e−3a | 3.2e−3±1.1e−3a |
| Intimal media thickness, mm | 0.50 ± 0.05 | 0.79 ± 0.1a | 0.84 ± 0.11a |
| Extra media thickness, mm | 0.47 ± 0.08 | 0.58 ± 0.06a | 0.54 ± 0.08a |
Values are represented as means ± SD.
aPWV = aortic pulse wave velocity.
P < 0.05 compared to young adults.
Participant characteristics and vascular outcome measures.
Association between EMT and measures of arterial health
Correlation analyses were conducted to determine the relationship between EMT, measures of arterial health and other known cardiovascular disease risk factors. EMT was significantly correlated with age (ρ = 0.48, P < 0.01), aPWV (r = 0.46, P < 0.01), IMT (ρ = 0.41, P < 0.01), and distensibility (r = −0.37, P < 0.01) (Table 2). Figure 1 demonstrates the linear relationship between EMT and measures of vascular health.
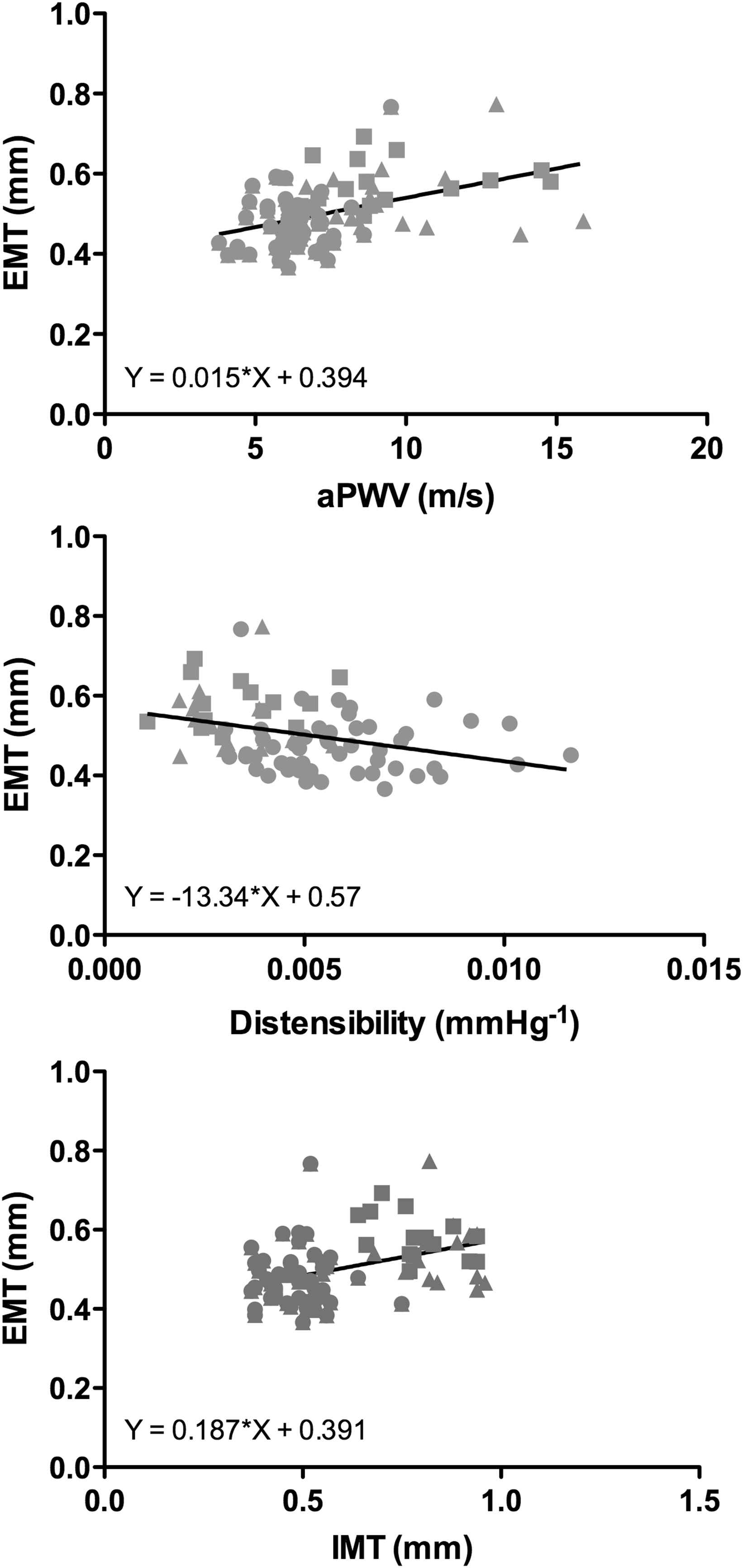
Scatterplots of the linear relationships between extra-media thickness (EMT) and vascular measures (aortic pulse wave velocity (aPWV), carotid distensibility, and carotid intima-media thickness (IMT)) for pooled analysis with younger adults (circles), older adults (squares) and older adults with coronary artery disease (triangles). Simple regressions of EMT and measures of arterial stiffness are also displayed.
| r | P-value | |
|---|---|---|
| Age | 0.48a | <0.01 |
| Body mass index | 0.26 | 0.02 |
| Resting heart rate | −0.25 | 0.02 |
| Resting Systolic Blood Pressure | 0.24 | 0.04 |
| Resting diastolic blood pressure | 0.22a | 0.05 |
| Resting mean arterial pressure | 0.23a | 0.04 |
| aPWV | 0.46 | <0.01 |
| Carotid distensibility | −0.37 | <0.01 |
| Intimal media thickness | 0.41a | <0.01 |
aPWV = aortic pulse wave velocity.
Spearman’s correlation (ρ).
Correlations with EMT for pooled sample.
In addition, we performed multiple regression analyses to determine if EMT is an independent predictor of aPWV, carotid distensibility, and IMT (Table 3). In a backwards model to predict aPWV, age (β = 0.58, P < 0.01) and SBP (β = 0.35, P < 0.01) were significant predictors. Although EMT was included in the final model, it was not a significant independent predictor (β = 0.07, P = 0.37) of aPWV. For the carotid distensibility model, age (β = −0.55, P < 0.01) and height (β = 0.31, P = 0.02) were significant predictors, while EMT did not meet the criteria to be included in the final model. For the IMT model, age (β = 0.43, P < 0.01) was the only significant predictor, while EMT was not included in the final model.
| Predictor variable | β | t | P |
|---|---|---|---|
| aPWV model: F[6,73] = 30.204, P < 0.01, R2 = 71.3% | |||
| Age | 0.58 | 7.10 | <0.01 |
| Sex | −0.12 | −1.46 | 0.15 |
| Weight | −0.07 | −0.83 | 0.41 |
| Height | 0.07 | 0.79 | 0.44 |
| SBP | 0.35 | 4.49 | <0.01 |
| EMT | 0.07 | 0.91 | 0.37 |
| Carotid distensibility model: F[4,75] = 14.003, P < 0.01, R2 = 42.8% | |||
| Age | −0.55 | −5.90 | <0.01 |
| Sex | 0.20 | 1.77 | 0.08 |
| Weight | −0.09 | −0.78 | 0.44 |
| Height | 0.31 | 2.41 | 0.02 |
| IMT model: F[3,76] = 61.173, P < 0.01, R2 = 70.7% | |||
| Age | 0.43 | 11.18 | <0.01 |
| SBP | 0.01 | 1.79 | 0.08 |
| DBP | −0.20 | −0.91 | 0.37 |
aPWV = aortic pulse wave velocity; EMT = extra medial thickness; DBP diastolic blood pressure; SBP = systolic blood pressure.
Final multiple regression models predicting aPWV, carotid distensibility and IMT.
Discussion
The current study is the first to make the direct comparison of EMT between younger healthy adults, older healthy adults, and older adults with CAD. Similar to traditional measures of arterial health, we found that EMT was different between the younger and older groups, with no additional difference in either EMT or measures of arterial health between older adults and older adults with CAD. While EMT increases with age similar to established measures of arterial stiffness and IMT, it does not appear to be related to these arterial health indicators when controlling for the independent effects of age or other known risk factors. Rather, EMT may represent an independent yet parallel progression of atherosclerosis associated with the adventitia that occurs coincident with the development of arterial stiffness and thickening of the intima media.
Reference values for aPWV27 and carotid distensibility28,29 show a clear increase in arterial stiffness with age. In agreement, we observed increases in arterial stiffness in older adults compared to younger adults, as well as a strong predictive effect of age in our regression models. Previous investigations in healthy adults and adults with CAD have focused on the thickness of the intima-media layer, with large population studies demonstrating the strong cross-sectional relationship with cardiovascular disease endpoints.30–32 While IMT increases with age similar to arterial stiffness,33 little is known about EMT across the different age groups. The EMT values of our older participants were similar to those reported previously,11 and we have added to these findings to show that EMT is thicker in older adults than in younger healthy adults. Previous literature has suggested that increases in EMT could be attributed to increased adventitial vasa vasorum neovascularization,34 and adventitial remodeling due to an increase in cellular components, extracellular matrix9 and adventitial dysfunction.35 As the measurement of EMT is relatively novel, further work should examine any relationships between EMT progression with age and cardiovascular disease endpoints among older adults.
We did not observe the predicted differences in EMT or other vascular health indices between the OHA and CAD groups. Although previous work has identified a relationship between the severity of CAD and arterial stiffness,13 the group differences in the current study could be compounded by the effects of other cardiovascular risk factors on vascular wall health. One study suggests that arterial stiffness is not a significant predictor of CAD in the presence of other clinical states, including an increased BMI.36 Previous research suggests that there is an association between body composition and EMT in both children,37 and young adults.16 Both cohorts of OHA and CAD in the current study had a mean BMI of greater than 25, which could potentially explain the diminished ability to detect group differences in IMT, EMT or arterial stiffness. In addition, the CAD group in our study were not asked to stop taking their regular prescription medication for participation in this study. One of the most common medications among this group was Lipitor, or atorvastatin, which has been shown to inhibit adventitial neovascularization, potentially limiting the progression of thickening of EMT in the presence of cardiovascular disease.38 Atorvastatin also works to inhibit plaque development, which could explain the lack of group differences between OHA and CAD in IMT in the current study.38
In the current study, correlational analyses revealed significant relationships between EMT and all of aPWV, carotid distensibility, and IMT; however, when the effect of age and anthropometrics were accounted for in regression models, EMT was not predictive of any of these arterial health indicators. These findings contrast previous findings in children15 and young adults,16 which have demonstrated relationships between arterial stiffness and EMT; however, these studies specifically focused on the relationship between EMT and arterial stiffness in a narrow age range. Aging is a complex process, which is affected by many changes in physiological function including increases in oxidative stress,39 development of chronic systemic inflammation,39 and adipose tissue dysfunction.40 While EMT may be related to arterial stiffness in the early years of life, the combination of aging, arterial stiffness development and IMT thickening could lessen the influence of EMT on arterial stiffness.
Limitations
The current study employed a cross-sectional design, limiting the conclusions that can be drawn related to the aging process. Because EMT is a novel measurement, future studies would need to also focus on validating measurement reliability with a larger sample size. Future studies should also include more female participants to consider any sex-related factors, as well as expand investigation into patients with focal plaque development to examine the impact of local IMT abnormalities on EMT. For a more complete assessment of traditional cardiovascular risk profile, factors such as diabetes, smoking, hypertension and dyslipidemia should be included in future models.
Despite not observing a relationship between EMT and arterial stiffness, we cannot rule out the potential for EMT to predict CVD risk, as our study was not designed to assess the contribution of EMT to CVD risk assessment. Specifically, EMT and a novel combined index of BMI, IMT and epicardial fat thickness (PATIMA) were predictive for CAD in a moderate sample of 422 patients.41 Although a recent study demonstrated a lack of association between EMT and cardiovascular events in high-risk adults,42 longitudinal prospective studies including the measurement of EMT with a combination of traditional CVD risk variables may provide further understanding of the potential for EMT to assess CVD risk and monitor the progression of atherosclerosis.
Conclusion
We found that aging was associated with an increase in EMT in healthy adults, which is not further impacted by the presence of overt cardiovascular disease. EMT was not an independent predictor of measures of aPWV, carotid distensibility or IMT, which may indicate that other factors contribute to EMT thickening with aging and disease. Despite the lack of association between EMT, IMT and arterial stiffness, EMT increases with age and future research should explore the relationship between EMT and the development of cardiovascular disease.
Conflict of interest statement
No competing interests, financial or otherwise, are declared by the authors.
Acknowledgements
This study was supported by funding from the
References
Cite this article
TY - JOUR AU - Hon Lam Choi AU - Jason S. Au AU - Maureen J. MacDonald PY - 2017 DA - 2017/12/22 TI - Carotid extra-media thickness increases with age, but is not related to arterial stiffness in adults JO - Artery Research SP - 13 EP - 19 VL - 21 IS - C SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2017.12.003 DO - 10.1016/j.artres.2017.12.003 ID - Choi2017 ER -
